Abstract
The use of antibiotics in animal agriculture is steadily increasing, especially in developing countries. The European Union and a handful of developed countries have implemented policies to scale back the use of antibiotics, recognizing its role in the global rise of antibiotic resistance. But many farmers who raise animals live in poor countries without public health regulations, or work for large corporate entities that can move their operations to places with weak regulations. To minimize the careless use of antibiotics around the world, we need multi-lateral coordination between states on some common standards for the use of antibiotics in animals.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
Keywords
The use of antibiotics in animal agriculture is steadily increasing, especially in developing countries. The European Union and a handful of developed countries have implemented policies to scale back the use of antibiotics, recognizing its role in the global rise of antibiotic resistance. But many farmers who raise animals live in poor countries without public healthregulations, or work for large corporate entities that can move their operations to places with weak regulations. To minimize the careless use of antibiotics around the world, we need multi-lateral coordination between states on some common standards for the use of antibiotics in animals.
1 Introduction
Imagine a world in which every time you tied your shoes, you contributed to a process that resulted in the unintended suffering and death of thousands of people you’ll never know.Footnote 1 In this world, like ours, shoelaces are useful: they save time, are a little cheaper than using Velcro ties, and more convenient than wearing slip-on shoes. But when everyone ties their shoes, lots of people die, and many more suffer.
This is a strange world to imagine, but it is a lot like the world we live in. The culprit isn’t tying shoelaces, of course, but consuming factory farmed meat. Factory farms are wicked places – one of the last bastions of legally sanctioned cruelty toward animals. But more than this, they are bad for human health.
Some antibiotics are given to cattle and pigs to marginally speed up their growth. The biological mechanisms through which antibiotics promote growth aren’t well understood, but the use of antibiotics to promote growth does seem to work. More importantly, raising animals in densely packed conditions requires a steady dose of antibiotics to prevent infections that would otherwise run rampant.
Like many practices, there are benefits as well as costs: meat from factory farms is cheaper than meat from farms with free-range animals, often about half the price. This is partly because factory farms allow animals to occupy less space, which makes their production cheaper, and this savings is passed on to consumers.
Apart from its obvious benefits, factory farming produces many costs (Anomaly 2015). In this essay, I will focus on the threat that our use of antibiotics in animal agriculture poses for human health. Contrary to popular opinion, the problem is not that antibiotics are passed along from animals to people who eat them, and that this is bad for our health. Instead, the problem is that the more antibiotics we give to livestock, the more we encourage the emergence and spread of antibiotic-resistant bacteria in a microbial environment shared by animals and people (Marshall and Levy 2011; Spellberg et al. 2016).
Like all eukaryotic organisms, people pay a high price for sex: each child only shares half of her genes with each parent. But sexual reproduction seems to confer benefits by increasing variation in the immune system children inherit, thus making it more likely that some of them will survive the onslaught of parasites that continually evolve novel ways of exploiting their hosts (Hamilton et al. 1990). As strange as sex is – each of two independent organisms swapping their genes to create a hybrid – the bacterial equivalent is even kinkier than a San Francisco night club. Bacteria reproduce by cloning themselves, but they evolve throughout their lives by promiscuously swapping genes with other bacteria and by extracting genes from the viruses that parasitize them. This allows them to adapt to new environments quickly: in a lethal environment, a small number of bacteria are likely to have some advantage over the trillions that die. And this advantage comes either from a random genetic mutation, or from the lateral transfer of genes from one bacterium to another.
Some genes allow bacteria to fend off the antibiotics that plants, animals, and other bacteria use to destroy them. Many of these naturally occurring antibiotics have existed for billions of years, as part of an unending evolutionary arms race between host and parasite. Like their naturally occurring cousins, synthetic antibiotics made in a lab usually involve penetrating a bacterial cell wall and disrupting DNA synthesis, or otherwise slowing or stopping bacterial reproduction.
All a bacterium needs to survive an antibiotic is some way to either block the penetration of the chemical with a thick cell wall, degrade it with enzymes, or pump it out if it penetrates its body. Once that happens, it’s off to the races. The lucky bacterium multiplies rapidly and spreads its resistance to other bacteria. When new resistant strains of bacteria emerge in animal agriculture, they are passed along to farmers who work with animals, workers who slaughter animals, consumers who eat meat, and people in our more general microbial environment (Laxminarayan et al. 2016).
