Abstract
Background and Objective: Posaconazole (Noxafil®) is an extended-spectrum triazole antifungal agent for prevention and treatment of invasive fungal infections. An inadequate dietary intake and abnormal gastric pH levels are common in critically ill patients receiving antifungal treatment with posaconazole, resulting in unpredictable bioavailability and sub-therapeutic plasma concentrations. This study was carried out to elucidate the impact of pH on posaconazole absorption and to explore the underlying mechanisms of enhanced intestinal absorption when coadministering an acidic carbonated beverage. In contrast to previously published studies, in which only plasma concentrations were determined, we also explored the gastric and intestinal behaviour of posaconazole after a single oral dose.
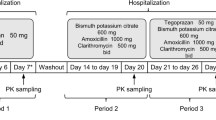
Methods: A crossover study was performed in five healthy subjects. A single dose (10 mL) of posaconazole suspension (40 mg/mL) was administered orally in four different conditions: with 330 mL of water (condition 1); with 330 mL of a cola beverage [Coca-Cola®] (condition 2); with 330 mL of water following intake of the proton pump inhibitor esomeprazole 40 mg once daily for 3 days (condition 3); or with 330 mL of Coca-Cola® following intake of esomeprazole 40 mg once daily for 3 days (condition 4). After administration, gastrointestinal fluid and plasma samples were collected at regular time points, and posaconazole concentrations were determined.
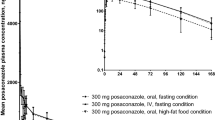
Results: Compared with administration with water, coadministration of Coca-Cola® did not alter the pH of the intraluminal environment but did significantly increase posaconazole gastric concentrations (+102%; p < 0.001) and systemic exposure (+70%; p<0.05). This enhancement could be attributed to improved posaconazole solubility in Coca-Cola® and prolonged gastric residence. Coadministration of esomeprazole led to an increased gastric pH, which was accompanied by decreased posaconazole absorption; the mean plasma and gastric area under the concentration-time curve (AUC) values decreased by 37% and 84%, respectively. Simultaneous intake of Coca-Cola® could not completely compensate for the increase in pH induced by esomeprazole; compared with the reference condition, the mean plasma and gastric AUC values were still decreased by 19% and 73%, respectively. A good correlation between plasma and gastric posaconazole concentrations was observed (r=0.8165; p<0.0001), indicating that dissolution in the stomach dictates absorption of posaconazole.
Conclusions: These results demonstrate that coadministration of Coca-Cola® has a positive effect on posaconazole bioavailability in the fasted state. However, it can only be considered a partially efficient strategy to increase absorption in patients with inadequate food intake who exhibit abnormal gastric pH levels due to coadministration of acid-suppressive agents.








Similar content being viewed by others
References
Schiller DS, Fung HB. Posaconazole: an extended-spectrum triazole antifungal agent. Clin Ther 2007; 29(9): 1862–86
Nagappan V, Deresinski S. Reviews of anti-infective agents: posaconazole: a broad-spectrum triazole antifungal agent. Clin Infect Dis 2007; 45(12): 1610–7
Keating GM. Posaconazole. Drugs 2005; 65(11): 1553–67; discussion 1568-9
Sabatelli F, Patel R, Mann PA, et al. In vitro activities of posaconazole, fluconazole, itraconazole, voriconazole, and amphotericin B against a large collection of clinically important molds and yeasts. Antimicrob Agents Chemother 2006; 50(6): 2009–15
Espinel-Ingroff A. Comparison of in vitro activities of the new triazole SCH56592 and the echinocandins MK-0991 (L-743,872) and LY303366 against opportunistic filamentous and dimorphic fungi and yeasts. J Clin Microbiol 1998; 36(10): 2950–6
Manavathu EK, Cutright JL, Loebenberg D, et al. A comparative study of the in vitro susceptibilities of clinical and laboratory-selected resistant isolates of Aspergillus spp. to amphotericin B, itraconazole, voriconazole and posaconazole (SCH 56592). J Antimicrob Chemother 2000; 46(2): 229–34
Pfaller MA, Messer SA, Hollis RJ, et al. In vitro activities of posaconazole (Sch 56592) compared with those of itraconazole and fluconazole against 3,685 clinical isolates of Candida spp. and Cryptococcus neoformans. Antimicrob Agents Chemother 2001; 45(10): 2862–4
Pfaller MA, Messer SA, Hollis RJ, et al. Antifungal activities of posaconazole, ravuconazole, and voriconazole compared to those of itraconazole and amphotericin B against 239 clinical isolates of Aspergillus spp. and other filamentous fungi: report from SENTRY Antimicrobial Surveillance Program, 2000. Antimicrob Agents Chemother 2002; 46(4): 1032–7
Krieter P, Flannery B, Musick T, et al. Disposition of posaconazole following single-dose oral administration in healthy subjects. Antimicrob Agents Chemother 2004; 48(9): 3543–51
Courtney R, Pai S, Laughlin M, et al. Pharmacokinetics, safety, and tolerability of oral posaconazole administered in single and multiple doses in healthy adults. Antimicrob Agents Chemother 2003; 47(9): 2788–95
