Abstract
Backgrounds
The optimal lymph node classification system for prognostic assessment in gastric adenocarcinoma (GAC) patients who undergo lymph node dissection remains unclear. Therefore, this study aimed to compare prognostic nomograms based on AJCC N stage, lymph node ratio (LNR), and log odds of metastatic lymph nodes (LODDS) to evaluate the prognosis and differentiate risk subgroups of patients with resected GAC.
Patients and Methods
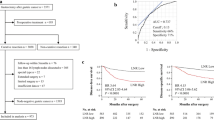
We collected 4633 patients with resected stage I–III GAC receiving chemotherapy from the Surveillance, Epidemiology, and End Results (SEER) database between 2004 and 2015. Independent prognostic factors were selected by Cox regression analyses, based on which nomograms were constructed. External validation was performed in 228 cases from Nanjing Drum Tower Hospital. Kaplan–Meier survival analysis was used to evaluate the effect of postoperative radiotherapy (PORT) for different lymph node classifications.
Results
Multivariate analysis indicated that age, grade, primary site, T stage, N stage, LNR, LODDS, and radiotherapy were independent predictors. Good discrimination power and high consistency of calibration plots were obtained from the LODDS system nomogram. The LODDS classification could more precisely differentiate risk subgroups and improve the discrimination of the resected GAC prognosis. A user-friendly webserver of LODDS system was built based on the nomogram for convenient clinical application.
Conclusions
The LODDS seems to be the most reliable lymph node classification in predicting the prognosis of patients with resected GAC and should be recommended in clinical prognostic assessment. Incorporating LODDS into the staging system will enable clinicians to more accurately predict prognosis and guide radiotherapy regimen decisions.




Similar content being viewed by others
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424.
Ikoma N, Das P, Hofstetter W, et al. Preoperative chemoradiation therapy induces primary-tumor complete response more frequently than chemotherapy alone in gastric cancer: analyses of the National Cancer Database 2006–2014 using propensity score matching. Gastric Cancer. 2018;21(6):1004–13.
Amin MB, Greene FL, Edge SB, et al. The Eighth Edition AJCC Cancer Staging Manual: continuing to build a bridge from a population-based to a more "personalized" approach to cancer staging. CA Cancer J Clin. Mar 2017;67(2):93-99.
Smith DD, Nelson RA, Schwarz RE. A comparison of five competing lymph node staging schemes in a cohort of resectable gastric cancer patients. Ann Surg Oncol. 2014;21(3):875–82.
Slidell MB, Chang DC, Cameron JL, et al. Impact of total lymph node count and lymph node ratio on staging and survival after pancreatectomy for pancreatic adenocarcinoma: a large, population-based analysis. Ann Surg Oncol. 2008;15(1):165–74.
Zhou R, Zhang J, Sun H, Liao Y, Liao W. Comparison of three lymph node classifications for survival prediction in distant metastatic gastric cancer. Int J Surg. 2016;35:165–71.
Cheraghlou S, Agogo GO, Girardi M. Evaluation of lymph node ratio association with long-term patient survival after surgery for node-positive merkel cell carcinoma. JAMA Dermatol. 2019;155(7):803–11.
Qiu MZ, Qiu HJ, Wang ZQ, et al. The tumor-log odds of positive lymph nodes-metastasis staging system, a promising new staging system for gastric cancer after D2 resection in China. PloS One. 2012;7(2):e31736.
Spolverato G, Ejaz A, Kim Y, et al. Prognostic performance of different lymph node staging systems after curative intent resection for gastric adenocarcinoma. Ann Surg. 2015;262(6):991–8.
Yu Y, Zhang P, Yao R, et al. Prognostic value of log odds of positive lymph nodes in node-positive lung squamous cell carcinoma patients after surgery: a SEER population-based study. Transl Lung Cancer Res. 2020;9(4):1285–301.
Balachandran VP, Gonen M, Smith JJ, DeMatteo RP. Nomograms in oncology: more than meets the eye. Lancet Oncol. 2015;16(4):e173-180.
Wang J, Dang P, Raut CP, et al. Comparison of a lymph node ratio-based staging system with the 7th AJCC system for gastric cancer: analysis of 18,043 patients from the SEER database. Ann Surg. 2012;255(3):478–85.
Marchet A, Mocellin S, Ambrosi A, et al. The ratio between metastatic and examined lymph nodes (N ratio) is an independent prognostic factor in gastric cancer regardless of the type of lymphadenectomy: results from an Italian multicentric study in 1853 patients. Ann Surg. 2007;245(4):543–52.
Siddiqui MM, Rais-Bahrami S, Turkbey B, et al. Comparison of MR/ultrasound fusion-guided biopsy with ultrasound-guided biopsy for the diagnosis of prostate cancer. JAMA. 2015;313(4):390–7.
Gupta S, Rohatgi A, Ayers CR, et al. Cardiorespiratory fitness and classification of risk of cardiovascular disease mortality. Circulation. 2011;123(13):1377–83.
Waddell T, Verheij M, Allum W, Cunningham D, Cervantes A, Arnold D. Gastric cancer: ESMO-ESSO-ESTRO clinical practice guidelines for diagnosis, treatment and follow-up. Eur J Surg Oncol. 2014;40(5):584–91.
Noh SH, Park SR, Yang HK, et al. Adjuvant capecitabine plus oxaliplatin for gastric cancer after D2 gastrectomy (CLASSIC): 5-year follow-up of an open-label, randomised phase 3 trial. Lancet Oncol. 2014;15(12):1389–96.