The average person hosts about 40 trillion bacteria at any given time, and we constantly swap bacteria with each other and with the environment around us (Sender et al. 2016). So even though the overuse of antibiotics tends to affect those closest to the source of resistant bacteria – whether animals or people – over time, strains of bacteria that are resistant to antibiotics can spread through trade and travel among people, and through soil and streams around factory farms. And while reducing the use of antibiotics does tend to reduce resistance, the decline of resistance does not happen immediately, since reservoirs of antibiotic-resistant genes tend to persist in bacterial plasmids for a long time (Andersson and Hughes 2010).
For more than a decade the European Union has banned antibiotics for growth promotion in farm animals, and tried to impose standards that increase animal welfare and reduce the need to use antibiotics. The US has begun to follow suit, driven by consumer demand for antibiotic-free meat, and FDA threats of regulation. But most developing countries are moving in the opposite direction, with explosive growth of antibiotic use in both people and animals in China, India, Pakistan, Egypt, and many sub-Saharan African countries (Van Boeckel et al. 2015).
2 Economic Models
The problem of antibiotic resistance is often framed by well-known economic models like the prisoner’s dilemma, the tragedy of the commons, or the provision of public goods. All three models are useful in some contexts, but when they are not adequately qualified they can cast shade rather than light on the problem of resistance.
2.1 Prisoner’s Dilemma
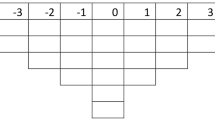
Consider first the prisoner’s dilemma (PD). In the original example, we are presented with two prisoners who are suspected of armed robbery, but a District Attorney (DA) who only has enough evidence to prosecute them for the illegal possession of firearms. The prisoners are in separate jail cells, and the DA offers each of them a deal: if you snitch on your accomplice and he stays silent, you’ll get off scot free and he’ll be executed. If you both stay silent, you’ll each get one year in prison. If you both snitch, you’ll each get a decade in prison. The payoffs are as follows:
Odin | Loki | |
Silence | Snitch | |
Silence | 1 year/1 year | Death/Freedom |
Snitch | Freedom/Death | 10 years/10 years |
If the accomplices lack friendly feelings for one another, and if neither fears reprisals outside of prison, the rational move for each is to snitch, even if the socially optimal move is for both to stay silent. The PD is interesting because each player acting rationally produces an outcome that is worse for everyone.
The PD is a simple model that is frequently invoked to explain why rational agents act in ways that contribute to air pollution or species extinction even when each person would prefer to breath clean air or preserve biodiversity. Although most of the real-world games the PD is used to illustrate are complicated by the fact that there are more than two players, that players have asymmetric information or poorly formed preferences, and that they face uncertainty about whether (or how many times) the game will be repeated, the simplistic two player model is still of some use in visualizing problems like antibiotic resistance.
Consider the following case. Each carnivore faces the choice to consume meat from factory farmed animals or humanely raised animals free from antibiotics.
Odin | Loki | |
Humanely raised | Factory farmed | |
Humanely raised | 2nd/2nd | 4th/1st |
Factory farmed | 1st/4th | 3rd/3rd |
The payoff matrix indicates that each person does best by consuming factory farmed meat, that each does worst by consuming humanely raised meat (if the other does not), but that they both do better if they both consume meat from humanely raised rather than factory farmed animals. In the real world, if there were only two consumers and two producers, the effects of Loki’s consumption choices would not be big enough to adversely affect Odin’s welfare. But when we generalize to hundreds of millions of people, we get a case in which each person marginally increases the probability of antibiotic-resistant bacteria emerging and spreading, but each also saves a bit of money by consuming meat from factory farmed animals. As long as the benefit to each from buying factory farmed meat exceeds the costs associated with the alternative, the model predicts they will continue their socially suboptimal behavior.
