Abstract
Objective
Stroke presenting as dizziness is a diagnostic challenge in frontline settings, given the multitude of benign conditions that present similarly. The risk of stroke after episodic dizziness is unknown, leading to divergent guidance on optimal workup and management. Prior TIA risk scores have shown a history of dizziness is a negative predictor of subsequent stroke. Our objective was to assess the subsequent stroke risk within 90 days following emergency department assessment (ED) for isolated dizziness diagnosed as TIA during the index visit.
Methods
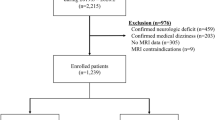
We conducted prospective, multicenter cohort studies at 13 Canadian EDs over 11 years. We enrolled patients diagnosed with TIA and compared patients with isolated dizziness to those with other neurological deficits. Our primary outcome was subsequent stroke within 90 days. Secondary outcomes were subsequent stroke within 2, 7, and 30 days, respectively, as well as subsequent TIA within 90 days.
Results
Only 4/483 (0.8%) patients with isolated dizziness had a stroke within 90 days compared to 320/11024 (2.9%) of those with any focal neurological sign or symptom (RR 0.29, 95% CI 0.11–0.76). Over the first 90 days, the two groups differ significantly in their probability of stroke (p = 0.007). Subsequent TIA was also significantly less common in the isolated dizziness group (1.7% vs. 5.6%, p = 0.001) with a relative risk of 0.30 (95% CI 0.15–0.60).
Conclusion
The risk of subsequent stroke following ED presentation for TIA is low when the presenting symptoms are isolated dizziness.
Résumé
Objectif
Les accidents vasculaires cérébraux (AVC) se présentant sous forme de vertiges constituent un défi diagnostique en première ligne, étant donné la multitude d'affections bénignes qui se présentent de la même manière. Le risque d'accident vasculaire cérébral (AVC) après des vertiges épisodiques est inconnu, ce qui donne lieu à des conseils divergents sur le bilan et la prise en charge optimaux. Des scores de risque d'AIT antérieurs ont montré que des antécédents de vertiges sont un facteur prédictif négatif d'accident vasculaire cérébral ultérieur. Notre objectif était d'évaluer le risque ultérieur d'accident vasculaire cérébral (AVC) dans les 90 jours suivant l'évaluation aux urgences d'un étourdissement isolé diagnostiqué comme un AIT lors de la visite de référence.
Méthodes
Nous avons mené des études de cohorte prospectives multicentriques dans 13 services d'urgence canadiens pendant 11 ans. Nous avons recruté des patients ayant reçu un diagnostic d'AIT et avons comparé les patients présentant des vertiges isolés à ceux présentant d'autres déficits neurologiques. Nous avons inscrit des patients ayant reçu un diagnostic d’AIT et comparé des patients ayant des étourdissements isolés à ceux présentant d’autres déficits neurologiques. Notre résultat primaire était l'AVC subséquent dans les 90 jours. Les résultats secondaires étaient l'AVC subséquent dans les 2, 7 et 30 jours, respectivement, ainsi que l'AIT subséquent dans les 90 jours.
Résultats
Seuls 4/483 (0,8 %) des patients présentant des vertiges isolés ont eu un AVC dans les 90 jours, contre 320/11 024 (2,9 %) de ceux présentant un signe ou symptôme neurologique focal (RR 0,29, IC 95 % 0,11-0,76). Au cours des 90 premiers jours, les deux groupes diffèrent significativement en termes de probabilité d'AVC (p = 0,007). L'AIT ultérieur était également significativement moins fréquent dans le groupe des vertiges isolés (1,7 % contre 5,6 %, p = 0,001) avec un risque relatif de 0,30 (IC 95 % 0,15-0,60).
Conclusions
Le risque d'AVC ultérieur après une présentation aux urgences pour un AIT est faible lorsque les symptômes présentés sont des étourdissements isolés.

Similar content being viewed by others
References
Newman-Toker DE, Moy E, Valente E, et al. Missed diagnosis of stroke in the emergency department: a cross-sectional analysis of a large population-based sample. Diagnosis (Berl). 2014;1:155–66.
Tarnutzer AA, Lee SH, Robinson KA, et al. ED misdiagnosis of cerebrovascular events in the era of modern neuroimaging: a meta-analysis. Neurology. 2017;88:1468–77.
Newman-Toker DE, Edlow JA. TiTrATE: a novel, evidence-based approach to diagnosing acute dizziness and vertigo. Neurol Clin. 2015;33:577–99 (viii).
Nadarajan V, Perry RJ, Johnson J, et al. Transient ischaemic attacks: mimics and chameleons. Pract Neurol. 2014;14:23–31.
Welgampola MS, Young AS, Pogson JM, et al. Dizziness demystified. Pract Neurol. 2019;19:492–501.
