Abstract
Although total knee arthroplasty (TKA) is considered to be a cost-effective intervention, most patients do not experience natural joints, and it is reported that up to 20% of them are dissatisfied [1, 2]. A systematic review of gait analysis after TKA indicates that patients display significant kinematic differences from normal controls [3]. Due to the significant deficiencies in both our knowledge and technology in the past, we were far from replicating normal knee kinematics with TKA. These limitations in TKA function and patient satisfaction should stimulate us to restart the entire development process. Enhancements in our understanding of knee anatomy and biomechanics may suggest ways of improving TKA outcomes. Implant design needs to be advanced to reproduce the anatomy and kinematics of native knees. More precise surgical techniques with navigation, patient-matched instrumentation and robotics need to be further refined. The future of TKA is to produce more natural knee joints, with resultant improved patient satisfaction and ultimately a forgotten joint.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
-
After five decades of knee joint replacement development, we still do not reliably provide a forgotten knee joint to our patients.
-
A better understanding of human anatomy will help to define the surgical goal during prosthetic implantation.
-
Precise surgical tools like computer navigation, personalized instruments or robotics will be valuable to achieve each patient’s individualised target.
-
More anatomic surgical procedures and implants may better reproduce native joint kinematics.
-
Improving perioperative care and reducing adverse events will remain major factors for success in knee joint replacement.
-
The future of knee joint replacement relies on our capacity to restore patient-specific knee anatomy and function.
1 Introduction
Although total knee arthroplasty (TKA) is considered to be a cost-effective intervention, most patients do not experience natural joints, and it is reported that up to 20% of them are dissatisfied [1, 2]. A systematic review of gait analysis after TKA indicates that patients display significant kinematic differences from normal controls [3]. Due to the significant deficiencies in both our knowledge and technology in the past, we were far from replicating normal knee kinematics with TKA. These limitations in TKA function and patient satisfaction should stimulate us to restart the entire development process. Enhancements in our understanding of knee anatomy and biomechanics may suggest ways of improving TKA outcomes. Implant design needs to be advanced to reproduce the anatomy and kinematics of native knees. More precise surgical techniques with navigation, patient-matched instrumentation and robotics need to be further refined. The future of TKA is to produce more natural knee joints, with resultant improved patient satisfaction and ultimately a forgotten joint.
2 Historical Perspectives
The anatomy of the knee and its kinematics are complex and remain poorly understood. The normal anatomy varies widely, and pathological changes increase its variability further [4,5,6]. Instrument precision was poor, and implantation errors were frequent when TKA surgery was introduced in the 1970s [7]. The focus was therefore on implant survivorship rather than reproducing normal knee anatomy and function. To simplify operations, surgeons selected neutral femoral and tibial cuts to create rectangular flexion and extension gaps and a neutral mechanical axis. Individual patient anatomy was not reproduced, with the focus on standardisation of the procedure. Bony anatomy modifications created by mechanical alignment are linked to mediolateral and flexion-extension joint gap imbalances [8]. Multiple soft tissue release techniques were developed to force the patient’s soft tissues to adjust to the non-anatomical bone cuts.
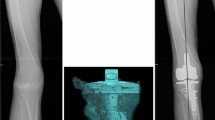
There is a very large variation in the anatomy of the knee across individuals. The precise restoration of this anatomy during total knee arthroplasty (TKA) may improve knee stability, kinematics and clinical function. The future of TKA should therefore look to restore individual anatomy with a personalized joint replacement. Currently, there is a developing interest in new methods of alignment for TKA. In the future, this is likely to expand with a move away from traditional mechanical alignment to an individualised or kinematic alignment [9] (Fig. 15.1). In Chaps. 24, 25 and 26, a detailed description of these alignment philosophies are discussed. The authors feel a restricted kinematic alignment protocol offers the advantages of the restoration of the patient’s constitutional limb anatomy but within a safe margin, which avoids reproducing the extreme pathologies that may result in early failure.
Conventional TKA instrumentation restricts the surgeon to standardised alignment, so new techniques and technologies are required to allow a patient-specific alignment.