There are several limitations of extending a two-person model to a many-person case. First, in the large number case we can treat other people’s actions as given, whereas in the small number case we might change their behavior by reasoning with them (Bowles and Gintis 2013). Second, in the large number case we may have to resort to using state power to incentivize socially optimal behavior, whereas in the small number case people are in a better position to create local solutions that exploit social norms and informal punishments to move from the Nash equilibrium to the Pareto optimum (Ostrom 2000).
Similar considerations apply to farmers choosing whether to raise their animals with or without antibiotics, which is a many-person prisoner’s dilemma in which most people reason parametrically (taking other’s actions as more-or-less given). While there is a growing market for antibiotic-free meat, so that some farmers find it profitable to reject factory farming, most consumers around the world either don’t know enough or care enough about the problem to entice farmers to reject antibiotics and raise their animals humanely.
2.2 Tragedy of the Commons
Many have argued that our aggregate use of antibiotics – in hospital settings and animal agriculture – is analogous to the misuse of commonly owned resources. In the classic example of a commons tragedy, farmers lack private property rights and are forced to raise animals on a common plot of land. The farmers internalize the benefits from raising animals and selling their meat, but share the costs of grass and soil depletion. Consequently, in the absence of sufficient altruistic restraint, each farmer continues to add animals to the commons up to the point at which the personal benefits equal the personal costs. To the extent that they ignore social costs, farmers add animals even if it makes everyone worse off than they would be if they agreed to a set of enforceable constraints.
Assume, for example, that above some number for each animal added to a common pasture, each farmer will get 10 utility points but the community will lose 20 utility points as the grass becomes overgrazed. If there are 10 farmers, each nets 8 utility points from adding another animal (+10 from selling the meat and − 2 from depleting grass and soil), and so they add animals until the commons is ruined. The typical solution to commons tragedies is to privatize plots of land, or (less efficiently) to set up enforceable limits with penalties for exceeding the limits. In small settings, these standards can be enforced by the court of public opinion, assuming farmers care about their reputation in the community. In large settings, standards are usually set by the state, and enforced with penalties for violating laws, or taxes and subsidies that attempt to bring about a socially optimal use of common resources.
Is the use of antibiotics on factory farms a commons tragedy? Some suggest that it is (Hollis and Maybarduk 2015). Others are more cautious, arguing that it depends on assumptions that include how quickly alternative antibiotics and vaccines will be developed, and how accurately we can diagnose infections (McAdams 2017a). Just as there is no such thing as a precise carrying capacity for land (since we can develop chemical fertilizers to increase soil productivity, or genetically engineer animals to more efficiently turn grass into meat), so too there is no specific point at which using more antibiotics necessarily imposes net costs on people.
As with the Prisoner’s Dilemma, the commons tragedy model can help us conceptualize the incentives that generate the problem of antibiotic resistance. But it can also be misleading. For example, suppose we develop better diagnostics. Rapid diagnostic tests can make broad-spectrum antibiotics last longer by helping us identify the specific kind of infection plaguing a person or animal so that we can treat it with a narrow-spectrum antibiotic agent (McAdams 2017a). When better diagnostics are available to guide treatment in conjunction with extremely narrow-spectrum agents, David McAdams argues that “greater antibiotic use can in some cases decrease the selective pressure favoring resistant bacteria” (2017a, p. 6). Better diagnostics may also make it more profitable for companies to manufacture and conserve antibiotics if it leads physicians and farmers to more carefully use antibiotics to target specific infections (2017b). Using the wrong antibiotic often fails to treat the relevant infection, and it encourages resistance among all bacteria that the antibiotic affects. Using broad-spectrum antibiotics without a specific diagnosis is like carpet-bombing an entire city in order to kill a few soldiers. To the extent that we can target our enemies with precision strikes, there is less opportunity for collateral damage in the form of resistant strains of bacteria that grow in number as their susceptible compatriots are killed.
In addition to rapid diagnostic tests, the invention of “adjuvants” (supplements that make antibiotics more effective by priming our immune system, or by blocking bacterial resistance) can extend the life of antibiotics (Wright 2016). Rapid diagnostics and effective adjuvants show that the collective consumption of antibiotics does not automatically create a commons tragedy. It all depends on how we use antibiotics, and this is in part a function of technology, and the incentives that physicians and farmers face as a result of public policies.
