Abstract
Background
The application of splenic hilar lymph node (no. 10 LN) dissection (no. 10 LND) for proximal gastric cancer (PGC) remains controversial. This study aimed to investigate the clinical relevance of no. 10 LND from the perspective of long-term survival.
Methods
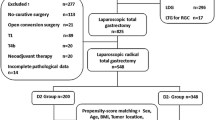
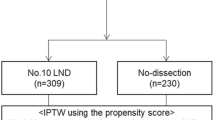
The main study population included 995 previously untreated patients who underwent laparoscopic radical total gastrectomy between January 2008 and December 2014. Of these 995 patients, 564 underwent no. 10 LND (no. 10D+ group) and the remaining 431 patients did not (no. 10D– group). Propensity score-matching was applied to reduce the effects of confounding factors. The study end points were overall survival (OS) and disease-free survival (DFS). Additionally, 39 patients who received neoadjuvant chemotherapy during the same period also were included as a separate population for analysis.
Results
The metastasis rate for no. 10 LN was 10.5 % (59/564). No significant differences were observed in intra- and postoperative complications nor in mortality between the no. 10D+ and no. 10D– groups (all P > 0.05). After 1:1 matching, the two groups were comparable in clinicopathologic characteristics. The no. 10D+ group had significantly better survival than the no. 10D– group (5-year OS: 63.3 % vs 52.2 %, P = 0.003; 5-year DFS: 60.4 % vs 48.1 %, P = 0.013). For the patients who received neoadjuvant chemotherapy, the 5-year OS rates in the no. 10D+ and no. 10D– groups were respectively 50.6 % and 31.3 % (P = 0.150) and the 5-year DFS rates were respectively 51.5 % and 31.3 % (P = 0.123).
Conclusions
Patients with untreated PGC may achieve the benefit of long-term survival from no. 10 LND. For patients with PGC who undergo neoadjuvant chemotherapy, no. 10 LND may not bring survival benefits. However, further validation with a large-sample study is needed.




Similar content being viewed by others
References
Zheng CH, Xu YC, Zhao G, et al. Safety and feasibility of laparoscopic spleen-preserving no. 10 lymph node dissection for locally advanced upper third gastric cancer: a prospective, multicenter clinical trial. Surg Endosc. 2020;34:5062–5073.
Watanabe M, Kinoshita T, Enomoto N, et al. Clinical significance of splenic hilar dissection with splenectomy in advanced proximal gastric cancer: an analysis at a single institution in Japan. World J Surg. 2016;40:1165–71.
Sasako M, McCulloch P, Kinoshita T, Maruyama K. New method to evaluate the therapeutic value of lymph node dissection for gastric cancer. Br J Surg. 1995;82:346–51.
Jeong O, Jung MR, Ryu SY. Clinicopathological features and prognostic impact of splenic hilar lymph node metastasis in proximal gastric carcinoma. Eur J Surg Oncol. 2019;45:432–8.
Ikeguchi M, Kaibara N. Lymph node metastasis at the splenic hilum in proximal gastric cancer. Am Surg. 2004;70:645–8.
Falk J, Carstens H, Lundell L, Albertsson M. Incidence of carcinoma of the oesophagus and gastric cardia: changes over time and geographical differences. Acta Oncol. 2007;46:1070–4.
Blot WJ, Devesa SS, Kneller RW, Fraumeni JF Jr. Rising incidence of adenocarcinoma of the esophagus and gastric cardia. JAMA. 1991;265:1287–9.
Ahn HS, Lee HJ, Yoo MW, et al. Changes in clinicopathological features and survival after gastrectomy for gastric cancer over a 20-year period. Br J Surg. 2011;98:255–60.
Ma Z, Shi G, Chen X, et al. Laparoscopic splenic hilar lymph node dissection for advanced gastric cancer: to be or not to be. Ann Transl Med. 2019;7:343.
Japanese Gastric Cancer A. Japanese gastric cancer treatment guidelines 2018 (5th edition). Gastric Cancer. 2021;24:1-21.
