Abstract
Background
Sarcopenia and cachexia are two predictors of adverse clinical outcomes, but they are partly overlapping. We aimed to compare the characteristics and prognostic value of cachexia and sarcopenia in patients after gastrectomy.
Methods
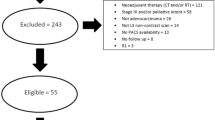
From 2014 to 2019, a total of 1215 gastric cancer patients were enrolled. Cachexia and sarcopenia were diagnosed according to the most recent consensus definitions. Baseline characteristics and clinical outcomes were compared between the two groups. Risk factors of survival were evaluated by Cox regression analysis.
Results
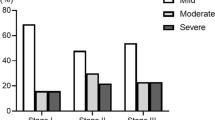
Of all patients, 26.5% were diagnosed with cachexia and 19.8% were diagnosed with sarcopenia. Sarcopenia was more prevalent in elderly patients, while cachexia was prone to occur in patients with TMN stage III. Survival curves showed that sarcopenia had adverse effects in patients with TMN stage I and II–III, while cachexia was only associated with poor survival at stages II–III. For the entire cohort, both cachexia and sarcopenia were adverse factors for prognosis. However, for stage I patients, sarcopenia was an independent predictor for overall survival (OS) (HR = 4.939, P < 0.001) and disease-free survival (DFS) (HR = 4.256, P < 0.001), but not cachexia; for stage II–III patients, cachexia was an independent predictor for OS (HR = 1.538, P < 0.001) and DFS (HR = 1.473, P = 0.001), but not sarcopenia.
Conclusions
Sarcopenia and cachexia have different clinical characteristics and prognostic values. For patients with early stage gastric cancer, detection for sarcopenia was more meaningful than cachexia. However, the prognostic significance of cachexia exceeded sarcopenia in advanced cancer.



Similar content being viewed by others
References
Arends J, Bachmann P, Baracos V, et al. ESPEN guidelines on nutrition in cancer patients. Clin Nutr. 2017;36(1):11–48.
Porporato PE. Understanding cachexia as a cancer metabolism syndrome. Oncogenesis. 2016;5:e200.
Mattox TW. Cancer cachexia: cause, diagnosis, and treatment. Nutr Clin Pract. 2017;32(5):599–606.
Inui A. Cancer anorexia-cachexia syndrome: current issues in research and management. CA Cancer J Clin. 2002;52(2):72–91.
Aoyagi T, Terracina KP, Raza A, Matsubara H, Takabe K. Cancer cachexia, mechanism and treatment. World J Gastrointest Oncol. 2015;7(4):17–29.
Fearon KC, Voss AC, Hustead DS, Cancer Cachexia Study Group. Definition of cancer cachexia: effect of weight loss, reduced food intake, and systemic inflammation on functional status and prognosis. Am J Clin Nutr. 2006;83(6):1345–50.
Fearon K, Strasser F, Anker SD, et al. Definition and classification of cancer cachexia: an international consensus. Lancet Oncol. 2011;12(5):489–95.
Kamarajah SK, Bundred J, Tan BHL. Body composition assessment and sarcopenia in patients with gastric cancer: a systematic review and meta-analysis. Gastric Cancer Off J Int Gastric Cancer Assoc Jpn Gastric Cancer Assoc. 2019;22(1):10–22.
Dobs AS, Boccia RV, Croot CC, et al. Effects of enobosarm on muscle wasting and physical function in patients with cancer: a double-blind, randomised controlled phase 2 trial. Lancet Oncol. 2013;14(4):335–45.
Antoun S, Baracos VE, Birdsell L, Escudier B, Sawyer MB. Low body mass index and sarcopenia associated with dose-limiting toxicity of sorafenib in patients with renal cell carcinoma. Ann Oncol. 2010;21(8):1594–8.
Thoresen L, Frykholm G, Lydersen S, et al. Nutritional status, cachexia and survival in patients with advanced colorectal carcinoma. Different assessment criteria for nutritional status provide unequal results. Clin Nutr. 2013;32(1):65–72.
Cruz-Jentoft AJ, Bahat G, Bauer J, et al. Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing. 2019;48(1):16–31.
Peterson SJ, Mozer M. Differentiating sarcopenia and cachexia among patients with cancer. Nutr Clin Pract. 2017;32(1):30–9.
Kvist H, Sjostrom L, Tylen U. Adipose tissue volume determinations in women by computed tomography: technical considerations. Int J Obes. 1986;10(1):53–67.
Prado CM, Lieffers JR, McCargar LJ, et al. Prevalence and clinical implications of sarcopenic obesity in patients with solid tumours of the respiratory and gastrointestinal tracts: a population-based study. Lancet Oncolol. 2008;9(7):629–35.
Zhuang CL, Huang DD, Pang WY, et al. Sarcopenia is an independent predictor of severe postoperative complications and long-term survival after radical gastrectomy for gastric cancer: analysis from a large-scale cohort. Medicine. 2016;95(13):e3164.