Nevertheless, the careless way in which antibiotics are currently used in animal agriculture outside of Europe probably is a commons tragedy. This is because farmers in most countries today simply ignore the social cost of using antibiotics in livestock, and many farmers fail to understand how using antibiotics in agriculture can lead to the rise of bacterial infections in people that are increasingly expensive, difficult, or impossible to treat.
2.3 Public Goods
A final model frequently used to describe problems associated with our use of antibiotics requires us to make a distinction. In economics, private goods are those that are consumed by individuals in ways that don’t involve significant externalities (costs or benefits borne by people external to an economic transaction). For example, when I buy a private good like a cup of coffee or a pair of eyeglasses, the costs or benefits imposed on other people are trivial. Publicgoods, by contrast, are consumed in common, so that we share the benefits of consumption. Public goods can be thought of as non-excludable positive externalities (Cowen 2008), though this is misleading in cases where the public good is experienced as a cost rather than a benefit to those who consume it.
Antibiotics themselves are not public goods, but to some extent the efficacy of antibiotics, and efforts made to move us toward the socially optimal use of antibiotics, are public goods. Similarly, efforts to eliminate infectious diseases are public goods (Selgelid 2007), since the reduction or eradication of a disease is shared by all people in a region, and potentially all people on the planet. By extension, reducing the reckless use of antibiotics in agriculture is a public good. Although alternative agricultural methods are more expensive, the enormous external costs of drug-resistant diseases that emerge from factory farming almost certainly exceed the benefits of cheaper meat (O’Neill et al. 2015).Footnote 2
Many people, including some economists, equate public goods problems with commons tragedies and prisoner’s dilemmas. This is a mistake, although it is understandable since many commons tragedies and public goods problems can be usefully modeled by the prisoner’s dilemma. But often public goods are better described as assurance games or coordination games (Hampton 1987), and this is good news for lawmakers and farming associations who are aware of the problem and want to converge on common standards that allow them to make a profit and minimize the risk of antibiotic resistance. One problem with preserving global public goods like the efficacy of antibiotics is that most people are unaware of the problem, since each plays a very small role in producing it. In other words, many people who might help preserve or produce public goods are rationally ignorant about the nature of the problem.
3 Moral Principles
Ignorance of how the use of antibiotics in agriculture harms human health is rational in the economic sense, but it is not necessarily morally excusable (Anomaly 2015). Since the problem of AMR is difficult to understand, and since each act of consuming factory-farmed products contributes only imperceptibly to the problem, it makes perfect sense that consumers would ignore the problem and purchase cheap factory-farmed meat, rather than more expensive meat from farms that don’t use antibiotics.
But the fact that we can explain consumer ignorance does not absolve consumers of responsibility for contributing to the problem. As information about the private benefits and social costs of using antibiotics in farm animals becomes more widely available, consumers have an increasing responsibility to act on it by changing their purchasing habits and trying to persuade governments to make it harder to purchase meat from animals unnecessarily dosed with antibiotics. Alexander Fleming famously warned that “the thoughtless person playing with penicillin is morally responsible for the death of the man who finally succumbs to infection with the penicillin-resistant organism.”Footnote 3 One form of “playing with penicillin” is the use of it as a growth promoter on factory farms, or the more common use of it to prevent infections in the cramped and cruel conditions that characterize factory farms.
A more nuanced version of Fleming’s admonition requires us to distinguish actual harms to discrete people from probabilistic harms to actual or potential people. Another way to put the point is to say that the harms of antibiotic resistance are “identity-independent” in the sense that the victims of AMR cannot be known ahead of time and, in some cases, are not yet born. While a single farmer (or consumer) misusing antibiotics can create or encourage a resistant strain that spreads to other people, generally the prevalence of resistant bacteria in the environment depends on how all of us act. By acting in ways that create genetic pollution in our microbial environment, we make it a little more likely that someone will suffer or die of a previously treatable infection.