Japanese Gastric Cancer A. Japanese gastric cancer treatment guidelines 2014 (ver. 4). Gastric Cancer. 2017;20:1–19.
Japanese Gastric Cancer A. Japanese gastric cancer treatment guidelines 2010 (ver. 3). Gastric Cancer. 2011;14:113–23.
Yura M, Yoshikawa T, Otsuki S, et al. The therapeutic survival benefit of splenic hilar nodal dissection for advanced proximal gastric cancer invading the greater curvature. Ann Surg Oncol. 2019;26:829–35.
Maezawa Y, Aoyama T, Yamada T, et al. Priority of lymph node dissection for proximal gastric cancer invading the greater curvature. Gastric Cancer. 2018;21:569–72.
Huang CM, Zhang JR, Zheng CH, et al. A 346-case analysis for laparoscopic spleen-preserving no. 10 lymph node dissection for proximal gastric cancer: a single-center study. PLoS One. 2014;9:e108480.
Sano T, Sasako M, Mizusawa J, et al. Randomized controlled trial to evaluate splenectomy in total gastrectomy for proximal gastric carcinoma. Ann Surg. 2017;265:277–83.
Yamamoto M, Baba H, Kakeji Y, et al. Postoperative morbidity/mortality and survival rates after total gastrectomy, with splenectomy/pancreaticosplenectomy for patients with advanced gastric cancer. Hepatogastroenterology. 2004;51:298–302.
Wanebo HJ, Kennedy BJ, Winchester DP, et al. Role of splenectomy in gastric cancer surgery: adverse effect of elective splenectomy on long-term survival. J Am Coll Surg. 1997;185:177–84.
Yu W, Choi GS, Chung HY. Randomized clinical trial of splenectomy versus splenic preservation in patients with proximal gastric cancer. Br J Surg. 2006;93:559–63.
Csendes A, Burdiles P, Rojas J, et al. A prospective randomized study comparing D2 total gastrectomy versus D2 total gastrectomy plus splenectomy in 187 patients with gastric carcinoma. Surgery. 2002;131:401–7.
Schwarz RE. Spleen-preserving splenic hilar lymphadenectomy at the time of gastrectomy for cancer: technical feasibility and early results. J Surg Oncol. 2002;79:73–6.
Fang WL, Huang KH, Wu CW, et al. Combined splenectomy does not improve survival in radical total gastrectomy for advanced gastric cardia cancer. Hepatogastroenterology. 2012;59:1150–4.
Son T, Lee JH, Kim YM, et al. Robotic spleen-preserving total gastrectomy for gastric cancer: comparison with conventional laparoscopic procedure. Surg Endosc. 2014;28:2606–15.
Lu J, Huang CM, Zheng CH, et al. Major perioperative complications in laparoscopic spleen-preserving total gastrectomy for gastric cancer: perspectives from a high-volume center. Surg Endosc. 2016;30:1034–42.
Guo X, Peng Z, Lv X, et al. Randomized controlled trial comparing short-term outcomes of laparoscopic and open spleen-preserving splenic hilar lymphadenectomy for advanced proximal gastric cancer: an interim report. J Surg Oncol. 2018;118:1264–70.
Sakuramoto S, Kikuchi S, Futawatari N, et al. Laparoscopy-assisted pancreas- and spleen-preserving total gastrectomy for gastric cancer as compared with open total gastrectomy. Surg Endosc. 2009;23:2416–23.
Hyung WJ, Lim JS, Song J, et al. Laparoscopic spleen-preserving splenic hilar lymph node dissection during total gastrectomy for gastric cancer. J Am Coll Surg. 2008;207:e6-11.
Hur H, Jeon HM, Kim W. Laparoscopic pancreas- and spleen-preserving D2 lymph node dissection in advanced (cT2) upper-third gastric cancer. J Surg Oncol. 2008;97:169–72.
