Abstract
Purpose
We reported preliminary outcomes of high-intensity focused ultrasound (HIFU) [Sonablate®] in the combination of transurethral resection of the prostate for localized prostate cancer in Taiwan.
Methods
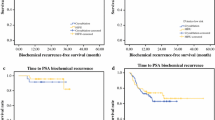
Seventy-seven patients using Sonablate® HIFU for localized prostate cancer were enrolled in this study from April 2021 to December 2022. Prostate-specific antigen biochemical recurrence, International Index of Erectile Function (IIEF)-5 scores, International Prostate Symptom Score (IPSS), quality of life (QoL) scores, and postoperative complications were recorded during follow-up.
Results
Overall, 19.5% of patients were low-risk, 36.4% were intermediate-risk, and 44.1% were high-risk according to the D’Amico risk classification. The median follow-up was 12.09 ± 5.85 months, and the biochemical-free survival rates for the low-, intermediate-, and high-risk groups were 100% (15/15), 96.4% (27/28), and 79.4% (27/34), respectively. Four patients (5.2%) received salvage radiotherapy and all maintained biochemical-free survival. The mean IPSS and QoL scores before versus after HIFU were 10.4 versus 6.8 (p = 0.003) and 3.2 versus 3.0 (p = 0.096), respectively. There was no statistically significant change in preoperative and postoperative IIEF scores (20.6 vs. 19; p = 0.062) in patients who had an IIEF score of >15 at baseline and received nerve-sparing procedures (subtotal ablation).
Conclusions
The results of Sonablate® HIFU in Taiwan indicated adequate short-term cancer control, excellent potency, and continence preservation. HIFU can achieve improvement of IPSS with low complication rates.

Similar content being viewed by others
References
Bray F, et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424.
Cooperberg MR, et al. Contemporary trends in low-risk prostate cancer: risk assessment and treatment. J Urol. 2007;178(3 Pt 2):S14–9.
Ziglioli F, et al. Oncologic outcome, side effects and comorbidity of high-intensity focused ultrasound (HIFU) for localized prostate cancer: a review. Ann Med Surg (Lond). 2020;56:110–5.
Eastham JA, Scardino PT, Kattan MW. Predicting an optimal outcome after radical prostatectomy: the trifecta nomogram. J Urol. 2008;179(6):2207–10; discussion 2210-1.
Bakavicius A, et al. Comprehensive evaluation of focal therapy complications in prostate cancer: a standardized methodology. J Endourol. 2019;33(7):509–15.
Valerio M, et al. The role of focal therapy in managing localized prostate cancer: a systematic review. Eur Urol. 2014;66(4):732–51.
Liu YY, Chiang PH. Comparisons of oncological and functional outcomes between primary whole-gland cryoablation and high-intensity focused ultrasound for localized prostate cancer. Ann Surg Oncol. 2016;23(1):328–34.
Chiang PH, Liu YY. Comparisons of oncological and functional outcomes among radical retropubic prostatectomy, high dose rate brachytherapy, cryoablation, and high-intensity focused ultrasound for localized prostate cancer. Springerplus. 2016;5(1):1905–12.
Chen PY, Ching PH, Liu YY, et al. Primary whole-gland ablation for localized prostate cancer with high-intensity focused ultrasound: the important predictors of biochemical recurrence. Int Urol. 2018;25(6):615–20.
Wu YT, Chiang PH. Cohort study of high-intensity focused ultrasound in the treatment of localized prostate cancer treatment: medium-term results from a single center. PLoS One. 2020;15(7):e0236026.
Kennedy JE, Ter Haar GR, Cranston D. High intensity focused ultrasound: surgery of the future? Br J Radiol. 2003;76(909):590–9.
Bozzini G, et al. Focal therapy of prostate cancer: energies and procedures. Urol Oncol. 2013;31(2):155–67.
Susani M, et al. Morphology of tissue destruction induced by focused ultrasound. Eur Urol. 1993;23(Suppl 1):34–8.
