Abstract
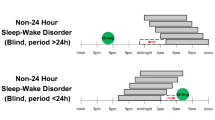
Non-24-hour sleep/wake rhythm disorder (non-24) most commonly presents in totally blind individuals and results from the loss of synchronization (entrainment) of the hypothalamic circadian pacemaker to the 24-hour day. The etiology of the disorder in the sighted is likely distinct from that in the blind and has yet to be definitively demonstrated. Diagnosis of this disorder is based on the patient’s report of relapsing and remitting symptoms of daytime hypersomnolence and/or nighttime insomnia as well as sleep/wake timing that can drift progressively later or earlier each day as documented by sleep diaries or wrist actigraphy. Both melatonin and the melatonin agonist tasimelteon have been shown to successfully entrain the circadian pacemaker in placebo-controlled trials and thereby treat the disorder. The clinician must carefully consider both the time and dose of melatonin administration to achieve the optimal clinical result. Controlled trials of light or melatonin are lacking in the treatment of non-24 among the sighted, but the use of both may be effective when the patients’ self-selected light/dark schedules are taken into account.
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Similar content being viewed by others
References
Medicine AAoS. International classification of sleep disorders. American Academy of Sleep Medicine: Darien; 2014.
Lucas RJ, Lall GS, Allen AE, Brown TM. How rod, cone, and melanopsin photoreceptors come together to enlighten the mammalian circadian clock. Prog Brain Res. 2012;199:1–18.
Czeisler CA, Kronauer RE, Allan JS, et al. Bright light induction of strong (Type O) resetting of the human circadian pacemaker. Science. 1989;244:1328–33.
Khalsa SB, Jewett ME, Cajochen C, Czeisler CA. A phase-response curve to single bright light pulses in human subjects. J Physiol. 2003;549:945–52.
St Hilaire MA, Gooley JJ, Khalsa SB, Kronauer RE, Czeisler CA, Lockley SW. Human phase response curve to a 1h pulse of bright white light. J Physiol. 2012;590:3035–45.
Duffy JF, Cain SW, Chang AM, et al. Sex difference in the near-24-hour intrinsic period of the human circadian timing system. Proc Natl Acad Sci U S A. 2011;108:15602–8.
Czeisler CA, Duffy JF, Shanahan TL, et al. Stability, precision and near-24-hour period of the human circadian pacemaker. Science. 1999;284:2177–81.
Lewy AJ, Sack RL. The dim light melatonin onset as a marker for circadian phase position. Chronobiol Int. 1989;6:93–102.
Lewy AJ, Cutler NL, Sack RL. The endogenous melatonin profile as a marker for circadian phase position. J Biol Rhythm. 1999;14:227–36.
Klerman EB, Gershengorn HB, Duffy JF, Kronauer RE. Comparisons of the variability of three markers of the human circadian pacemaker. J Biol Rhythm. 2002;17:181–93.
Martin SK, Eastman CI. Sleep logs of young adults with self-selected sleep times predict the dim light melatonin onset. Chronobiol Int. 2002;19:695–707.
Burgess HJ, Eastman CI. The dim light melatonin onset following fixed and free sleep schedules. J Sleep Res. 2005;14:229–37.
Burgess HJ, Fogg LF. Individual differences in the amount and timing of salivary melatonin secretion. PLoS One. 2008;3:e3055.
Emens JS, Yuhas K, Rough J, Kochar N, Peters D, Lewy AJ. Phase angle of entrainment in morning- and evening-types under naturalistic conditions. Chronobiol Int. 2009;26:474–93.
Emens JS, Laurie AL, Songer JB, Lewy AJ. Non-24-hour disorder in blind individuals revisited: variability and the influence of environmental time cues. Sleep. 2013;36:1091–100.
Lockley SW, Skene DJ, Arendt J, Tabandeh H, Bird AC, Defrance R. Relationship between melatonin rhythms and visual loss in the blind. J Clin Endocrinol Metab. 1997;82:3763–70.
Czeisler CA, Shanahan TL, Klerman EB, et al. Suppression of melatonin secretion in some blind patients by exposure to bright light. New Engl J Med. 1995;332:6–11.
Klerman EB, ShanahanTL, Brotman DJ, et al. Photic resetting of the human circadian pacemaker in the absence of conscious vision. J Biol Rhythm. 2002;17:548–55.
LeGates TA, Fernandez DC, Hattar S. Light as a central modulator of circadian rhythms, sleep and affect. Nat Rev Neurosci. 2014;15:443–54.
Emens JS, Brotman DJ, Czeisler CA. Evaluation of the intrinsic period of the circadian pacemaker in a patient with a non-24-hour sleep-wake schedule disorder. Sleep Res. 1994;23:256.