Li P, Huang CM, Zheng CH, et al. Laparoscopic spleen-preserving splenic hilar lymphadenectomy in 108 consecutive patients with upper gastric cancer. World J Gastroenterol. 2014;20:11376–83.
Jia-Bin W, Chang-Ming H, Chao-Hui Z, et al. Laparoscopic spleen-preserving No. 10 lymph node dissection for advanced proximal gastric cancer in left approach: a new operation procedure. World J Surg Oncol. 2012;10:241.
Huang CM, Chen QY, Lin JX, et al. Laparoscopic spleen-preserving no. 10 lymph node dissection for advanced proximal gastric cancer using a left approach. Ann Surg Oncol. 2014;21:2051.
Huang CM, Chen QY, Lin JX, et al. Huang's three-step maneuver for laparoscopic spleen-preserving no. 10 lymph node dissection for advanced proximal gastric cancer. Chin J Cancer Res. 2014;26:208–10.
Goto H, Tokunaga M, Sugisawa N, et al. Value of splenectomy in patients with Siewert type II adenocarcinoma of the esophagogastric junction. Gastric Cancer. 2013;16:590–5.
Huang CM, Chen T, Lin JX, et al. The effects of laparoscopic spleen-preserving splenic hilar lymphadenectomy on the surgical outcome of proximal gastric cancer: a propensity score-matched, case-control study. Surg Endosc. 2017;31:1383–92.
Smith DD, Schwarz RR, Schwarz RE. Impact of total lymph node count on staging and survival after gastrectomy for gastric cancer: data from a large US-population database. J Clin Oncol. 2005;23:7114–24.
Sakuramoto S, Sasako M, Yamaguchi T, et al. Adjuvant chemotherapy for gastric cancer with S-1, an oral fluoropyrimidine. N Engl J Med. 2007;357:1810–20.
Kong SH, Lee HJ, Ahn HS, et al. Stage migration effect on survival in gastric cancer surgery with extended lymphadenectomy: the reappraisal of positive lymph node ratio as a proper N-staging. Ann Surg. 2012;255:50–8.
Dicken BJ, Graham K, Hamilton SM, et al. Lymphovascular invasion is associated with poor survival in gastric cancer: an application of gene-expression and tissue-array techniques. Ann Surg. 2006;243:64–73.
Austin PC. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivariate Behav Res. 2011;46:399–424.
Japanese Gastric Cancer A. Japanese classification of gastric carcinoma: 3rd English edition. Gastric Cancer. 2011;14:101–12.
Kurokawa Y, Takeuchi H, Doki Y, et al. Mapping of lymph node metastasis from esophagogastric junction tumors: a prospective nationwide multicenter study. Ann Surg. 2019. https://doi.org/10.1097/SLA.0000000000003499.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–13.
Yang DM, Kim HC, Jin W, et al. 64 Multidetector-row computed tomography for preoperative evaluation of gastric cancer: histological correlation. J Comput Assist Tomogr. 2007;31:98–103.
Small WC, Mehard WB, Langmo LS, et al. Preoperative determination of the resectability of hepatic tumors: efficacy of CT during arterial portography. AJR Am J Roentgenol. 1993;161:319–22.
Kim HJ, Kim AY, Oh ST, et al. Gastric cancer staging at multi-detector row CT gastrography: comparison of transverse and volumetric CT scanning. Radiology. 2005;236:879–85.
Amin MB, Greene FL, Edge SB, et al. The Eighth Edition AJCC Cancer Staging Manual: continuing to build a bridge from a population-based to a more “personalized” approach to cancer staging. CA Cancer J Clin. 2017;67:93–9.
Wang G, Zhao J, Song Y, et al. Phase II study of adjuvant chemotherapy with S1 plus oxaliplatin for Chinese patients with gastric cancer. BMC Cancer. 2018;18:547.
Fuse N, Bando H, Chin K, et al. Adjuvant capecitabine plus oxaliplatin after D2 gastrectomy in Japanese patients with gastric cancer: a phase II study. Gastric Cancer. 2017;20:332–40.
