Abstract
Background
Traditional principles for successful outcomes in Total Hip Arthroplasty (THA) have relied largely on placing the socket in the native position and trying to restore static anatomical femoral parameters gauged on X-rays or intra-operative measurement. Stability is conventionally achieved by making appropriate changes during the time of trial reduction. Post-operative complications of dislocation and significant Limb Length Discrepancy (LLD) requiring foot wear modification represents opposite ends of the spectrum from a biomechanical perspective and these continue to be relatively high. A move towards giving more importance to functional dynamic parameters rather than static anatomical parameters and less reliance on stability testing at trial reduction is warranted.
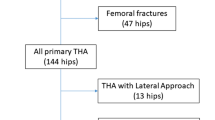
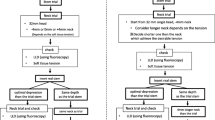
Methods
Intraoperative 3D functional balancing of THA without stability testing at trial reduction was practiced in all subjects undergoing THA in our unit from April 2014. To date 1019 patients have had their hips replaced with the same technique. They were followed up till April 2020 for post-operative complications of dislocation and significant LLD needing footwear modification. A secondary cohort of 114 patients from 1st January to December 31st 2017 within this primary group were analyzed clinically and radiologically to ascertain the implications of functional 3D balancing on X-ray parameters, clinical outcome scores (Harris Hip Score and Oxford Hip Score), ability to squat, and subtle subjective post-operative perception of limb lengthening (POPLL).
Results
In the primary group of 1019 patients, there were only two dislocations and no patient needed footwear modification for LLD. In the detailed analysis of the secondary cohort of 114 patients, the correlation with restoration of static radiological parameters was inconsistent. 40 patients could not squat and 4 patients had subtle subjective post-operative perceived limb lengthening (POPLL). Measured outcomes such as HHS and OHS were improved in all patients with significant statistical significance (P < 0.001).
Conclusion
This study underlines the fact that more importance must be given to functional dynamic parameters by 3D balancing of the THA and not on static anatomical X-rays parameters and stability testing during trial reduction. This represents a paradigm shift in the evolution of total hip arthroplasty.
Level of Evidence
A Level II study. (Data collected from the ongoing prospective study) (http://www.spine.org/Documents/LevelsofEvidenceFinal.pdf).







Similar content being viewed by others
References
Charnley, J. (1979). Hip sockets: Theory low friction arthroplasty of the hip (pp. 91–106). Springer.
Houcke, J. V., Khanduja, V., Pattyn, C., & Audenaert, E. (2017). The history of biomechanics in total hip arthroplasty. Indian Journal of Orthopaedics, 51(4), 359–367. https://doi.org/10.4103/ortho.IJOrtho_280_17
Flecher, X., Ollivier, M., & Argenson, J. N. (2016). Lower limb length and offset in total hip arthroplasty. Orthopaedics and Traumatology, 102(1), S9–S20. https://doi.org/10.1016/j.otsr.2015.11.001
Keršič, M., Dolinar, D., Antolič, V., & Mavčič, B. (2014). The impact of leg length discrepancy on clinical outcome of total hip arthroplasty: Comparison of four measurement methods. Journal of Arthroplasty, 29(1), 137–141. https://doi.org/10.1016/j.arth.2013.04.004
Fujimaki, H., Inaba, Y., Kobayashi, N., Tezuka, T., Hirata, Y., & Saito, T. (2013). Leg length discrepancy and lower limb alignment after total hip arthroplasty in unilateral hip osteoarthritis patients. Journal of Orthopaedic Science, 18(6), 969–976. https://doi.org/10.1007/s00776-013-0457-3
Tezuka, T., Heckmann, N. D., Bodner, R. J., & Dorr, L. D. (2019). Functional safe zone is superior to the lewinnek safe zone for total hip arthroplasty: why the lewinnek safe zone is not always predictive of stability. The Journal of Arthroplasty, 34(1), 3–8. https://doi.org/10.1016/j.arth.2018.10.034
Ike, H., Dorr, L. D., Trasolini, N., Stefl, M., McKnight, B., & Heckmann, N. (2018). Spine-pelvis-hip relationship in the functioning of a total hip replacement. The Journal of Bone and Joint Surgery, 100(18), 1606–1615. https://doi.org/10.2106/jbjs.17.00403