Stride EP, Coussios CC. Cavitation and contrast: the use of bubbles in ultrasound imaging and therapy. Proc Inst Mech Eng H 2010;224(2):171–91.
Tourinho-Barbosa RR, de la Rosette J, Sanchez-Salas R. Prostate cancer multifocality, the index lesion, and the microenvironment. Curr Opin Urol. 2018;28(6):499–505.
Sogutdelen E, Haberal HB, Guliyev F, et al. Urethral stricture is an unpleasant complication after prostate surgery: a critical review of current literature. J Urol Surg. 2016;3(1):1–6.
Crouzet S, et al. Whole-gland ablation of localized prostate cancer with high-intensity focused ultrasound: oncologic outcomes and morbidity in 1002 patients. Eur Urol. 2014;65(5):907–14.
Thüroff S, Chaussy C. Evolution and outcomes of 3 MHz high intensity focused ultrasound therapy for localized prostate cancer during 15 years. J Urol. 2013;190(2):702–10.
Pinthus JH, et al. Single-session primary high-intensity focused ultrasonography treatment for localized prostate cancer: biochemical outcomes using third generation-based technology. BJU Int. 2012;110(8):1142–8.
Misraï V, et al. Oncologic control provided by HIFU therapy as single treatment in men with clinically localized prostate cancer. World J Urol. 2008;26(5):481–5.
Blana A, et al. First analysis of the long-term results with transrectal HIFU in patients with localized prostate cancer. Eur Urol. 2008;53(6):1194–201.
Chaussy C, Thüroff S. The status of high-intensity focused ultrasound in the treatment of localized prostate cancer and the impact of a combined resection. Curr Urol Rep. 2003;4(3):248–52.
Netsch C, Pfeiffer D, Gross AJ. Development of bladder outlet obstruction after a single treatment of prostate cancer with high-intensity focused ultrasound: experience with 226 patients. J Endourol. 2010;24(9):1399–403.
Wilt TJ, et al. Radical prostatectomy versus observation for localized prostate cancer. N Engl J Med. 2012;367(3):203–13.
Demirel CH, Altok M, Davis JW. Focal therapy for localized prostate cancer: is there a “middle ground” between active surveillance and definitive treatment? Asian J Androl. 2018;21(1):37–44. https://doi.org/10.4103/aja.aja_64_18.
Huang YC, Kan CH, Chiang PH, et al. Salvage radiotherapy plus androgen deprivation therapy for high-risk prostate cancer with biochemical failure after high-intensity focused ultrasound as primary treatment. J Clin Med. 2022;11:4450–8.
Mearini L, Porena M. Transrectal high-intensity focused ultrasound for the treatment of prostate cancer: past, present, and future. Indian J Urol. 2010;26(1):4–11. https://doi.org/10.4103/0970-1591.60436.
Sia M, Pickles T, Morton G, Souhami L, Lukka H, Warde P. Salvage radiotherapy following biochemical relapse after radical prostatectomy: proceedings of the Genito-Urinary Radiation Oncologists of Canada consensus meeting. Can Urol Assoc J. 2008;2(5):500–7. https://doi.org/10.5489/cuaj.916.
Bechis SK, Carroll PR, Cooperberg MR. Impact of age at diagnosis on prostate cancer treatment and survival. J Clin Oncol. 2011;29(2):235–41. https://doi.org/10.1200/JCO.2010.30.2075.
Chaussy CG, Thüroff S. High-intensity focused ultrasound for the treatment of prostate cancer: a review. J Endourol. 2017;31(1):S30–7.
Acknowledgments
This study was supported by the Chin Pei Medical Foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Mu Yao Tsai, Chih Tai Lin, Ping Hsuan Chiang, Po Hui Chiang, and Ping Chia Chiang have no conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Tsai, M.Y., Lin, C.T., Chiang, P.H. et al. High-Intensity Focused Ultrasound (Sonablate®) for Prostate Cancer: Preliminary Outcomes in Taiwan. Ann Surg Oncol 30, 8764–8769 (2023). https://doi.org/10.1245/s10434-023-14250-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-023-14250-4