Abstract
Purpose
With advancements to blood management strategies, risk of perioperative transfusion following surgical treatment of adolescent idiopathic scoliosis (AIS) has diminished. We hypothesize that routine laboratory testing on postoperative-day 1 (POD1) and beyond is unnecessary. The purpose of this study is to determine necessity of POD1 labs, particularly hematocrit and hemoglobin levels, following surgical management of AIS.
Methods
We performed a retrospective cohort study of consecutive AIS patients aged 11–19 who underwent posterior spinal fusion (PSF) at a single institution. Univariable logistic regression was utilized to determine factors associated with hematocrit ≤ 22% on POD1 or a postoperative transfusion. Firth’s penalized logistic regression was used for any separation in data. Youden’s index was utilized to determine the optimal point on the ROC curve that maximizes both sensitivity and specificity.
Results
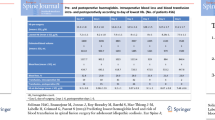
527 patients qualified for this study. Among the eight total patients with POD1 hematocrit ≤ 22, none underwent transfusion. These patients had lower last intraoperative hematocrit levels compared to patients with POD1 hematocrit > 22% (24.1% vs 31.5%, p < 0.001), and these groups showed no difference in preoperative hematocrit levels (38.2% vs 39.8%, p = 0.11). Four patients underwent postoperative transfusion. Both preoperative hematocrit levels (34.0% vs 39.9%, p = 0.001) and last intraoperative hematocrit levels (25.1% vs 31.4%, p = 0.002) were lower compared to patients without transfusion. Intraoperative hematocrit < 26.2%, operative time of more than 35.8 min per level fused, or cell salvage > 241 cc were significant risk factors for postoperative transfusion.
Conclusion
Transfusion after PSF for AIS is exceedingly rare. POD1 labs should be considered when last intraoperative hematocrit < 26%, operative time per level fused > 35 min, or cell salvage amount > 241 cc. Otherwise, unless symptomatic, patients do not benefit from postoperative laboratory screening.
Similar content being viewed by others
Data availability
The data supporting the findings of this research are available upon request from the corresponding author.
References
Weiss H, Moramarco M (2013) Scoliosis-treatment indications according to current evidence. OA Musculoskelet Med 3:1–7
Maruyama T, Takeshita K (2008) Surgical treatment of scoliosis: a review of techniques currently applied. Scoliosis 3:1–6. https://doi.org/10.1186/1748-7161-3-6/FIGURES/8
Edler A, Murray DJ, Forbes RB (2003) Blood loss during posterior spinal fusion surgery in patients with neuromuscular disease: is there an increased risk? Paediatr Anaesth 13:818–822. https://doi.org/10.1046/J.1460-9592.2003.01171.X
Shapiro F, Sethna N (2004) Blood loss in pediatric spine surgery. Eur Spine J 13(Suppl 1):S6–S17. https://doi.org/10.1007/S00586-004-0760-Y
Guigui P, Blamoutier A (2005) Complications of surgical treatment of spinal deformities: a prospective multicentric study of 3311 patients. Rev Chir Orthop Reparatrice Appar Mot 91:314–327. https://doi.org/10.1016/S0035-1040(05)84329-6
Xu S, Meng FQ, Guo C, Liang Y, Zhu ZQ, Liu HY (2021) Modified hidden blood loss based on drainage in posterior surgery on lumbar stenosis syndrome with rheumatoid arthritis. Orthop Surg 13:2263–2270. https://doi.org/10.1111/OS.13157
Smorgick Y, Baker KC, Bachison CC, Herkowitz HN, Montgomery DM, Fischgrund JS (2013) Hidden blood loss during posterior spine fusion surgery. Spine J 13:877–881. https://doi.org/10.1016/J.SPINEE.2013.02.008
