Abstract
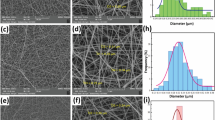
The ideal wound dressing should adequately protect the wound from bacterial infection and provide a suitable healing environment for the wound. Thus, we prepared a biodegradable functional nanofiber dressing with good antibacterial and biocompatibility by electrospinning technology. The average diameter of the dressing was 354 ± 185 nm, and the porosity was 93.27%. Scanning electron microscopy (SEM) showed that the dressing was smooth without beading. It was also characterized by Fourier-transform infrared spectroscopy (FTIR) and X-ray diffraction (XRD). The wettability and water vapor permeability of the dressing were tested; the results showed that the dressing had good wettability and permeability. The ability of drug release indicates that continuous release over a period of time is beneficial to wound healing. Finally, the antibacterial effect and in vivo pharmacodynamic evaluation of AS/CS/PLA nanofiber dressing were studied; the result showed that it had significant antibacterial activity and the ability to promote wound healing.
Graphical Abstract











Similar content being viewed by others
Data Availability
The authors confirm that the data supporting the findings of this study are available within the article.
References
He S, Jiang L, Liu J, Zhang J, Shao W. Electrospun PVA/gelatin based nanofiber membranes with synergistic antibacterial performance. Colloids Surfaces A Physicochem Eng Asp. 2022;637:128196.
Nandhini SN, Sisubalan N, Vijayan A, et al. Recent advances in green synthesized nanoparticles for bactericidal and wound healing applications. Heliyon. 2023;9(2):e13128.
Hamdan S, Pastar I, Drakulich S, et al. Nanotechnology-driven therapeutic interventions in wound healing: potential uses and applications. ACS Central Sci. 2017;3(3):163–75.
Amiri N, Golin AP, Jalili RB, et al. Roles of cutaneous cell-cell communication in wound healing outcome: an emphasis on keratinocyte-fibroblast crosstalk. Exp Dermatol. 2022;31(4):475–84.
Dobrovol’Skaya IP, Yudin VE, Popryadukhin PV, et al. In vivo study of the nanofiber-based composite wound dressing intended for treatment of deep skin wounds. J Appl Cosmetol. 2016;34(1–2):1–8.
Wang FD, Hu S, Jia QX, et al. Advances in electrospinning of natural biomaterials for wound dressing[J]. J Nanomater. 2020;2020:1–14.
Hickman DA, Pawlowski CL, Sekhon UDS, Marks J, Gupta AS. Biomaterials and advanced technologies for hemostatic management of bleeding. Adv Mater. 2018;30(4):10.
Floyd CT, Rothwell SW, Martin R, Risdahl J, Olson CE. A salmon thrombin-fibrinogen dressing controls hemorrhage in a swine model compared to standard kaolin-coated gauze. J Spec Oper Med. 2012;12(1):49–55.
Vigani B, Rossi S, Sandri G, Bonferoni MC, Caramella CM, Ferrari F. Hyaluronic acid and chitosan-based nanosystems: a new dressing generation for wound care. Expert Opin Drug Deliv. 2019;16(7):715–40.
Villarreal-Gómez LJ, Cornejo-Bravo JM, Vera-Graziano R, Grande D. Electrospinning as a powerful technique for biomedical applications: a critically selected survey. J Biomater Sci Polym Ed. 2016;27(2):157–76.
Boateng J, Catanzano O. Advanced therapeutic dressings for effective wound healing–a review. J Pharm Sci. 2015;104(11):3653–80.
Bruggeman KF, Williams RJ, Nisbet DR. Dynamic and responsive growth factor delivery from electrospun and hydrogel tissue engineering materials. Adv Healthc Mater. 2018;7(1):10.
Mulholland EJ. Electrospun biomaterials in the treatment and prevention of scars in skin wound healing. Front Bioeng Biotechnol. 2020;8:481.
Ambekar RS, Kandasubramanian B. Advancements in nanofibers for wound dressing: a review. Eur Polym J. 2019;117:304–36.
Thenmozhi S, Dharmaraj N, Kadirvelu K, et al. Electrospun nanofibers: new generation materials for advanced applications. Mater Sci Eng B. 2017;217:36–48.
Fatehi P, Abbasi M. Medicinal plants used in wound dressings made of electrospun nanofibers. J Tissue Eng Regen Med. 2020;14(11):1527–48.
Haider A, Haider S, Kang I-K. A comprehensive review summarizing the effect of electrospinning parameters and potential applications of nanofibers in biomedical and biotechnology. Arab J Chem. 2018;11(8):1165–88.