Many other pollution problems are structurally similar to antibiotic resistance. For example, each of us drives to work and produces the social costs of pollution and traffic congestion as a byproduct, while experiencing the private benefit of an enjoyable ride in our own car. There are also social benefits when each person drives, if driving contributes to a more efficient workforce that creates better goods at lower cost. Suppose the social costs of air pollution and traffic congestion exceed the individual benefits of driving. A common response is to impose a price on driving by taxing fuel or charging user fees to encourage the efficient use of roads and the atmosphere. The underlying moral principles are that we should pay in proportion to the amount we contribute to the problem, and that if anyone’s liberties to pollute are restricted, then all us should face the same restrictions (Gaus 1999, p. 197).
Similar arguments have been made for taxing antibiotics in medicine and agriculture to discourage low-value use (Kades 2005; Anomaly 2013). But antibiotic resistance is much more complicated than air pollution or traffic congestion: in some cases we may want to subsidize rather than tax the use of antibiotics when people who can’t afford them are likely to spread infectious diseases to others (Selgelid 2007). Apart from taxes and subsidies, there is a vast literature on how to harness intellectual property rights, prescription requirements, basic science research funding, and shared surveillance to control the problem (O’Neill et al. 2016).
What I now want to argue is that without more coordination between states, the problem of antibiotic resistance in agriculture will likely get worse, with dire consequences for human health in the coming century.
4 Global Coordination
The provision of global public goods like conserving antibiotics and reducing infectious disease raises two problems: the free rider problem occurs when individual consumers, farmers, or states seek the gains of limited antibiotic use without paying the costs; the assurance problem occurs when each is willing to pay the cost of reducing unnecessary use, but lacks the assurance that others will abide by policies that constrain our collective use of antibiotics.
The first problem is difficult to overcome to the extent that self-interest dominates the actions of farmers in a market or of politicians in a government. But there is some evidence that most consumers who understand the problem are willing to pay higher prices for meat from animals not given antibiotics (Spellberg et al. 2016). Moreover, if people really understood the problems factory farms create they would likely be willing to pay significantly more for meat, since most people support taxes (or costly regulations) when they are reasonably sure the tax will be used to discourage the problems associated with pollution (Kallbekken et al. 2011).
Agricultural producers are also likely to be willing to comply with standards that limit antibiotic use provided other firms are also forced to internalize the cost of similar regulations or taxes. The fact that the assurance problem is often more serious than the free rider problem in trying to elicit cooperation in many public goods games (Bowles and Gintis 2013) is good news for those who worry about the feasibility of states setting mutually beneficial standards.
Part of the problem with antibiotics in agriculture is that as transportation costs decline, the market for animal meat becomes increasingly global: animal feed is produced in one country, animals are raised in another, and then meat is exported to a third country. Since producers in many countries are now in a position to operate industrial animal farms, unless all states set standards that limit antibiotic use, producers will tend to migrate to countries with the weakest regulations. There is already some evidence that this “race to the bottom” is happening as Chinese farms are producing meat in factory farms that use more confinement and antibiotics than farms in other countries. In fact, just as the US is beginning to move away from factory farming due to consumer demand and threats of regulation by the US Food and Drug Administration, many of the most populous developing countries – including China, India, and Brazil – are embracing factory farming (O’Neill et al. 2015).
A well-designed trade treaty between major exporters and importers of meat should recognize the problem of “leakage,” which occurs when one country sets relatively high environmental standards, and allows other countries with weaker standards to increase the production of similar goods in ways that simply changes where the pollution is emitted (Barrett 1999). In other words, any treaty worth implementing cannot reward free-riding countries whose firms are permitted to externalize the costs of their production, while firms in other countries internalize the costs of complying with policies that would make everyone better off if countries complied with them.
A second feature of an effective treaty to limit antibiotics in agriculture is a minimum participation clause to assure prospective signatories that unless a sufficient number of nations sign on, they will not be forced to pay additional production costs (Barrett 1999). This feature solves the assurance problem for firms and nations that are willing to comply with stricter production practices provided enough others do to produce the global benefits associated with restricting antibiotic use.