Ido K, Neo M, Asada Y, Kondo K, Morita T, Sakamoto T, Hayashi R, Kuriyama S (2000) Reduction of blood loss using tranexamic acid in total knee and hip arthroplasties. Arch Orthop Trauma Surg 120:518–520. https://doi.org/10.1007/S004029900132
Cheriyan T, Maier SP, Bianco K, Slobodyanyuk K, Rattenni RN, Lafage V, Schwab FJ, Lonner BS, Errico TJ (2015) Efficacy of tranexamic acid on surgical bleeding in spine surgery: a meta-analysis. Spine J 15:752–761. https://doi.org/10.1016/J.SPINEE.2015.01.013
Jones KE, Butler EK, Barrack T, Ledonio CT, Forte ML, Cohn CS, Polly DW (2017) Tranexamic acid reduced the percent of total blood volume lost during adolescent idiopathic scoliosis surgery. Int J Spine Surg 11:212–217. https://doi.org/10.14444/4027
Sui WY, Ye F, Yang JL (2016) Efficacy of tranexamic acid in reducing allogeneic blood products in adolescent idiopathic scoliosis surgery. BMC Musculoskelet Disord. https://doi.org/10.1186/S12891-016-1006-Y
Goobie SM, Zurakowski D, Glotzbecker MP, McCann ME, Hedequist D, Brustowicz RM, Sethna NF, Karlin LI, Emans JB, Timothy Hresko M (2018) Tranexamic acid is efficacious at decreasing the rate of blood loss in adolescent scoliosis surgery: a randomized placebo-controlled trial. J Bone Joint Surg Am 100:2024–2032. https://doi.org/10.2106/JBJS.18.00314
Verma K, Errico T, Diefenbach C, Hoelscher C, Peters A, Dryer J, Huncke T, Boenigk K, Lonner BS (2014) The relative efficacy of antifibrinolytics in adolescent idiopathic scoliosis: a prospective randomized trial. J Bone Joint Surg Am 96:e80(1). https://doi.org/10.2106/JBJS.L.00008
Liu JM, Fu BQ, Chen WZ, Chen JW, Huang SH, Liu ZL (2017) Cell salvage used in scoliosis surgery: is it really effective? World Neurosurg 101:568–576. https://doi.org/10.1016/J.WNEU.2017.02.057
Cheriyan J, Cheriyan T, Dua A, Goldstein JA, Errico TJ, Kumar V (2020) Efficacy of intraoperative cell salvage in spine surgery: a meta-analysis. J Neurosurg Spine 33:261–269. https://doi.org/10.3171/2019.12.SPINE19920
Carless PA, Henry DA, Moxey AJ, O’Connell D, Brown T, Fergusson DA (2010) Cell salvage for minimising perioperative allogeneic blood transfusion. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD001888.PUB4
Borden TC, Bellaire LL, Fletcher ND (2016) Improving perioperative care for adolescent idiopathic scoliosis patients: the impact of a multidisciplinary care approach. J Multidiscip Healthc 9:435–446. https://doi.org/10.2147/JMDH.S95319
Barnes MS, Igou TA, Costner CF, Bork MA, Martin V, Aydinian TN, Dunn T (2021) Routine postoperative laboratory testing: necessity or habit? J Gynecol Surg 37:399–401. https://doi.org/10.1089/GYN.2020.0181
Matthyssens LE, Ziol M, Barrat C, Champault GG (2006) Routine surgical pathology in general surgery. Br J Surg 93:362–368. https://doi.org/10.1002/bjs.5268
Netser JC, Robinson RA, Smith RJ, Raab SS (1997) Value-based pathology: a cost–benefit analysis of the examination of routine and nonroutine tonsil and adenoid specimens. Am J Clin Pathol 108:158–165. https://doi.org/10.1093/AJCP/108.2.158
Dewan M, Galvez J, Polsky T, Kreher G, Kraus B, Ahumada L, Mccloskey J, Wolfe H (2017) Reducing unnecessary postoperative complete blood count testing in the pediatric intensive care unit. Perm J 21:16–051. https://doi.org/10.7812/TPP/16-051
Halawi MJ, Plourde JM, Cote MP (2019) Routine postoperative laboratory tests are not necessary after primary total hip arthroplasty. J Arthroplasty 34:538–541. https://doi.org/10.1016/J.ARTH.2018.11.037
Paynter JW, Raley JA, Kyrkos JG, Paré DW, Houston H, Crosby LA, Parada SA (2020) Routine postoperative laboratory tests are unnecessary after primary reverse shoulder arthroplasty. J Shoulder Elbow Surg 29:1656–1664. https://doi.org/10.1016/J.JSE.2019.12.023