Bose, V. C., & Baruah, B. D. (2010). Resurfacing arthroplasty of the hip for avascular necrosis of the femoral head: A minimum follow-up of four years. The Journal of Bone and Joint Surgery British Volume, 92(7), 922–928. https://doi.org/10.1302/0301-620x.92b7.23639
Esposito, C. I., Miller, T. T., Kim, H. J., Barlow, B. T., Wright, T. M., Padgett, D. E., et al. (2016). Does degenerative lumbar spine disease influence femoroacetabular flexion in patients undergoing total hip arthroplasty? Clinical Orthopaedics and Related Research, 474(8), 1788–1797. https://doi.org/10.1007/s11999-016-4787-2
Onggo, J. R., Nambiar, M., Onggo, J. D., Phan, K., Ambikaipalan, A., Babazadeh, S., et al. (2020). Clinical outcomes and complication profile of total hip arthroplasty after lumbar spine fusion: A meta-analysis and systematic review. European Spine Journal, 29(2), 282–294. https://doi.org/10.1007/s00586-019-06201-z
Sultan, A. A., Khlopas, A., Piuzzi, N. S., Chughtai, M., Sodhi, N., & Mont, M. A. (2018). The impact of spino-pelvic alignment on total hip arthroplasty outcomes: A critical analysis of current evidence. Journal of Arthroplasty, 33(5), 1606–1616. https://doi.org/10.1016/j.arth.2017.11.021
Lewinnek, G. E., Lewis, J. L., Tarr, R., Compere, C. L., & Zimmerman, J. R. (1978). Dislocations after total hip-replacement arthroplasties. Journal of Bone and Joint Surgery, 60(2), 217–220.
Kanawade, V., Dorr, L. D., & Wan, Z. (2014). Predictability of acetabular component angular change with postural shift from standing to sitting position. Journal of Bone and Joint Surgery, 96(12), 978–986. https://doi.org/10.2106/jbjs.m.00765
Rivière, C., Lazennec, J. Y., Van Der Straeten, C., Auvinet, E., Cobb, J., & Muirhead-Allwood, S. (2017). The influence of spine-hip relations on total hip replacement: A systematic review. Orthopaedics and Traumatology, 103(4), 559–568. https://doi.org/10.1016/j.otsr.2017.02.014
Mavčič, B., & Antolič, V. (2021). Cementless femoral stem fixation and leg-length discrepancy after total hip arthroplasty in different proximal femoral morphological types. International Orthopaedics, 45(4), 891–896. https://doi.org/10.1007/s00264-020-04671-1
Verma, M., Joshi, S., Tuli, A., Raheja, S., Jain, P., & Srivastava, P. (2017). Morphometry of proximal femur in Indian population. Journal of Clinical and Diagnostic Research, 11(2), Ac01–Ac04. https://doi.org/10.7860/jcdr/2017/23955.9210
Lazennec, J. Y., Brusson, A., & Rousseau, M. A. (2013). Lumbar-pelvic-femoral balance on sitting and standing lateral radiographs. Orthopaedics and Traumatology, 99(1), S87–S103. https://doi.org/10.1016/j.otsr.2012.12.003
Gorin, M., Roger, B., Lazennec, J. Y., Charlot, N., Arafati, N., Bissery, A., et al. (2004). Hip-spine relationship: A radio-anatomical study for optimization in acetabular cup positioning. Surgical and Radiologic Anatomy, 26(2), 136–144. https://doi.org/10.1007/s00276-003-0195-x
Archbold, H. A. P., Mockford, B., Molloy, D., McConway, J., Ogonda, L., & Beverland, D. (2006). The transverse acetabular ligament: an aid to orientation of the acetabular component during primary total hip replacement. The Journal of Bone and Joint Surgery, 88-B(7), 883–886. https://doi.org/10.1302/0301-620x.88b7.17577
Nawabi, D. H., Meftah, M., Nam, D., Ranawat, A. S., & Ranawat, C. S. (2014). Durable fixation achieved with medialized, high hip center cementless THAs for Crowe II and III dysplasia. Clinical Orthopaedics and Related Research, 472(2), 630–636. https://doi.org/10.1007/s11999-013-3187-0
Russotti, G. M., & Harris, W. H. (1991). Proximal placement of the acetabular component in total hip arthroplasty. A long-term follow-up study. The Journal of Bone and Joint Surgery, 73(4), 587–592. https://doi.org/10.2106/00004623-199173040-00016
Shen, J., Sun, J., Ma, H., Du, Y., Li, T., & Zhou, Y. (2020). High Hip Center technique in total hip arthroplasty for crowe type II-III developmental dysplasia: Results of midterm follow-up. Orthopaedic Surgery, 12(4), 1245–1252. https://doi.org/10.1111/os.12756
Bhaskar, D., Rajpura, A., & Board, T. (2017). Current concepts in acetabular positioning in total hip arthroplasty. Indian Journal of Orthopaedics, 51(4), 386–396. https://doi.org/10.4103/ortho.IJOrtho_144_17