Uchiyama M, Lockley SW. Non-24-hour sleep-wake syndreom in sighted and blind patients. Sleep Med Clin. 2009;4:195–211.
Hayakawa T, Uchiyama M, Kamei Y, et al. Clinical analyses of sighted patients with non-24-hour sleep-wake syndrome: a study of 57 consecutively diagnosed cases. Sleep. 2005;28:945–52.
Kitamura S, Hida A, Enomoto M, et al. Intrinsic circadian period of sighted patients with circadian rhythm sleep disorder, free-running type. Biol Psychiatry. 2013;73:63–9.
Wever R. The circadian system of man: results of experiments under temporal isolation. New York, NY: Springer-Verlag; 1979.
Czeisler CA, Weitzman ED, Moore-Ede MC, Zimmerman JC, Knauer RS. Human sleep: its duration and organization depend on its circadian phase. Science. 1980;210:1264–9.
Wittmann M, Dinich J, Merrow M, Roenneberg T. Social jetlag: misalignment of biological and social time. Chronobiol Int. 2006;23:497–509.
Stothard ER, McHill AW, Depner CM, et al. Circadian entrainment to the natural light-dark cycle across seasons and the weekend. Curr Biol. 2017;27:508–13.
Czeisler CA, Richardson GS, Coleman RM, et al. Chronotherapy: resetting the circadian clocks of patients with delayed sleep phase insomnia. Sleep. 1981;4:1–21.
Sack RL, Lewy AJ, Blood ML, Keith LD, Nakagawa H. Circadian rhythm abnormalities in totally blind people: incidence and clinical significance. J Clin Endocrinol Metab. 1992;75:127–34.
Lockley SW, Dressman MA, Licamele L, et al. Tasimelteon for non-24-hour sleep–wake disorder in totally blind people (SET and RESET): two multicentre, randomised, double-masked, placebo-controlled phase 3 trials. Lancet. 2015;386:1754–64.
Lockley SW, Skene DJ, Butler LJ, Arendt J. Sleep and activity rhythms are related to circadian phase in the blind. Sleep. 1999;22:616–23.
Sack RL, Lewy AJ, Blood ML, Keith LD, Nakagawa H. Circadian rhythm abnormalities in totally blind people: incidence and clinical significance. J Clin Endocrinol Metab. 1992;75:127–34.
Burgess HJ, Wyatt JK, Park M, Fogg LF. Home circadian phase assessments with measures of compliance yield accurate dim light melatonin onsets. Sleep. 2015;38:889–97.
Sack RL, Brandes RW, Kendall AR, Lewy AJ. Entrainment of free-running circadian rhythms by melatonin in blind people. New Engl J Med. 2000;343:1070–7.
Leger D, Guilleminault C, Defrance R, Domont A, Paillard M. Prevalence of sleep/wake disorders in persons with blindness. Clin Sci (Lond). 1999;97:193–9.
Scheer FAJL, Hilton MF, Mantzoros CS, Shea SA. Adverse metabolic and cardiovascular consequences of circadian misalignment. Proc Natl Acad Sci U S A. 2009;106:4453–8.
Ruger M, Scheer FAJL. Effects of circadian disruption on the cardiometabolic system. Rev Endocr Metab Disord. 2009;10:245.
Vogel M, Braungardt T, Meyer W, Schneider W. The effects of shift work on physical and mental health. J Neural Trans. 2012;119:1121–32.
Jagannath A, Peirson SN, Foster RG. Sleep and circadian rhythm disruption in neuropsychiatric illness. Curr Opin Neurobiol. 2013;23:888–94.
Kelleher FC, Rao A, Maguire A. Circadian molecular clocks and cancer. Cancer Lett. 2014;342:9–18.
Lewy AJ, Bauer VK, Ahmed S, et al. The human phase response curve (PRC) to melatonin is about 12 hours out of phase with the PRC to light. Chronobiol Int. 1998;15:71–83.
Burgess HJ, Revell VL, Molina TA, Eastman CI. Human phase response curves to three days of daily melatonin: 0.5 mg versus 3.0 mg. J Clin Endocrinol Metab. 2010;95:3325–31.
Lockley SW, Skene DJ, James K, Thapan K, Wright J, Arendt J. Melatonin administration can entrain the free-running circadian system of blind subjects. J Endocrinol. 2000;164:R1–6.
Hack LM, Lockley SW, Arendt J, Skene DJ. The effects of low-dose 0.5-mg melatonin on the free-running circadian rhythms of blind subjects. J Biol Rhythm. 2003;18:420–9.
Lewy AJ, Bauer VK, Hasler BP, Kendall AR, Pires ML, Sack RL. Capturing the circadian rhythms of free-running blind people with 0.5 mg melatonin. Brain Res. 2001;918:96–100.