3 Precision Technologies
Greater precision in surgery is now possible due to newer techniques using computer navigation, patient-specific instrumentation (PSI) and robotics. These technologies allow the surgeon to individualise the alignment of the knee replacement to replicate individual anatomy. Further study and refinement of these technologies will determine which will be the best to use going forward.
There is an abundance of evidence that computer navigation produces better precision than conventional instrumentation [10] but only limited evidence that this translates into better clinical outcomes [11]. The use of robotics in orthopaedic surgery is much more recent, so there is little evidence of efficacy in the literature at present. One benefit of PSI is standardisation of the procedure with all the planning done preoperatively, compared to computer navigation or robotic surgery where the planning is done at the time of surgery. This may lead to shorter operating times.
There is no doubt that greater accuracy in surgery is an important goal. Perhaps the reason why this greater accuracy has not always resulted in better clinical outcomes [12] is that we were aiming for the wrong target (Fig. 15.2). Accurately achieving a neutral HKA is of limited value if such implant orientation is not linked with improved patient satisfaction. With a new target in mind, being a personalized alignment goal for each patient, improved precision may reveal its value.
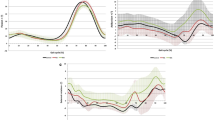
In a recent study, we compared the parameters of kinematics during gait of 36 TKA (single radius, CR) implanted using computer navigation with either kinematic alignment or mechanical alignment technique, with a group of 170 healthy controls [13]. Eighteen kinematically aligned TKAs were matched by gender and age to 18 mechanically aligned TKAs. Knee kinematics were assessed with the Knee KG™ (Emovi, Laval, Canada) frame and software (Fig. 15.3). The kinematic alignment group showed no significant knee kinematic differences compared to healthy knees in sagittal plane range of motion, maximum flexion, abduction-adduction curves or knee external tibial rotation. Conversely, the mechanical alignment group displayed several significant knee kinematic differences to the healthy group: less sagittal plane range of motion (49.1° vs. 54.0°, p = 0.020), decreased maximum flexion (52.3° vs. 57.5°, p = 0.002), increased adduction angle (2.0–7.5° vs. −2.8–3.0°, p < 0.05) and increased external tibial rotation (by a mean of 2.3 ± 0.7°, p < 0.001). The postoperative KOOS score was significantly higher in the kinematic alignment group compared to the mechanical alignment group (74.2 vs. 60.7, p = 0.034). Such results demonstrate that a better restoration of the individual’s knee anatomy and ligament tension led to improved knee kinematics and clinical outcomes and greater patient satisfaction.
On the other hand, achieving a patient-specific implant implantation with a non-anatomic prosthesis design makes little sense either. The next logical step on this road forward would be to have a personalized implant to reproduce individual anatomy.
4 Customised Implants
Re-establishing the native knee anatomy and kinematics using custom implants has recently been developed as a novel technology in TKA. Matching the bony anatomy with the implant geometry should facilitate restoration of the native pre-arthritic limb alignment. Belzile et al. and Bonnin et al. in Chaps. 19 and 22 discuss the advantages of such patient-specific implants. These include an optimised implant fit to the native bone, avoiding prosthetic overhang or under-coverage. Improved ligament balancing may be achieved by avoiding resection laxity due to asymmetric bone cuts. Restoring the native radii of curvature of the knee may improve mid-flexion stability and kinematics. Restoring the native femoral rotation and a customised trochlea may lead to improved patellofemoral tracking.
The anatomy of the knee has been shown to vary by gender, ethnicity and body type [14, 15]. Furthermore, within these groups, there is substantial variation such that every individual has a unique anatomical geometry [16]. This would suggest that a customised implant would be advantageous to try to replicate this individual variation.
Although these customised implants are reproducing the bony anatomy and native knee alignment, they still resect the cruciate ligaments. Resecting the cruciate ligaments will affect the knee kinematics. Perhaps, the path to a more natural, forgotten joint should start with preservation of the cruciate ligaments.
Bi-cruciate-preserving TKA is not a new procedure, but as Pritchett et al. point out in Chap. 23, there are a number of new implant designs. There have been high failure rates of some historical designs of these knee replacements. This is in part because preservation of the cruciate ligaments is technically difficult. However, if done correctly, there is evidence of good long-term survivorship with excellent functional outcome.