Xue J, Xie J, Liu W, Xia Y. Electrospun nanofibers: new concepts, materials, and applications. Acc Chem Res. 2017;50(8):1976–87.
Abrigo M, McArthur SL, Kingshott P. Electrospun nanofibers as dressings for chronic wound care: advances, challenges, and future prospects. Macromol Biosci. 2014;14(6):772–92.
Ding Y, Li W, Zhang F, et al. Electrospun fibrous architectures for drug delivery, tissue engineering and cancer therapy. Adv Func Mater. 2019;29:1802852.
Bano I, Arshad M, Yasin T, Ghauri MA, Younus M. Chitosan: a potential biopolymer for wound management. Int J Biol Macromol. 2017;102:380–3.
Takei T, Danjo S, Sakoguchi S, et al. Autoclavable physically-crosslinked chitosan cryogel as a wound dressing. J Biosci Bioeng. 2018;125(4):490–5.
Dang Q, Liu K, Liu C, et al. Preparation, characterization, and evaluation of 3,6-0-N-acetylethylenediamine modified chitosan as potential antimicrobial wound dressing material. Carbohydr Polym. 2018;180(1):1–12.
Sheik S, Sheik S, Nairy R, et al. Study on the morphological and biocompatible properties of chitosan grafted silk fibre reinforced PVA films for tissue engineering applications. Int J Biol Macromol. 2018;116:45–53.
Bowei WANG, Rui MA, Fan WU, et al. Preparation and characterization of graphene oxide-sodium alginate-chitosan composite scaffold[J]. Chem J Chin Univ. 2020;41(9):2099–106.
Levengood SL, Erickson AE, Chang FC, Zhang M. Chitosan-poly(caprolactone) nanofibers for skin repair. J Mater Chem B. 2017;5(9):1822–33.
Adeli H, Khorasani MT, Parvazinia M. Wound dressing based on electrospun PVA/chitosan/starch nanofibrous mats: fabrication, antibacterial and cytocompatibility evaluation and in vitro healing assay. Int J Biol Macromol. 2019;122:238–54.
Du SQ, Wang JC, Peng XQ, et al. Fabrication and mechanical properties of biodegradable jute/polylactic acid composites. J Shanghai Jiaotong Univ (Chin Ed). 2019;53(11):1335–41.
Liu SQ, Zheng YZ, Wu ZZ, et al. Preparation and characterization of aspirin-loaded polylactic acid/graphene oxide biomimetic nanofibrous scaffolds. Polymer. 2020;211:123093.
Yang ZJ, Sun C, Wang LC, et al. Novel Poly(l-lactide)/graphene oxide films with improved mechanical flexibility and antibacterial activity. J Colloid Interface Sci. 2017;507:344–52.
AlinezhadSardareh E, Shahzeidi M, SalmanifardArdestani MT, et al. Antimicrobial activity of blow spun PLA/gelatin nanofibers containing green synthesized silver nanoparticles against wound infection-causing bacteria. Bioengineering (Basel). 2022;9(10):518.
Lappe S, Mulac D, Langer K. Polymeric nanoparticles - influence of the glass transition temperature on drug release. Int J Pharm. 2017;517(1–2):338–47.
Sun H, Pang X, Li J. Research progress on biological activity of astragaloside IV. Chin Pharm. 2011;22(7):657–61.
Li L, Hou XF, Xu RL, et al. Research review on the pharmacological effects of astragaloside IV. Fundam Clin Pharmacol. 2017;31(1):17–36.
Yu JW, Guo MF, Zhang J, et al. Effects of astragaloside on astrocyte inflammation induced by lipopolysaccharide in vitro and its mechanism. Chin J Microbiol Immunol. 2018;38(11):829–34.
Zheng XT, Gan HY, Li L, et al. Astragaloside IV inhibits inflammation after cerebral ischemia in rats by promoting M2-type polarization of microglia/macrophages. J Zhejiang Univ: Med Sci. 2020;49(6):679–86.
Wang DD, Zhang LZ, Pang CJ, et al. Astragaloside IV promotes keratinocyte proliferation and migration through upregulating lncRNA H19 recruited ILF3 to enhance the stability of CDK4 mRNA. Kaohsiung J Med Sci. 2023;39(8):811–23.
Huang NC, Dai LG, Kang LY, et al. Beneficial effects of astragaloside IV-treated and 3-dimensional-cultured endothelial progenitor cells on angiogenesis and wound healing. Ann Plast Surg. 2021;86(2S Suppl 1):S3–12.
Yue Y, Liu X, Pang L, et al. Astragalus polysaccharides/PVA nanofiber membranes containing astragaloside IV-loaded liposomes and their potential use for wound healing. Evid Based Complement Alternat Med. 2022;2022:9716271.