Zhong Q, Chen QY, Xu YC, et al. Reappraise role of no. 10 lymphadenectomy for proximal gastric cancer in the era of minimal invasive surgery during total gastrectomy: a pooled analysis of 4 prospective trials. Gastric Cancer. 2021;24:245–57.
Lee CM, Cho JM, Jang YJ, et al. Should lymph node micrometastasis be considered in node staging for gastric cancer? The significance of lymph node micrometastasis in gastric cancer. Ann Surg Oncol. 2015;22:765–71.
Jeuck TL, Wittekind C. Gastric carcinoma: stage migration by immunohistochemically detected lymph node micrometastases. Gastric Cancer. 2015;18:100–8.
Liu K, Chen XZ, Zhang YC, et al. The value of spleen-preserving lymphadenectomy in total gastrectomy for gastric and esophagogastric junctional adenocarcinomas: a long-term retrospective propensity score-match study from a high-volume institution in China. Surgery. 2021;169:426–35.
Yang K, Zhang WH, Chen XZ, et al. Survival benefit and safety of no. 10 lymphadenectomy for gastric cancer patients with total gastrectomy. Medicine Baltimore. 2014;93:e158.
Cunningham D, Allum WH, Stenning SP, et al. Perioperative chemotherapy versus surgery alone for resectable gastroesophageal cancer. N Engl J Med. 2006;355:11–20.
Macdonald JS, Smalley SR, Benedetti J, et al. Chemoradiotherapy after surgery compared with surgery alone for adenocarcinoma of the stomach or gastroesophageal junction. N Engl J Med. 2001;345:725–30.
Bang YJ, Kim YW, Yang HK, et al. Adjuvant capecitabine and oxaliplatin for gastric cancer after D2 gastrectomy (CLASSIC): a phase 3 open-label, randomised controlled trial. Lancet. 2012;379:315–21.
Al-Batran SE, Homann N, Pauligk C, et al. Perioperative chemotherapy with fluorouracil plus leucovorin, oxaliplatin, and docetaxel versus fluorouracil or capecitabine plus cisplatin and epirubicin for locally advanced, resectable gastric or gastro-oesophageal junction adenocarcinoma (FLOT4): a randomised, phase 2/3 trial. Lancet. 2019;393:1948–57.
Acknowledgment
This study was supported by Scientific and Technological Innovation Joint Capital Projects of Fujian Province (2017Y9011, 2017Y9004, 2018Y9041), the Construction Project of Fujian Province Minimally Invasive Medical Center (No. [2017]171), the second batch of special support funds for Fujian Province innovation and entrepreneurship talents (2016B013), the Special Fund for Clinical Research of Wu Jieping Medical Foundation (No: 320.6750.17511), and the general project of sailing fund of Fujian Medical University (2017XQ1026). The authors are express their gratitude to the patients and their families for their support in this study.
Author information
Authors and Affiliations
Contributions
Conceptualization, JXL, PL, ZKW; Data Curation, ZKW, HLZ, YQH; Formal Analysis, ZKW, ML, RHT; Funding acquisition, CMH, CHZ, JWX, PL; Investigation, ZNH, JLL; Methodology, JXL, PL, ZKW; Project administration, PL, CMH, CHZ; Software, ZKW, JL, QYC, LLC; Supervision, PL, CMH, CHZ; Validation, CMH, CHZ, JWX, JBW; Visualization, ZKW, YQH; Writing Original Draft Preparation, JXL, ZKW; Writing Review and Editing, PL, CMH, CHZ. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Disclosure
There are no conflicts of interest.
Informed Consent
Signed informed consent was obtained from all patients before surgery. The Ethics Committee of Fujian Medical University Union Hospital approved the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Lin, JX., Wang, ZK., Huang, YQ. et al. Clinical Relevance of Splenic Hilar Lymph Node Dissection for Proximal Gastric Cancer: A Propensity Score-Matching Case-Control Study. Ann Surg Oncol 28, 6649–6662 (2021). https://doi.org/10.1245/s10434-021-09830-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-021-09830-1