Preservation of the cruciate ligaments mandates the correct tension of all of the knee’s ligaments. There is more natural transmission of weight-bearing forces with more natural kinematics. Traditional CR design TKAs often exhibit paradoxical anterior slide and reverse rotation of the femoral component with increasing flexion [17, 18].
This consistent motion pattern is thought to be a result of the absence of the ACL, with the resultant inability to counterbalance the PCL properly and account for the changed geometry of the prosthesis [19].
Patient-specific/custom designs of bi-cruciate-preserving TKA that facilitate implantation and reduce the risks of specific complications such as fracture of the tibial eminence may be a possible solution to reproducing normal knee kinematics.
5 Optimized Perioperative Care
Many of the advances in TKA surgery have been around the optimization of the perioperative care. This has seen a large reduction in the number of inpatient days following a joint replacement. The introduction of principles of enhanced recovery after surgery (ERAS) in TKA surgery has improved patient’s well-being to a level allowing them to return home the same day (Fig. 15.4).
Implementation of an ERAS protocol in our facility had a dramatic impact on patient outcomes. We compared the complications rated according to the Clavien-Dindo scale, hospital LOS and costs of the episode of care between our first 120 ERAS short-stay THA or TKA and a matched historical control group of 150 THA or TKA [20]. ERAS cases had lower rate of Grade 1 and 2 complications compared with the standard group (mean 0.8 vs. 3.0, p < 0.001). No difference was found between the two groups for Grade 3, 4 or 5 complications. The mean hospital length of stay for the ERAS short-stay group decreased by 2.8 days for the THAs (0.1 vs. 2.9 days, p < 0.001) and 3.9 days for the TKAs (1.0 vs. 4.9 days, p < 0.001). The mean estimated direct healthcare costs reduction with the ERAS short-stay protocol was 1489 CND per THA and 4206 CND per TKA. Implementation of an ERAS short-stay protocol for patients undergoing THA or TKA at our institution resulted not only in reduced hospital length of stay but also in improved patient care and reduced direct healthcare costs.
A successful ERAS program requires multidisciplinary collaboration among anaesthesiologists, surgeons, physiotherapists, nurses and hospital administrators. The future of knee arthroplasty, is to improve perioperative care to obtain the ultimate goal of a “pain- and risk-free operation” [21].
6 Conclusion
It is an exciting time for surgeons to be performing knee replacements. The initial aim of TKA surgery in providing a reliable prosthesis with good survivorship has been met. The focus has therefore shifted to improving patient function, kinematics and satisfaction. New precision technologies, replication of native alignment and anatomy with preservation of soft tissues and ligaments are the areas of current and future developments in the field. The future of knee arthroplasty will rely on a personalized joint reconstruction. A patient-specific/custom prosthetic implanted with precision to match patient anatomy, coupled with a holistic perioperative care model will hopefully lead to the holy grail of joint replacement surgery: a forgotten or natural knee joint.
References
Collins M, Lavigne M, Girard J, Vendittoli PA. Joint perception after hip or knee replacement surgery. Orthop Traumatol Surg Res. 2012;98:275–80.
Bourne RB, Chesworth BM, Davis AM, Mahomed NN, Charron KDJ. Patient satisfaction after total knee arthroplasty: who is satisfied and who is not? Clin Orthop Relat Res. 2010;468:57–63.
McClelland JA, Webster KE, Feller JA. Gait analysis of patients following total knee replacement: a systematic review. Knee. 2007;14:253–63.
Bellemans J, Colyn W, Vandenneucker H, Victor J. The Chitranjan Ranawat award: is neutral mechanical alignment normal for all patients? The concept of constitutional varus. Clin Orthop Relat Res. 2012;470:45–53.
Almaawi AM, Hutt JRB, Masse V, Lavigne M, Vendittoli P-A. The impact of mechanical and restricted kinematic alignment on knee anatomy in total knee arthroplasty. J Arthroplast. 2017;32:2133–40.
Eckhoff DG, Bach JM, Spitzer VM, et al. Three-dimensional mechanics, kinematics, and morphology of the knee viewed in virtual reality. J Bone Joint Surg Am. 2005;87(Suppl 2):71–80.