A third feature of any multi-lateral agreement to restrict antibiotic use is that it would need to be flexible enough to allow countries to achieve collective goals in different ways. For example, some experts advocate setting targets for the per capita quantity of antibiotics that can be administered to animals. According to the British Review on Antimicrobial Resistance, pork producers in Denmark (the first country to ban antibiotics as growth promoters) use about 50 mg of antibiotics per kg of livestock in the country (O’Neill et al. 2015, p. 2).
A flexible treaty would take something like this number as a benchmark that all countries must meet, but it would allow countries to achieve the relevant goal in different ways: by taxing antibiotics, placing a cap on total use, restricting antibiotics by requiring veterinary oversight, or some combination of these policies. Antibiotics deemed especially important for human use should probably be banned for use in agriculture by all countries. But what often matters is the quantity of antibiotics used, not just the kind. This is especially true because plasmids that confer antibiotic resistance can be transferred between bacteria of different species, and can reduce the efficacy of different drugs than those administered by farmers (Marshall and Levy 2011).
One advantage of imposing “pollution taxes” or user fees on antibiotics in agriculture is that, unlike regulations, governments have strong incentives to enforce them. Governments can use the revenue raised from taxes to finance vaccination programs that minimize the need to administer antibiotics. They might also fund basic science research that aims to develop new vaccines and diagnostics for infectious diseases, and to develop entirely new treatments like genetically engineered bacteriophage viruses (Bikard et al. 2014).
Taxing socially costly activities like using antibiotics in agriculture also incentivizes farmers to find alternative ways to produce meat that minimize antibiotic resistance. These alternatives may include increasing the roaming space animals have, and decreasing the stress they face when forced to live in extreme confinement. A more promising alternative is to create “in vitro meat” made in a lab from embryonic stem cells. This would avoid the need to raise animals at all, thus reducing untold amounts of suffering and potential public health problems.
Finally, any agreement to restrict antibiotic use should be attractive enough for each participating country to be willing to enforce it. It is likely that offering benefits for compliance will be more effective than simply threats of sanctions for non-compliance. For example, it is in the interest of all nations that each nation monitors the outbreak and spread of infectious diseases, as well as novel patterns of antibiotic resistance. But sometimes only wealthier states have the budgets and technology to accomplish this. By sharing information and technology with developing countries, wealthier countries can both signal goodwill and deliver tangible benefits to other countries they wish to comply with stricter controls on antibiotic use. This may act as a positive incentive for poor countries to do their part, even if the threat of sanctions for non-compliance with collectively beneficial restrictions is also important.
Each nation faces its own challenges, including an electorate that is unlikely to fully understand the social benefits and costs of antibiotics, and factory farmers who are unlikely to welcome regulations that impose new costs on them. Governments can justify spending some money to ease the transition from factory farming techniques to alternatives that produce better consequences for the same reason they can justify compensating taxi cab drivers who were required to buy a costly permit from the state to drive a taxi, but who are now forced to compete with companies like Uber, whose drivers did not have to pay for the right to operate as a taxi service. In fact, if relatively wealthy governments offer temporary assistance to domestic firms to transition away from factory farming, and to relatively poor governments to comply with new restrictions, the move away from the reckless use of antibiotics may be easier to induce, and more fair from the standpoint of global distributive justice.
Notes
- 1.
Parts of the introduction are reprinted from an article that first appeared in Compass, the annual magazine of the Kenan Institute for Ethics at Duke University (2017).
- 2.
It may be that some use of antibiotics in agriculture is both individually beneficial for animals (who contract infections despite humane and prudent farming practices), and socially beneficial for people (who may be less likely to contract a bacterial infection an animal has). But the growing quantity of antibiotics used in farming today is likely to produce harms that far exceed these benefits.
- 3.
References
Andersson, Dan, and Diarmaid Hughes. 2010. Antibiotic resistance and its cost: Is it possible to reverse resistance? Nature 8: 260–271.
Anomaly, Jonathan. 2013. Collective action and individual choice. Journal of Medical Ethics 39: 752–756.
———. 2015. What’s wrong with factory farming? Public Health Ethics 8 (3): 246–254.
Barrett, Scott. 1999. Montreal vs Kyoto. In Global public goods: International cooperation for the 21st century, ed. Inge Kaul et al. Oxford: Oxford University Press.
