Abstract
Background
The optimal time interval to define early recurrence (ER) among patients who underwent resection of gallbladder cancer (GBC) is not well defined. We sought to develop and validate a novel GBC recurrence risk (GBRR) score to predict ER among patients undergoing resection for GBC.
Patients and Methods
Patients who underwent curative-intent resection for GBC between 2000 and 2018 were identified from the US Extrahepatic Biliary Malignancy Consortium database. A minimum p value approach in the log-rank test was used to define the optimal cutoff for ER. A risk stratification model was developed to predict ER based on relevant clinicopathological factors and was externally validated.
Results
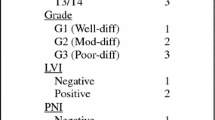
Among 309 patients, 103 patients (33.3%) had a recurrence at a median follow-up period of 15.1 months. The optimal cutoff for ER was defined at 12 months (p = 3.04 × 10−18). On multivariable analysis, T3/T4 disease (HR: 2.80; 95% CI 1.58–5.11) and poor tumor differentiation (HR: 1.91; 95% CI 1.11–3.25) were associated with greater hazards of ER. The GBRR score was developed using β-coefficients of variables in the final model, and patients were classified into three distinct groups relative to the risk for ER (12-month RFS; low risk: 88.4%, intermediate risk: 77.9%, high risk: 37.0%, p < 0.001). The external validation demonstrated good model generalizability with good calibration (n = 102: 12-month RFS; low risk: 94.2%, intermediate risk: 59.8%, high risk: 42.0%, p < 0.001). The GBRR score is available online at https://ktsahara.shinyapps.io/GBC_earlyrec/.
Conclusions
A novel online calculator was developed to help clinicians predict the probability of ER after curative-intent resection for GBC. The proposed web-based tool may help in the optimization of surveillance intervals and the counselling of patients about their prognosis.


Similar content being viewed by others
References
Siegel RL, Miller KD, Jemal A. Cancer statistics 2016. CA: Cancer J Clin. 2016;66(1):7–30.
Castro FA, Koshiol J, Hsing AW, Devesa SS. Biliary tract cancer incidence in the United States—Demographic and temporal variations by anatomic site. Int J Cancer. 2013;133(7):1664–71.
Ito H, Takahashi Y, Mise Y, Inoue Y, Ishizawa T, Saiura A. Locally advanced gallbladder cancer: Contemporary outcomes for aggressive surgical management. J Clin Oncol. 2018;36(4_suppl):420.
Sahara K, Tsilimigras DI, Maithel SK, et al. Survival benefit of lymphadenectomy for gallbladder cancer based on the therapeutic index: An analysis of the US extrahepatic biliary malignancy consortium. J Sur Oncol. 2020;121(3):503–10.
Engineer R, Goel M, Chopra S, et al. Neoadjuvant chemoradiation followed by surgery for locally advanced gallbladder cancers: a new paradigm. Ann Surg Oncol. 2016;23(9):3009–15.
Jarnagin WR, Ruo L, Little SA, et al. Patterns of initial disease recurrence after resection of gallbladder carcinoma and hilar cholangiocarcinoma: implications for adjuvant therapeutic strategies. Cancer. 2003;98(8):1689–700.
Kim WS, Choi DW, You DD, Ho CY, Heo JS, Choi SH. Risk factors influencing recurrence, patterns of recurrence, and the efficacy of adjuvant therapy after radical resection for gallbladder carcinoma. J Gastrointest Surg. 2010;14(4):679–87.
Margonis GA, Gani F, Buettner S, et al. Rates and patterns of recurrence after curative intent resection for gallbladder cancer: a multi-institution analysis from the US extra-hepatic biliary malignancy consortium. HPB. 2016;18(11):872–8.
Chan AWH, Zhong J, Berhane S, et al. Development of pre and post-operative models to predict early recurrence of hepatocellular carcinoma after surgical resection. J Hepatol. 2018;69(6):1284–93.
Groot VP, Gemenetzis G, Blair AB, et al. Defining and predicting early recurrence in 957 patients with resected pancreatic ductal adenocarcinoma. Ann Surg. 2019;269(6):1154–62.
Tsilimigras ID, Sahara K, Wu L, et al. Very early recurrence after liver resection for intrahepatic cholangiocarcinoma: considering alternative treatment approaches. JAMA Surg. 2020. https://doi.org/10.1001/jamasurg.2020.1973.
Network NCC. NCCN clinical practice guidelines iin oncology, hepatobiliary cancers. 2020; https://www.nccn.org/professionals/physician_gls/pdf/hepatobiliary.pdf.
Aloia TA, Járufe N, Javle M, et al. Gallbladder cancer: expert consensus statement. HPB. 2015;17(8):681–90.
Lee KJ, Carlin JB. Multiple imputation for missing data: fully conditional specification versus multivariate normal imputation. Am J Epidemiol. 2010;171(5):624–32.
Camp RL, Dolled-Filhart M, Rimm DL. X-tile: a new bio-informatics tool for biomarker assessment and outcome-based cut-point optimization. Clin Cancer Res. 2004;10(21):7252–9.
Facciabene A, Peng X, Hagemann IS, et al. Tumour hypoxia promotes tolerance and angiogenesis via CCL28 and T(reg) cells. Nature. 2011;475(7355):226–30.