Sansone-Parsons A, Krishna G, Simon J, et al. Effects of age, gender, and race/ethnicity on the pharmacokinetics of posaconazole in healthy volunteers. Antimicrob Agents Chemother 2007; 51(2): 495–502
Courtney R, Wexler D, Radwanski E, et al. Effect of food on the relative bioavailability of two oral formulations of posaconazole in healthy adults. Br J Clin Pharmacol 2004; 57(2): 218–22
Ezzet F, Wexler D, Courtney R, et al. Oral bioavailability of posaconazole in fasted healthy subjects: comparison between three regimens and basis for clinical dosage recommendations. Clin Pharmacokinet 2005; 44(2): 211–20
Krishna G, Moton A, Ma L, et al. Pharmacokinetics and absorption of posaconazole oral suspension under various gastric conditions in healthy volunteers. Antimicrob Agents Chemother 2009; 53(3): 958–66
Lewis R, Hogan H, Howell A, et al. Progressive fusariosis: unpredictable posaconazole bioavailability, and feasibility of recombinant interferon-gamma plus granulocyte macrophage-colony stimulating factor for refractory disseminated infection. Leuk Lymphoma 2008; 49(1): 163–5
Fennerty MB. Pathophysiology of the upper gastrointestinal tract in the critically ill patient: rationale for the therapeutic benefits of acid suppression. Crit Care Med 2002; 30(6 Suppl.): S351–5
Jain R, Pottinger P. The effect of gastric acid on the absorption of posaconazole [letter]. Clin Infect Dis 2008; 46(10): 1627; author reply 1627-8
Courtney R, Radwanski E, Lim J, et al. Pharmacokinetics of posaconazole coadministered with antacid in fasting or nonfasting healthy men. Antimicrob Agents Chemother 2004; 48(3): 804–8
Jaruratanasirikul S, Kleepkaew A. Influence of an acidic beverage (Coca-Cola) on the absorption of itraconazole. Eur J Clin Pharmacol 1997; 52(3): 235–7
Lange D, Pavao JH, Wu J, et al. Effect of a cola beverage on the bioavailability of itraconazole in the presence of H2 blockers. J Clin Pharmacol 1997; 37(6): 535–40
Chin TW, Loeb M, Fong IW. Effects of an acidic beverage (Coca-Cola) on absorption of ketoconazole. Antimicrob Agents Chemother 1995; 39(8): 1671–5
Lim SG, Sawyerr AM, Hudson M, et al. Short report: the absorption of fluconazole and itraconazole under conditions of low intragastric acidity. Aliment Pharmacol Ther 1993; 7(3): 317–21
Lelawongs P, Barone JA, Colaizzi JL, et al. Effect of food and gastric acidity on absorption of orally administered ketoconazole. Clin Pharm 1988; 7(3): 228–35
Brouwers J, Ingels F, Tack J, et al. Determination of intraluminal theophylline concentrations after oral intake of an immediate- and a slow-release dosage form. J Pharm Pharmacol 2005; 57(8): 987–96
Brouwers J, Tack J, Lammert F, et al. Intraluminal drug and formulation behavior and integration in in vitro permeability estimation: a case study with amprenavir. J Pharm Sci 2006; 95(2): 372–83
Müller-Lissner SA, Fimmel CJ, Will N, et al. Effect of gastric and transpyloric tubes on gastric emptying and duodenogastric reflux. Gastroenterology 1982; 83(6): 1276–9
Ploutz-Snyder L, Foley J, Ploutz-Snyder R, et al. Gastric gas and fluid emptying assessed by magnetic resonance imaging. Eur J Appl Physiol Occup Physiol 1999; 79(3): 212–20
Houston JB, Levy G. Effect of carbonated beverages and of an antiemetic containing carbohydrate and phosphoric acid on riboflavin bioavailability and salicylamide biotransformation in humans. J Pharm Sci 1975; 64(9): 1504–7
AstraZeneca Pharmaceuticals LP. Nexium® (esomeprazole magnesium): US prescribing information [online]. Available from URL: http://www1.astrazeneca-us.com/pi/Nexium.pdf [Accessed 2011 May 26]
Maton PN, Burton ME. Antacids revisited: a review of their clinical pharmacology and recommended therapeutic use. Drugs 1999; 57(6): 855–70
Pea F, Furlanut M, Viale P. What should be the first-choice strategy to maximize posaconazole exposure in daily clinical practice? [letter]. Antimicrob Agents Chemother 2009; 53(8): 3608–9; author reply 3609-10
Goodwin ML, Drew RH. Antifungal serum concentration monitoring: an update. J Antimicrob Chemother 2008; 61(1): 17–25
Andes D, Pascual A, Marchetti O. Antifungal therapeutic drug monitoring: established and emerging indications. Antimicrob Agents Chemother 2009; 53(1): 24–34
Acknowledgements
Jeroen Walravens and Joachim Brouwers contributed equally to this work and should be considered joint first authors of the article.
This research was funded by grants from the Research Foundation — Flanders (FWO; Brussels, Belgium) and from the “Onderzoeksfonds” of the Katholieke Universiteit Leuven (Leuven, Belgium). Dr J. Brouwers is a postdoctoral fellow of the FWO. The authors declare that they have no conflicts of interest to disclose.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Walravens, J., Brouwers, J., Spriet, I. et al. Effect of pH and Comedication on Gastrointestinal Absorption of Posaconazole. Clin Pharmacokinet 50, 725–734 (2011). https://doi.org/10.2165/11592630-000000000-00000
Published:
Issue Date:
DOI: https://doi.org/10.2165/11592630-000000000-00000