Abstract
Background
The Physical Resilience Instrument for Older Adults (PRIFOR) is a questionnaire for assessing physical resilience in older adults suffering from acute health stressors. Prior psychometric evidence of the PRIFOR showed that it has good criterion-related validity, known-group validity, predictive validity, and internal consistency. However, it is unclear whether the PRIFOR can be replicated in older adults suffering after surgical treatment.
Objectives
This study aimed at evaluating whether the three-factor structure of the PRIFOR can be replicated in older adults suffering after surgical treatment. Moreover, the concurrent validity of the PRIFOR was examined using the association between the PRIFOR and measures of depression, cognition, activities of daily living, and frailty.
Design and Setting
A longitudinal study was adopted in a tertiary-care medical center in Taiwan.
Participants
A total of 207 patients aged 65 years old and older who underwent surgery and if they were able to communicate independently. Measurements: The PRIFOR, the 5-item Geriatric Depression Scale, the Short Portable Mental Status Questionnaire, the Katz Index of Independence in Activities of Daily Living and Clinical Frailty Scale were all assessed after surgery.
Results
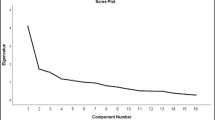
The three-factor structure (positive thinking, cope and adjust lifestyle, and belief and hopeful mindset) was supported by the CFA results in the present sample. In addition, the PRIFOR showed good concurrent validity with depression (r = −0.470 to −0.542), cognition (r = 0.358 to 0.409), activities of daily living (r = 0.209 to 0.310), and frailty (r =−0.161 to −0.237).
Conclusion
The PRIFOR can be recommended to measure physical resilience in older adults suffering after surgical treatment. For the adequate estimation of older adults’ level of physical resilience postoperatively and to guide the implementation of individualized interventions, it is important to provide appropriate care for older adults to recover after surgery.
Similar content being viewed by others
References
Hadley EC, Kuchel GA, Newman AB, et al. Report: NIA workshop on measures of physiologic resiliencies in human aging. J Gerontol A Biol Sci Med Sci 2017;72:980–990. doi:https://doi.org/10.1093/gerona/glx015
Nygren B, Aléx L, Jonsén E, Gustafson Y, Norberg A, Lundman B. Resilience, sense of coherence, purpose in life and self-transcendence in relation to perceived physical and mental health among the oldest old. Aging Ment Health 2005;9:354–362. doi:https://doi.org/10.1080/1360500114415
Whitson HE, Duan-Porter W, Schmader KE, Morey MC, Cohen HJ, Colón-Emeric CS. Physical resilience in older adults: systematic review and development of an emerging construct. J Gerontol A Biol Sci Med Sci 2016;71:489–495. doi:https://doi.org/10.1093/gerona/glv202
Johnson AJ, Terry E, Bartley EJ, et al. Resilience factors may buffer cellular aging in individuals with and without chronic knee pain. Mol Pain 2019;15:1744806919842962. doi:https://doi.org/10.1177/1744806919842962
Colon-Emeric C, Pieper CF, Schmader KE, et al. Two approaches to classifying and quantifying physical resilience in longitudinal data. J Gerontol A Biol Sci Med Sci 2020;75:731–738. doi:https://doi.org/10.1093/gerona/glz097
Hu FW, Lin CH, Yueh FR, Lo YT, Lin CY. Development and psychometric evaluation of the Physical Resilience Instrument for Older Adults (PRIFOR). BMC geriatr 2022;22:229. doi:https://doi.org/10.1186/s12877-022-02918-7
Hu FW, Lin CH, Lai PH, Lin CY. Predictive Validity of the Physical Resilience Instrument for Older Adults (PRIFOR). J Nutr Health Aging 2021;25:1042–1045. doi:https://doi.org/10.1007/s12603-021-1667-6
Huang HT, Chang CM, Liu LF, Lin HS, Chen CH. Trajectories and predictors of functional decline of hospitalised older patients. J Clin Nurs 2013;22:1322–1331. doi:https://doi.org/10.1111/jocn.12055
Berian JR, Mohanty S, Ko CY, Rosenthal RA, Robinson TN. Association of loss of independence with readmission and death after discharge in older patients after surgical procedures. JAMA Surg 2016;151:e161689. doi:https://doi.org/10.1001/jamasurg.2016.1689
Zhang LM, Hornor MA, Robinson T, Rosenthal RA, Ko CY, Russell MM. Evaluation of postoperative functional health status decline among older adults. JAMA Surg 2020;115: 950–958. doi:https://doi.org/10.1001/jamasurg.2020.2853
Hoyl MT, Alessi CA, Harker JO, et al. Development and testing of a five-item version of the geriatric depression scale. J Am Geriatr Soc. 1999;47:873–878. doi:https://doi.org/10.1111/j.1532-5415.1999.tb03848.x
Rinaldi P, Mecocci P, Benedetti C, et al. Validation of the five-item geriatric depression scale in elderly subjects in three different settings. J Am Geriatr Soc 2003;51:694–698. doi:https://doi.org/10.1034/j.1600-0579.2003.00216.x