Moro A, Mehta R, Sahara K, et al. The impact of preoperative CA19-9 and CEA on outcomes of patients with intrahepatic cholangiocarcinoma. Ann Surg Oncol. 2020;27(8):2888–901.
Sahara K, Merath K, Tsilimigras DI, et al. Conditional disease-free survival after curative-intent liver resection for neuroendocrine liver metastasis. J Surg Oncol. 2019;120(7):1087–95.
Shimizu Y, Ohtsuka M, Ito H, et al. Should the extrahepatic bile duct be resected for locally advanced gallbladder cancer? Surgery. 2004;136(5):1012–7.
Tsilimigras DI, Hyer JM, Paredes AZ, et al. The optimal number of lymph nodes to evaluate among patients undergoing surgery for gallbladder cancer: Correlating the number of nodes removed with survival in 6531 patients. J Surg Oncol. 2019;119(8):1099–107.
Lim H, Seo DW, Park DH, et al. Prognostic factors in patients with gallbladder cancer after surgical resection: analysis of 279 operated patients. J Clin Gastroenterol. 2013;47(5):443–8.
Kim Y, Amini N, Wilson A, et al. Impact of chemotherapy and external-beam radiation therapy on outcomes among patients with resected gallbladder cancer: a multi-institutional analysis. Ann Surg Oncol. 2016;23(9):2998–3008.
Xu XF, Xing H, Han J, et al. Risk factors, patterns, and outcomes of late recurrence after liver resection for hepatocellular carcinoma: a multicenter study from China. JAMA Surg. 2019;154(3):209–17.
Parasar K, Saluja SS, Varshney VK, Deepak B, Mishra PK. Early recurrence after laparoscopic radical cholecystectomy in a patient with gallbladder cancer. J Minimal Access Surg. 2019;15(1):74–6.
Ohtsuka M, Miyazaki M, Itoh H, et al. Routes of hepatic metastasis of gallbladder carcinoma. Am J Clin Pathol. 1998;109(1):62–8.
Creasy JM, Goldman DA, Gonen M, et al. Predicting residual disease in incidental gallbladder cancer: risk stratification for modified treatment strategies. J Gastrointest Surg. 2017;21(8):1254–61.
Ethun CG, Postlewait LM, Le N, et al. A novel pathology-based preoperative risk score to predict locoregional residual and distant disease and survival for incidental gallbladder cancer: a 10-institution study from the U.S. Extrahepatic Biliary Malignancy Consortium. Ann Surg Oncol. 2017;24(5):1343–50.
Hakeem AR, Papoulas M, Menon KV. The role of neoadjuvant chemotherapy or chemoradiotherapy for advanced gallbladder cancer—a systematic review. EurJ Surg Oncol. 2019;45(2):83–91.
Creasy JM, Goldman DA, Dudeja V, et al. Systemic chemotherapy combined with resection for locally advanced gallbladder carcinoma: surgical and survival outcomes. J Am Coll Surg. 2017;224(5):906–16.
Chaudhari VA, Ostwal V, Patkar S, et al. Outcome of neoadjuvant chemotherapy in “locally advanced/borderline resectable” gallbladder cancer: the need to define indications. HPB. 2018;20(9):841–7.
Cherkassky L, Jarnagin W. Selecting treatment sequence for patients with incidental gallbladder cancer: a neoadjuvant approach versus upfront surgery. Updates Surg. 2019;71(2):217–25.
Zamboni BA, Yothers G, Choi M, et al. Conditional survival and the choice of conditioning set for patients with colon cancer: an analysis of NSABP trials C-03 through C-07. J Clin Oncol 2010;28(15):2544–48.
Buettner S, Margonis GA, Kim Y, et al. Changing odds of survival over time among patients undergoing surgical resection of gallbladder carcinoma. Ann Surg Oncol. 2016;23(13):4401–9.
Margonis GA, Buettner S, Andreatos N, et al. Prognostic factors change over time after hepatectomy for colorectal liver metastases: a multi-institutional, international analysis of 1099 patients. Ann Surg. 2019;269(6):1129–37.
Spolverato G, Kim Y, Ejaz A, et al. Conditional probability of long-term survival after liver resection for intrahepatic cholangiocarcinoma: a multi-institutional analysis of 535 patients. JAMA Surg. 2015;150(6):538–45.
Bischof DA, Kim Y, Dodson R, et al. Conditional disease-free survival after surgical resection of gastrointestinal stromal tumors: a multi-institutional analysis of 502 patients. JAMA Surg. 2015;150(4):299–306.
Primrose JN, Fox RP, Palmer DH, et al. Capecitabine compared with observation in resected biliary tract cancer (BILCAP): a randomised, controlled, multicentre, phase 3 study. Lancet Oncol. 2019;20(5):663–73.
Acknowledgments
None.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
The authors declare that they have no conflict of interest to this work.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Sahara, K., Tsilimigras, D.I., Kikuchi, Y. et al. Defining and Predicting Early Recurrence after Resection for Gallbladder Cancer. Ann Surg Oncol 28, 417–425 (2021). https://doi.org/10.1245/s10434-020-09108-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-020-09108-y