Dingman. Preparation and properties of chitosan / polylactic acid drug-loaded nanofibers [ D ]. Anhui: Hefei University of Technology; 2012.
Liu YP, Zuo LN, Ke JX, et al. Optimization of preparation for electrospun nanofifiber membranes loaded with shikonin nanocrystals. Chin J Pharm Ind. 2022; 5(4): 515–521.563.
Huang Z, Xu L. Preparation of astragaloside IV nanomicelles and transport study in Caco-2 cell model. Northwest J Pharm. 2022;37(2):94–8.
HU Bingyu. Preparation and properties of chitosan-based nanofiber / foam composite dressing [ D ].Wuhan Textile University; 2020.
Wang P. Preparation of novel photocatalysts and photodegradable plastic films. Henan: Zhengzhou University; 2015.
Bazbouz MB, Liang H, Tronci G. A UV-cured nanofibrous membrane of vinylbenzylated gelatin-poly(ɛ-caprolactone) dimethacrylate co-network by scalable free surface electrospinning. Mater Sci Eng C Mater Biol Appl. 2018;91:541–55.
Bhowmick S, Scharnweber D, Koul V. Co-cultivation of keratinocyte-human mesenchymal stem cell (hMSC) on sericin loaded electrospun nanofibrous composite scaffold (cationic gelatin/hyaluronan/chondroitin sulfate) stimulates epithelial differentiation in hMSCs: in vitro study. Biomaterials. 2016;88:83–96.
Salerno A, Oliviero M, Di Maio E, Iannace S. Thermoplastic foams from zein and gelatin. Int Polym Proc. 2007;22(5):480–8.
Yang Q, Guo J, Liu SX, et al. Molecular action and bioactivity characterization of electrospun chitosan- polylactic acid composite nerve conduit. Chinese J Compos Mater. 2019;38(6):1950–9.
Gu SY, Wang ZM, Ren J, et al. Electrospinning of gelatin and gelatin/poly(l-lactide) blend and its characteristics for wound dressing. Mater Sci Eng C. 2009;29:1822–8.
Gartner H, Li Y, Almenar E. Improved wettability and adhesion of polylactic acid/chitosan coating for bio-based multilayer film development. Appl Surf Sci. 2015;332:488–93.
Pal AK, Katiyar V. Theoretical and analyzed data related to thermal degradation kinetics of poly (L-lactic acid)/chitosan-grafted-oligo L-lactic acid (PLA/CH-g-OLLA) bionanocomposite films. Data Brief. 2016;10:304–11.
Tort S, Demiröz FT, Coşkun Cevher Ş, Sarıbaş S, Özoğul C, Acartürk F. The effect of a new wound dressing on wound healing: biochemical and histopathological evaluation. Burns. 2020;46(1):143–55.
Fu DW, Yan YH. Degradation performance of biological barrier membrane. J Wuhan Univ Technol. 2005;27(10):26–9.
Tu Y, Peng F, André AA, Men Y, Srinivas M, Wilson DA. Biodegradable hybrid stomatocyte nanomotors for drug delivery. ACS Nano. 2017;11(2):1957–63.
Han W. Preparation of the degradable free-standing polylactic acid/chitosan based films. Jiangsu: Southeast University; 2018.
Zhang D, Cai G, Mukherjee S, et al. Elastic, persistently moisture-retentive, and wearable biomimetic film inspired by fetal scarless repair for promoting skin wound healing. ACS Appl Mater Interfaces. 2020;12(5):5542–56.
Funding
This experiment was supported by project of Guizhou Traditional Chinese Medicine Administration (QZYY-2020–039), Guizhou Provincial Health Commission Science and Technology Fund Project (zwkj2022-234), and Young Scientific and Technological Talents Growth Project of Guizhou Provincial Department of Education (Qian Jiao He KY Zi(2018)205).
Author information
Authors and Affiliations
Contributions
All authors contributed to the data analysis, drafting, and analysis; made rigorous revisions to the paper; gave final approval for publication; and agreed to take responsibility for all aspects of the work. ZL conceived and designed the experiment and wrote the paper. ZL and YL conducted the experiment. GZ and WW conducted the analysis of Fourier infrared spectroscopy and X-ray diffraction, and XC reviewed the manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Liu, Z., Lv, Y., Zheng, G. et al. Chitosan/Polylactic Acid Nanofibers Containing Astragaloside IV as a New Biodegradable Wound Dressing for Wound Healing. AAPS PharmSciTech 24, 202 (2023). https://doi.org/10.1208/s12249-023-02650-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1208/s12249-023-02650-4