Pfeiffer E. A short portable mental status questionnaire for the assessment of organic brain deficit in elderly patients. J Am Geriatr Soc 1975;23:433–441. doi:https://doi.org/10.1111/j.1532-5415.1975.tb00927.x
Chou KL. Hong Kong Chinese everyday competence scale: a validation study. Clin Gerontol 2002;26:43–51. doi:https://doi.org/10.1300/J018v26n01_05
Haglund RMJ, Schuckid MA. A clinical comparison of tests of organicity in elderly patients. J Gerontol 1976;31:645–459. doi:https://doi.org/10.1093/geronj/31.6.654
Katz S, Ford AB, Moskowitz RS. Studies of illness in the aged. The index of ADL: a standardized measure of biological and psychosocial function. JAMA 1963;185:914–919. doi:https://doi.org/10.1001/jama.1963.03060120024016
Reijneveld SA, Spijker J, Dijkshoorn H. Katz’ ADL index assessed functional performance of Turkish, Moroccan, and Dutch elderly. J Clin Epidemiol 2007;60:82–88. doi:https://doi.org/10.1016/j.jclinepi.2006.02.022
Rockwood K, Song X, MacKnight C, et al. A global clinical measure of fitness and frailty in elderly people. CMAJ 2005;173:489–495. doi:https://doi.org/10.1503/cmaj.050051
Pulok MH, Theou O, van der Valk AM, Rockwood K. The role of illness acuity on the association between frailty and mortality in emergency department patients referred to internal medicine. Age Ageing 2020;49:1071–1079. doi:https://doi.org/10.1093/ageing/afaa089
Mavros MN, Athanasiou S, Gkegkes ID, Polyzos KA, Peppas G, Falagas ME. Do psychological variables affect early surgical recovery?. PLoS One 2011;6:e20306. doi:https://doi.org/10.1371/journal.pone.0020306
Kiecolt-Glaser JK, Page GG, Marucha PT, MacCallum RC, Glaser R. Psychological influences on surgical recovery. Perspectives from psychoneuroimmunology. Am Psychol. 1998;53:1209–1218. doi:https://doi.org/10.1037//0003-066x.53.11.1209
Segerstrom SC, Miller GE. Psychological stress and the human immune system: a meta-analytic study of 30 years of inquiry. Psychol Bull 2004;130:601–630. doi:https://doi.org/10.1037/0033-2909.130.4.601
Glaser R, Kiecolt-Glaser JK, Marucha PT, MacCallum RC, Laskowski BF, Malarkey WB. Stress-related changes in proinflammatory cytokine production in wounds. Arch Gen Psychiatry 1999;56:450–456. doi:https://doi.org/10.1001/archpsyc.56.5.450
Lim KK, Matchar DB, Tan CS, Yeo W, Østbye T, Howe TS, Koh JSB. The association between psychological resilience and physical function among older adults with hip fracture surgery. J Am Med Dir Assoc 2020;21:260–266. doi:https://doi.org/10.1016/j.jamda.2019.07.005
Divaasini D, Zhooriyati SM. Psychological effects and coping strategies after major surgery in adults. Jurnal Psikologi Malaysia. 2019;33(2):37–48.
Liu BS, Huang HC. Family care for the elderly and the importance of filial piety. Hu Li Za Zhi 2009;56:83–88.
Huber M, Knottnerus JA, Green L, et al. How should we define health?. BMJ 2011; 343: d4163. doi:https://doi.org/10.1136/bmj.d4163
Parker DC, Colón-Emeric C, Huebner JL, et al. Biomarkers associated with physical resilience after hip fracture. J Gerontol A Biol Sci Med Sci 2020;75:e166–e172. doi:https://doi.org/10.1093/gerona/glaa119
Gijzel SMW, Rector J, van Meulen FB, et al. Measurement of dynamical resilience indicators improves the prediction of recovery following hospitalization in older adults. J Am Med Dir Assoc 2020;21:525–530.e4. doi:https://doi.org/10.1016/j.jamda.2019.10.011
Whitson HE, Cohen HJ, Schmader KE, Morey MC, Kuchel G, Colon-Emeric CS. Physical resilience: not simply the opposite of frailty. J Am Geriatr Soc 2018; 66:1459–1461. doi:https://doi.org/10.1111/jgs.15233
Author information
Authors and Affiliations
Contributions
Author Contributions: FWH and CMC conceptualized the study. FWH, CHO and CYL were responsible for the data collection, analysis and interpretation of the results. FWH and CYL contributed substantially to the writing of the manuscript.
Corresponding author
Ethics declarations
Conflict of Interest: None of the authors have conflicts related to this manuscript.
Ethical standards: The study protocol was approved by the Institutional Review Board of National Cheng Kung University Hospital (No. A-ER-109-233).
Additional information
Financial Disclosure: This study was supported by a grant from the Ministry of Science and Technology (MOST 109-2314-B-006-072-MY3).
Sponsor Role: None.
Rights and permissions
About this article
Cite this article
Lin, CY., Ou, CH., Chang, CM. et al. The Physical Resilience Instrument for Older Adults (PRIFOR) in Surgical Inpatients: Further Evidence for Its Factor Structure and Validity. J Frailty Aging 12, 91–96 (2023). https://doi.org/10.14283/jfa.2023.8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.14283/jfa.2023.8