Smith DD, Schwarz RR, Schwarz RE. Impact of total lymph node count on staging and survival after gastrectomy for gastric cancer: data from a large US-population database. J Clin Oncol. 2005;23(28):7114–24.
Schwarz RE, Smith DD. Clinical impact of lymphadenectomy extent in resectable gastric cancer of advanced stage. Ann Surg Oncol. 2007;14(2):317–28.
Roder JD, Böttcher K, Busch R, Wittekind C, Hermanek P, Siewert JR. Classification of regional lymph node metastasis from gastric carcinoma. German Gastric Cancer Study Group Cancer. 1998;82(4):621–31.
Zhang N, Bai H, Deng J, et al. Impact of examined lymph node count on staging and long-term survival of patients with node-negative stage III gastric cancer: a retrospective study using a Chinese multi-institutional registry with Surveillance, Epidemiology, and End Results (SEER) data validation. Ann Transl Med. 2020;8(17):1075.
Jian-Hui C, Shi-Rong C, Hui W, et al. Prognostic value of three different lymph node staging systems in the survival of patients with gastric cancer following D2 lymphadenectomy. Tumour Biol. 2016;37(8):11105–13.
Yamashita K, Hosoda K, Ema A, Watanabe M. Lymph node ratio as a novel and simple prognostic factor in advanced gastric cancer. Eur J Surg Oncol. 2016;42(9):1253–60.
Marchet A, Mocellin S, Ambrosi A, et al. The prognostic value of N-ratio in patients with gastric cancer: validation in a large, multicenter series. Eur J Surg Oncol. 2008;34(2):159–65.
Fortea-Sanchis C, Martínez-Ramos D, Escrig-Sos J. The lymph node status as a prognostic factor in colon cancer: comparative population study of classifications using the logarithm of the ratio between metastatic and nonmetastatic nodes (LODDS) versus the pN-TNM classification and ganglion ratio systems. BMC Cancer. 2018;18(1):1208.
Xu J, Bian YH, Jin X, Cao H. Prognostic assessment of different metastatic lymph node staging methods for gastric cancer after D2 resection. World J Gastroenterol. 2013;19(12):1975–83.
Liu H, Deng J, Zhang R, Hao X, Jiao X, Liang H. The RML of lymph node metastasis was superior to the LODDS for evaluating the prognosis of gastric cancer. Int J Surg. 2013;11(5):419–24.
Sun Z, Xu Y, de Li M, et al. Log odds of positive lymph nodes: a novel prognostic indicator superior to the number-based and the ratio-based N category for gastric cancer patients with R0 resection. Cancer. 2010;116(11):2571–80.
Cao J, Yuan P, Ma H, et al. Log odds of positive lymph nodes predicts survival in patients after resection for esophageal cancer. Ann Thorac Surg. 2016;102(2):424–32.
Szczepanik AM, Paszko A, Szura M, Scully-Horner T, Kulig J. Alternative staging of regional lymph nodes in gastric cancer. Przeglad Gastroenterologiczny. 2016;11(3):145–9.
Smalley SR, Gunderson L, Tepper J, et al. Gastric surgical adjuvant radiotherapy consensus report: rationale and treatment implementation. Int J Radiat Oncol Biol Phys. 2002;52(2):283–93.
Ajani JA, Bentrem DJ, Besh S, et al. Gastric cancer version 2.2013: featured updates to the NCCN Guidelines. J Natl Compr Canc Netw. 2013;11(5):531–46.
Bang YJ, Kim YW, Yang HK, et al. Adjuvant capecitabine and oxaliplatin for gastric cancer after D2 gastrectomy (CLASSIC): a phase 3 open-label, randomised controlled trial. Lancet. 2012;379(9813):315–21.
Datta J, McMillan MT, Ruffolo L, et al. Multimodality therapy improves survival in resected early stage gastric cancer in the United States. Ann Surg Oncol. 2016;23(9):2936–45.
Acknowledgment
This work was funded by grants from the Fund for Distinguished Young Scholars of Jiangsu Province (No. BK20190001) and the Fundamental Research Funds for the Central Universities (No. 0214-14380497). The funding sources had no role in the study design, data collection, data analysis, data interpretation, or writing of the report.
Author information
Authors and Affiliations
Contributions
KYC analyzed and interpreted data and wrote and reviewed the manuscript. YW and NDW reviewed the manuscript. QL and JY prepared the data and reviewed the manuscript. JW and BRL designed the research, analyzed and interpreted the data, and reviewed the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Disclosure
The authors have no conflicts of interest.
Ethical Approval
Because the patients in the SEER database could not be identified, the analysis and reporting of the data in our study were exempt from review by the Ethics Board of Nanjing Drum Tower Hospital, The Affiliated Hospital of Nanjing University Medical School. The requirement for written informed consent to participate was waived. We were permitted to have Internet access to the database after our signed data-use agreement (http://seer.cancer.gov/data/sample-dua.html) was approved by the SEER administration. All patients from Nanjing Drum Tower Hospital read and signed the informed consent for surgery. The ethical committee and institutional review board of Nanjing Drum Tower Hospital approved this study.
Consent for Publication
This manuscript is approved by all authors for publication.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Che, K., Wang, Y., Wu, N. et al. Prognostic Nomograms Based on Three Lymph Node Classification Systems for Resected Gastric Adenocarcinoma: A Large Population-Based Cohort Study and External Validation. Ann Surg Oncol 28, 8937–8949 (2021). https://doi.org/10.1245/s10434-021-10299-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-021-10299-1