Lewy AJ, Hasler BP, Emens JS, Sack RL. Pretreatment circadian period in free-running blind people may predict the phase angle of entrainment to melatonin. Neurosci Lett. 2001;313:158–60.
Lewy AJ, Emens JS, Sack RL, Hasler BP, Bernert RA. Low, but not high, doses of melatonin entrained a free-running blind person with a long circadian period. Chronobiol Int. 2002;19:649–58.
Lewy AJ, Emens JS, Bernert RA, Lefler BJ. Eventual entrainment of the human circadian pacemaker by melatonin is independent of the circadian phase of treatment initiation: clinical implications. J Biol Rhythm. 2004;19:68–75.
Lewy AJ, Emens JS, Lefler BJ, Yuhas K, Jackman AR. Melatonin entrains free-running blind people according to a physiological dose-response curve. Chronobiol Int. 2005;22:1093–106.
Auger RR, Burgess HJ, Emens JS, Deriy LV, Thomas SM, Sharkey KM. Clinical practice guideline for the treatment of intrinsic circadian rhythm sleep-wake disorders: advanced sleep-wake phase disorder (ASWPD), delayed sleep-wake phase disorder (DSWPD), non-24-hour sleep-wake rhythm disorder (N24SWD), and irregular sleep-wake rhythm disorder (ISWRD). An update for 2015. J Clin Sleep Med. 2015;11:1199–236.
Emens J, Lewy AJ, Yuhas K, Jackman AR, Johnson KP. Melatonin entrains free-running blind individuals with circadian periods less than 24 hours. Sleep. 2006;29:A62.
Eastman CI, Anagnopoulus CA, Cartwright RD. Can bright light entrain a free-runner? Sleep Res. 1988;17:372.
Hoban TM, Sack RL, Lewy AJ, Miller LS, Singer CM. Entrainment of a free-running human with bright light? Chronobiol Int. 1989;6:347–53.
Hayakawa T, Kamei Y, Urata J, et al. Trials of bright light exposure and melatonin administration in a patient with non-24 hour sleep-wake syndrome. Psychiatry Clin Neurosci. 1998;52:261–2.
Watanabe T, Kajimura N, Kato M, Sekimoto M, Hori T, Takahashi K. Case of a non-24 h sleep-wake syndrome patient improved by phototherapy. Psychiatry Clin Neurosci. 2000;54:369–70.
McArthur AJ, Lewy AJ, Sack RL. Non-24-hour sleep-wake syndrome in a sighted man: circadian rhythm studies and efficacy of melatonin treatment. Sleep. 1996;19:544–53.
Kamei Y, Hayakawa T, Jujiro U, et al. Melatonin treatment for circadian rhythm sleep disorders. Psychiatry Clin Neurosci. 2000;54:381–2.
Watanabe A, Hirose M, Arakawa C, Iwata N, Kitajima T. A case of non-24-hour sleep-wake rhythm disorder treated with a low dose of ramelteon and behavioral education. J Clin Sleep Med. 2018;14:1265–7.
Zeitzer JM, Dijk DJ, Kronauer RE, Brown EN, Czeisler CA. Sensitivity of the human circadian pacemaker to nocturnal light: melatonin phase resetting and suppression. J Physiol. 2000;526:695–702.
Chang AM, Scheer FAJL, Czeisler CA. The human circadian system adapts to prior photic history. J Physiol. 2011;589:1095–102.
Czeisler CA, Boivin DB, Duffey JF, Kronauer RE. Dose-response relationships for resetting of human circadian clock by light. Nature. 1996;379:540–1.
Gronfier C, Wright KP Jr, Kronauer RE, Jewett ME, Czeisler CA. Efficacy of a single sequence of intermittent bright light pulses for delaying circadian phase in humans. Am J Physiol Endocrinol Metab. 2004;287:E174–81.
Najjar RP, Zeitzer JM. Temporal integration of light flashes by the human circadian system. The J Clin Invest. 2016;126:938–47.
Rahman SA, St Hilaire MA, Chang AM, et al. Circadian phase resetting by a single short-duration light exposure. JCI Insight. 2017;2:e89494.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 The Author(s)
About this chapter
Cite this chapter
Emens, J. (2020). Non-24-Hour Sleep-Wake Rhythm Disorder. In: Auger, R. (eds) Circadian Rhythm Sleep-Wake Disorders. Springer, Cham. https://doi.org/10.1007/978-3-030-43803-6_9
Download citation
DOI: https://doi.org/10.1007/978-3-030-43803-6_9
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-43802-9
Online ISBN: 978-3-030-43803-6
eBook Packages: MedicineMedicine (R0)