Eggli, S., Pisan, M., & Müller, M. E. (1998). The value of preoperative planning for total hip arthroplasty. The Journal of Bone and Joint Surgery, 80(3), 382–390. https://doi.org/10.1302/0301-620x.80b3.7764
Nercessian, O. A., Piccoluga, F., & Eftekhar, N. S. (1994). Postoperative sciatic and femoral nerve palsy with reference to leg lengthening and medializatiod lateralization of the hip joint following total hip arthroplasty. Clinical Orthopaedics and Related Research. https://doi.org/10.1097/00003086-199407000-00025
Konyves, A. (2005). The importance of leg length discrepancy after total hip arthroplasty. Journal of Bone and Joint Surgery, 87-B(2), 155–157. https://doi.org/10.1302/0301-620x.87b2.14878
Williamson, J. A., & Reckling, F. W. (1978). Limb length discrepancy and related problems following total hip joint replacement. Clinical Orthopaedics and Related Research. https://doi.org/10.1097/00003086-197807000-00016
Sarangi, P. P., & Bannister, G. C. (1997). Leg length discrepancy after total hip replacement. HIP International, 7(3), 121–124. https://doi.org/10.1177/112070009700700306
Cummings, G., Scholz, J. P., & Barnes, K. (1993). The effect of imposed leg length difference on pelvic bone symmetry. Spine, 18(3), 368–373. https://doi.org/10.1097/00007632-199303000-00012
Mihalko, W. M., Phillips, M. J., & Krackow, K. A. (2001). Acute sciatic and femoral neuritis following total hip arthroplasty. The Journal of Bone and Joint Surgery-American Volume, 83(4), 589–592. https://doi.org/10.2106/00004623-200104000-00017
Konyves, A., & Bannister, G. C. (2005). The importance of leg length discrepancy after total hip arthroplasty. The Journal of Bone and Joint Surgery British Volume, 87-B(2), 155–157. https://doi.org/10.1302/0301-620x.87b2.14878
Masaki, T., Takashi, N., Takashi, S., & Nobuhiko, S. (2012). Reliability of intra-operative assessment of soft tissue tension in total hip arthroplasty. Orthopaedic Proceedings, 94(SUPP_XL), 186. https://doi.org/10.1302/1358-992x.94bsupp_xl.ista2011-186
Hermansen, L. L., Viberg, B., Hansen, L., & Overgaard, S. (2021). “True” cumulative incidence of and risk factors for hip dislocation within 2 years after primary total hip arthroplasty due to osteoarthritis: a nationwide population-based study from the danish hip arthroplasty register. Journal of Bone and Joint Surgery, 103(4), 295–302. https://doi.org/10.2106/jbjs.19.01352
Fukunishi, S., Fukui, T., Nishio, S., Fujihara, Y., Okahisa, S., & Yoshiya, S. (2012). Combined anteversion of the total hip arthroplasty implanted with image-free cup navigation and without stem navigation. Orthopedic Reviews (Pavia), 4(4), e33. https://doi.org/10.4081/or.2012.e33
Acknowledgements
(1) Clinical fellows who assisted in data recovery: Dr. Karthik J, Dr. Ketan J Khatri, Dr. Sai Suchitra G, Dr. Kiran Manohar. (2) Mr. Ramalingam Rajendran: image formatting and database archive management. (3) Mr. Mohan Kumar: database entry and Patient Coordination
Funding
No specific financial support was received for this study.
Author information
Authors and Affiliations
Contributions
VCB: manuscript writing and chief operating surgeon. SP: manuscript edit and chief operating surgeon. AK: data collection and operating surgeon. KK: manuscript writing and operating surgeon. SY: data collection, analysis, and manuscript writing. SP: statistics workup, manuscript writing, and edit.
Corresponding authors
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Standard Statement
This article does not contain any studies with human or animal subjects performed by the any of the authors.
Ethical Approval
This manuscript has been read and approved by all the authors and presents trustworthy and reliable scientific data obtained in our facilities.
Consent for Study
The study was approved by SIMS Institutional Review Board and informed consent from patients was obtained.
Informed Consent
For this type of study informed consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Bose, V.C., Pichai, S., Ashok Kumar, P.S. et al. Does Balancing a Total Hip Arthroplasty Require a New Paradigm? Functional 3-Dimensional Balancing in Total Hip Arthroplasty. JOIO 55, 1240–1249 (2021). https://doi.org/10.1007/s43465-021-00505-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43465-021-00505-3