Zhuang CL, Shen X, Huang YY, et al. Myosteatosis predicts prognosis after radical gastrectomy for gastric cancer: a propensity score-matched analysis from a large-scale cohort. Surgery. 2019;166(3):297–304.
Zhuang CL, Zhang FM, Li W, et al. Associations of low handgrip strength with cancer mortality: a multicentre observational study. J Cachexia Sarcopenia Muscle. 2020;11(6):1476–86.
Chen LK, Liu LK, Woo J, et al. Sarcopenia in Asia: consensus report of the Asian Working Group for Sarcopenia. J Am Med Directors Assoc. 2014;15(2):95–101.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240(2):205–13.
Dunne RF, Loh KP, Williams GR, Jatoi A, Mustian KM, Mohile SG. Cachexia and sarcopenia in older adults with cancer: a comprehensive review. Cancers (Basel). 2019;11(12):1861.
Munhoz da Rocha Lemos Costa T, Costa FM, Jonasson TH, Moreira CA, Boguszewski CL, Borba VZC. Body composition and sarcopenia in patients with chronic obstructive pulmonary disease. Endocrine. 2018;60(1):95–102.
Bruggeman AR, Kamal AH, LeBlanc TW, Ma JD, Baracos VE, Roeland EJ. Cancer cachexia: beyond weight loss. J Oncol Pract. 2016;12(11):1163–71.
Vazeille C, Jouinot A, Durand JP, et al. Relation between hypermetabolism, cachexia, and survival in cancer patients: a prospective study in 390 cancer patients before initiation of anticancer therapy. Am J Clin Nutr. 2017;105(5):1139–47.
Chen LK, Lee WJ, Peng LN, et al. Recent advances in sarcopenia research in Asia: 2016 update from the Asian Working Group for Sarcopenia. J Am Med Directors Assoc. 2016;17(8):e761–7.
Biswas AK, Acharyya S. Understanding cachexia in the context of metastatic progression. Nat Rev Cancer. 2020;20(5):274–84.
McMillan DC. Systemic inflammation, nutritional status and survival in patients with cancer. Curr Opin Clin Nutr Metabolic Care. 2009;12(3):223–6.
Deng HY, Hou L, Zha P, Huang KL, Peng L. Sarcopenia is an independent unfavorable prognostic factor of non-small cell lung cancer after surgical resection: A comprehensive systematic review and meta-analysis. Eur J Surg Oncol J Eur Soc Surg Oncol Br Assoc Surg Oncol. 2019;45(5):728–35.
Icard P, Schussler O, Loi M, et al. Pre-disease and pre-surgery BMI, weight loss and sarcopenia impact survival of resected lung cancer independently of tumor stage. Cancers (Basel). 2012;12(2):266.
Marzetti E, Calvani R, Tosato M, et al. Sarcopenia: an overview. Aging Clin Exp Res. 2017;29(1):11–7.
Cruz-Jentoft AJ, Baeyens JP, Bauer JM, et al. Sarcopenia: European consensus on definition and diagnosis: report of the European Working Group on sarcopenia in older people. Age Ageing. 2010;39(4):412–23.
Martin L, Birdsell L, Macdonald N, et al. Cancer cachexia in the age of obesity: skeletal muscle depletion is a powerful prognostic factor, independent of body mass index. J Clin Oncol Off J Am Soc Clin Oncol. 2013;31(12):1539–47.
Miljkovic I, Zmuda JM. Epidemiology of myosteatosis. Curr Opin Clin Nutr Metabolic Care. 2010;13(3):260–4.
Addison O, Marcus RL, Lastayo PC, Ryan AS. Intermuscular fat: a review of the consequences and causes. Int J Endocrinol 2014;2014:309570.
Visser M, Goodpaster BH, Kritchevsky SB, et al. Muscle mass, muscle strength, and muscle fat infiltration as predictors of incident mobility limitations in well-functioning older persons. J Gerontol Ser A Biol Sci Med Sci. 2005;60(3):324–33.
Petersen KF, Befroy D, Dufour S, et al. Mitochondrial dysfunction in the elderly: possible role in insulin resistance. Science. 2003;300(5622):1140–2.
Acknowledgments
We thank the study participants and their families, whose help and participation made this work possible.
Funding
This work was supported by the National Key Research and Development Program: The National Natural Science Foundation of China (No. 81800795, 81770884), Shanghai Municipal Commission of Health and Family Planning (No.20184Y0301), the Key Technology of Palliative Care and Nursing for Cancer Patients (2017YFC1309200), the Zhejiang Provincial Health Department Medical Support Discipline—Nutrition (11-ZC24), the Wenzhou Municipal Science and Bureau (Y2020732).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Disclosures
The authors declare no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Zhuang, CL., Dong, QT., Shi, HP. et al. Cachexia Versus Sarcopenia in Clinical Characteristics and Prognostic Value After Radical Gastrectomy for Gastric Cancer: A Large-Scale Prospective Study. Ann Surg Oncol 29, 2348–2358 (2022). https://doi.org/10.1245/s10434-021-11084-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-021-11084-w