Bikard, David, et al. 2014. Exploiting CRISPR-Cas nucleases to produce sequence-specific antimicrobials. Nature Biotechnology 32: 1146–1150.
Bowles, Samuel, and Herbert Gintis. 2013. A cooperative species: Human reciprocity and its evolution. Princeton: Princeton University Press.
Cowen, Tyler. 2008. Public goods. The concise encyclopedia of economics. 2nd ed. http://www.econlib.org/library/Enc/PublicGoods.html.
Gaus, Gerald. 1999. Social philosophy. London: M.E. Sharpe Publishing.
Hamilton, William, et al. 1990. Sexual reproduction as an adaptation to resist parasites. Proceedings of the National Academy of Science 87: 3566–3573.
Hampton, Jean. 1987. Free rider problems in the production of collective goods. Economics and Philosophy 3: 245–273.
Hollis, Aidan, and Peter Maybarduk. 2015. Antibiotic resistance is a tragedy of the commons that necessitates global cooperation. Journal of Law, Medicine, and Ethics 43: 33–37.
Kades, Eric. 2005. Preserving a precious resource: Rationalizing the use of antibiotics. Northwest University Law Review 99: 611–675.
Kallbekken, Steffen, et al. 2011. Do you not like Pigou, or do you not understand him? Journal of Environmental Economics and Management 62 (1): 53–64.
Laxminarayan, Ramanan, et al. 2016. Antibiotic use and resistance in food animals. The Center for Disease Dynamics, Economics, and Policy.https://cddep.org/sites/default/files/india_abx_report.pdf. Accessed 1 May 2017.
Marshall, Bonnie, and Stuart Levy. 2011. Food animals and antimicrobials: Impacts on human health. Clinical Microbiology Reviews 24 (4): 718–733.
McAdams, David. 2017a. Resistance diagnosis and the changing epidemiology of antibiotic resistance. New York Academy of Sciences. 1388 (2017): 5–17.
———. 2017b. Resistance diagnosis and the changing economics of antibiotic discovery. New York Academy of Sciences. 1388 (2017): 18–25.
O’Neill, Jim, et al. 2015. Antimicrobials in agriculture and the environment: Reducing unnecessary use and waste. The Review on Antimicrobial Resistance. http://amr-review.org/.
———. 2016. Tackling drug-resistant infections globally: Final report and recommendations. The Review on Antimicrobial Resistance. http://amr-review.org/.
Ostrom, Elinor. 2000. Collective action and the evolution of social norms. Journal of Economic Perspectives 14 (3): 137–158.
Selgelid, Michael. 2007. Ethics and drug resistance. Bioethics 21 (4): 218–229.
Sender, Ron, et al. 2016, August 19. Revised estimates for the number of human and bacterial cells in the body. PLOS Biology. https://doi.org/10.1371/journal.pbio.1002533.
Spellberg, Brad, et al. 2016. Antibiotic resistance in humans and animals. Discussion paper for the National Academy of Medicine. Accessed May 2017. http://www.nam.edu/antibiotic-resistance-in-humans-and-animals.
Van Boeckel, T.P., et al. 2015. Global trends in antimicrobial use in food animals. Proceedings of the National Academy of Sciences 112 (18): 5649–5654.
Wright, Gerard. 2016. Antibiotic adjuvants: Rescuing antibiotics from resistance. Trends in Microbiology 24 (11): 862–871.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Open Access This chapter is licensed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence and indicate if changes were made. The images or other third party material in this chapter are included in the chapter’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the chapter’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Copyright information
© 2020 The Author(s)
About this chapter
Cite this chapter
Anomaly, J. (2020). Antibiotics and Animal Agriculture: The Need for Global Collective Action. In: Jamrozik, E., Selgelid, M. (eds) Ethics and Drug Resistance: Collective Responsibility for Global Public Health. Public Health Ethics Analysis, vol 5. Springer, Cham. https://doi.org/10.1007/978-3-030-27874-8_18
Download citation
DOI: https://doi.org/10.1007/978-3-030-27874-8_18
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-27873-1
Online ISBN: 978-3-030-27874-8
eBook Packages: Religion and PhilosophyPhilosophy and Religion (R0)