Paul NL, Simoni M, Rothwell PM, et al. Transient isolated brainstem symptoms preceding posterior circulation stroke: a population-based study. Lancet Neurol. 2013;12:65–71.
Kim HA, Oh EH, Choi SY, et al. Transient vestibular symptoms preceding posterior circulation stroke: a prospective multicenter study. Stroke J Cereb Circul. 2021;52:e224–8.
Perry JJ, Sharma M, Sivilotti ML, et al. A prospective cohort study of patients with transient ischemic attack to identify high-risk clinical characteristics. Stroke J Cereb Circul. 2014;45:92–100.
Perry JJ, Sivilotti MLA, Emond M, et al. Prospective validation of Canadian TIA Score and comparison with ABCD2 and ABCD2i for subsequent stroke risk after transient ischaemic attack: multicentre prospective cohort study. BMJ (Clin Res Ed). 2021;372:n49.
Meschia JF, Brott TG, Chukwudelunzu FE, et al. Verifying the stroke-free phenotype by structured telephone interview. Stroke J Cereb Circul. 2000;31:1076–80.
Jones WJ, Williams LS, Meschia JF. Validating the Questionnaire for Verifying Stroke-Free Status (QVSFS) by neurological history and examination. Stroke J Cereb Circul. 2001;32:2232–6.
The World Health Organization MONICA Project (monitoring trends and determinants in cardiovascular disease): a major international collaboration. WHO MONICA Project Principal Investigators. J Clin Epidemiol. 1988;41:105–114.
Kerber KA, Brown DL, Lisabeth LD, et al. Stroke among patients with dizziness, vertigo, and imbalance in the emergency department: a population-based study. Stroke J Cereb Circul. 2006;37:2484–7.
Norrving B, Magnusson M, Holtas S. Isolated acute vertigo in the elderly; vestibular or vascular disease? Acta Neurol Scand. 1995;91:43–8.
Wu CM, McLaughlin K, Lorenzetti DL, et al. Early risk of stroke after transient ischemic attack: a systematic review and meta-analysis. Arch Intern Med. 2007;167:2417–22.
Choi JH, Park MG, Choi SY, et al. Acute transient vestibular syndrome: prevalence of stroke and efficacy of bedside evaluation. Stroke J Cereb Circul. 2017;48:556–62.
Acknowledgements
The authors thank the hundreds of physicians who completed our data collection forms and all the emergency department nurses, and clerks at the 13 study sites for their cooperation with the study. We also thank the following research personnel at the study hospitals: Ottawa Hospital–Civic Campus and General Campus, Ottawa, Ontario (Rebecca Briscoe, Renée Labreche, Natalie Bilodeau, Tara Leach, Sarai Cohn-Kalter, Jane Sutherland, Juanita Wilzer, Ruth Glenwright, Carly O’Brien, Kathryn Madill, Alana Mistry, Kelly Smith, Connor Sheehan); Kingston General Hospital and Hotel Dieu Hospital, Kingston, Ontario (Jane Reid, Vlad Latiu, Jessica Montagner, Nicole O’Callaghan); Hôpital de L’Enfant-Jésus, Quebec City, Quebec (Suzy Lavoie); Hamilton Health Sciences Centre (General, and Henderson Sites), Hamilton, Ontario (Natasha Clayton); Montfort Hospital, Ottawa, Ontario (Christine Nadia Compas); Vancouver General Hospital, Vancouver, British Columbia (Vi Ho); Sacré Coeur Hospital, Montreal, Quebec (Chantal Lanthier); Sunnybrook Health Sciences Centre, Toronto, Ontario (Joanna Yeung); Queensway Carleton Hospital, Ottawa, Ontario (Karen Lemay, Katie Girimonte). We thank our colleagues at the Ottawa Hospital Research Institute (Sheryl Domingo, My-Linh Tran and Angela Marcantonio) for their assistance with this project. We thank David Newman-Toker for his thoughtful input and helpful discussions.
Funding
Canadian Institutes of Health Research. The funder had no role in the study design; in the collection, analysis, and interpretation of data; in the writing of the report; and in the decision to submit the article for publication. Researchers are independent from funders and all authors, external and internal, had full access to all of the data (including statistical reports and tables) in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Author information
Authors and Affiliations
Contributions
The author contributions were as follows: JP conceived the idea and AB prepared the manuscript. M-JN assisted with the statistical analysis. All co-authors contributed to revising the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Dr. Perry is supported by a mid-career award from the Heart and Stroke Foundation of Ontario. Dr. Lee is supported by the Schwartz/Reisman Emergency Medicine Institute Inaugural Research Chair in Geriatric Emergency Medicine. No other relationships or activities appear to have influenced the submitted work.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Bery, A.K., Sharma, M., Nemnom, MJ. et al. Risk of stroke is low after transient ischemic attack presentation with isolated dizziness. Can J Emerg Med 24, 844–852 (2022). https://doi.org/10.1007/s43678-022-00391-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43678-022-00391-0