Robinson RP. The early innovators of today’s resurfacing condylar knees. J Arthroplast. 2005;20:2–26.
Blakeney W, Beaulieu Y, Puliero B, Kiss MO, Vendittoli PA. Bone resection for mechanically aligned total knee arthroplasty creates frequent gap modifications and imbalances. Knee Surg Sports Traumatol Arthrosc. 2019. https://doi.org/10.1007/s00167-019-05562-8.
Rivière C, Vigdorchik JM, Vendittoli PA. Mechanical alignment: The end of an era! Orthop Traumatol Surg Res. 2019;105(7):1223–6.
Hetaimish BM, Khan MM, Simunovic N, Al-Harbi HH, Bhandari M, Zalzal PK. Meta-analysis of navigation vs conventional total knee arthroplasty. J Arthroplast. 2012;27:1177–82.
de Steiger RN, Liu YL, Graves SE. Computer navigation for total knee arthroplasty reduces revision rate for patients less than sixty-five years of age. J Bone Joint Surg Am. 2015;97:635–42.
Abdel MP, Ollivier M, Parratte S, Trousdale RT, Berry DJ, Pagnano MW. Effect of postoperative mechanical axis alignment on survival and functional outcomes of modern total knee arthroplasties with cement: a concise follow-up at 20 years. J Bone Joint Surg Am. 2018;100:472–8.
Blakeney W, Clement J, Desmeules F, Hagemeister N, Riviere C, Vendittoli PA. Kinematic alignment in total knee arthroplasty better reproduces normal gait than mechanical alignment. Knee Surg Sports Traumatol Arthrosc. 2019;27(5):1410–7.
Leszko F, Hovinga KR, Lerner AL, Komistek RD, Mahfouz MR. In vivo normal knee kinematics: is ethnicity or gender an influencing factor? Clin Orthop Relat Res. 2011;469:95–106.
Bellemans J, Carpentier K, Vandenneucker H, Vanlauwe J, Victor J. The John Insall Award: both morphotype and gender influence the shape of the knee in patients undergoing TKA. Clin Orthop Relat Res. 2010;468:29–36.
van den Heever DJ, Scheffer C, Erasmus P, Dillon E. Classification of gender and race in the distal femur using self organising maps. Knee. 2012;19:488–92.
Yoshiya S, Matsui N, Komistek RD, Dennis DA, Mahfouz M, Kurosaka M. In vivo kinematic comparison of posterior cruciate-retaining and posterior stabilized total knee arthroplasties under passive and weight-bearing conditions. J Arthroplast. 2005;20:777–83.
Cates HE, Komistek RD, Mahfouz MR, Schmidt MA, Anderle M. In vivo comparison of knee kinematics for subjects having either a posterior stabilized or cruciate retaining high-flexion total knee arthroplasty. J Arthroplast. 2008;23:1057–67.
Zeller IM, Sharma A, Kurtz WB, Anderle MR, Komistek RD. Customized versus patient-sized cruciate-retaining total knee arthroplasty: an in vivo kinematics study using mobile fluoroscopy. J Arthroplast. 2017;32:1344–50.
Vendittoli PA, Pellei K, Desmeules F, Lavigne M, Massé V, Loubert C, Fortier L-P. Enhanced recovery short-stay hip and knee joint replacement program improves patients outcomes while reducing hospital costs. Orthop Traumatol Surg Res. 2019;105(7):1237–43.
Kehlet H. Enhanced recovery after surgery (ERAS): good for now, but what about the future? Can J Anaesth. 2015;62:99–104.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Open Access This chapter is licensed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
The images or other third party material in this chapter are included in the chapter's Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the chapter's Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Copyright information
© 2020 The Author(s)
About this chapter
Cite this chapter
Blakeney, W.G., Vendittoli, PA. (2020). The Future of TKA. In: Rivière, C., Vendittoli, PA. (eds) Personalized Hip and Knee Joint Replacement. Springer, Cham. https://doi.org/10.1007/978-3-030-24243-5_15
Download citation
DOI: https://doi.org/10.1007/978-3-030-24243-5_15
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-24242-8
Online ISBN: 978-3-030-24243-5
eBook Packages: MedicineMedicine (R0)