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG (2009) Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inf 42:377–381. https://doi.org/10.1016/J.JBI.2008.08.010
Guo SS, Wu W, Chumlea WC, Roche AF (2002) Predicting overweight and obesity in adulthood from body mass index values in childhood and adolescence. Am J Clin Nutr 76:653–658. https://doi.org/10.1093/AJCN/76.3.653
Bowen RE, Gardner S, Scaduto AA, Eagan M, Beckstead J (2010) Efficacy of intraoperative cell salvage systems in pediatric idiopathic scoliosis patients undergoing posterior spinal fusion with segmental spinal instrumentation. Spine (Phila Pa 1976) 35:246–251. https://doi.org/10.1097/BRS.0B013E3181BDF22A
Ersen O, Ekıncı S, Bılgıc S, Kose O, Oguz E, Sehırlıoglu A (2012) Posterior spinal fusion in adolescent idiopathic scoliosis with or without intraoperative cell salvage system: a retrospective comparison. Musculoskelet Surg 96:107–110. https://doi.org/10.1007/S12306-012-0203-6/METRICS
Weiss JM, Skaggs D, Tanner J, Tolo V (2007) Cell saver: is it beneficial in scoliosis surgery? J Child Orthop 1:221. https://doi.org/10.1007/S11832-007-0032-6
Siller TA, Dickson JH, Erwin WD (1996) Efficacy and cost considerations of intraoperative autologous transfusion in spinal fusion for idiopathic scoliosis with predeposited blood. Spine (Phila Pa 1976) 21:848–852. https://doi.org/10.1097/00007632-199604010-00015
Miao YL, Ma HS, Guo WZ, Wu JG, Liu Y, Shi WZ, Wang XP, Mi WD, Fang WW (2014) The efficacy and cost-effectiveness of cell saver use in instrumented posterior correction and fusion surgery for scoliosis in school-aged children and adolescents. PLoS ONE 9:e92997. https://doi.org/10.1371/JOURNAL.PONE.0092997
Owens RK, Crawford CH, Djurasovic M, Canan CE, Burke LO, Bratcher KR, McCarthy KJ, Carreon LY (2013) Predictive factors for the use of autologous cell saver transfusion in lumbar spinal surgery. Spine (Phila Pa 1976) 38:E217–E222. https://doi.org/10.1097/BRS.0B013E31827F044E
Elgafy H, Bransford RJ, McGuire RA, Dettori JR, Fischer D (2010) Blood loss in major spine surgery: are there effective measures to decrease massive hemorrhage in major spine fusion surgery? Spine (Phila Pa 1976) 35:S47–S56. https://doi.org/10.1097/BRS.0B013E3181D833F6
Ng BKW, Chau WW, Hung ALH, Hui ACN, Lam TP, Cheng JCY (2015) Use of tranexamic acid (TXA) on reducing blood loss during scoliosis surgery in Chinese adolescents. Scoliosis 10:1–6. https://doi.org/10.1186/S13013-015-0052-9/TABLES/3
Neilipovitz DT, Murto K, Hall L, Barrowman NJ, Splinter WM (2001) A randomized trial of tranexamic acid to reduce blood transfusion for scoliosis surgery. Anesth Analg 93:82–87. https://doi.org/10.1097/00000539-200107000-00018
Lykissas MG, Crawford AH, Chan G, Aronson LA, Al-Sayyad MJ (2013) The effect of tranexamic acid in blood loss and transfusion volume in adolescent idiopathic scoliosis surgery: a single-surgeon experience. J Child Orthop 7:245–249. https://doi.org/10.1007/S11832-013-0486-7
Halanski MA, Cassidy JA, Hetzel S, Reischmann D, Hassan N (2014) The efficacy of amicar versus tranexamic acid in pediatric spinal deformity surgery: a prospective, randomized, double-blinded pilot study. Spine Deform 2:191–197. https://doi.org/10.1016/J.JSPD.2014.02.001
Yvonne Buowari O (2013) Complications of venepuncture. Adv Biosci Biotechnol 4:126–128. https://doi.org/10.4236/abb.2013.41A018
Pate JT, Blount RL, Cohen LL, Smith AJ (2010) Childhood medical experience and temperament as predictors of adult functioning in medical situations. Child Health Care 25:281–298. https://doi.org/10.1207/S15326888CHC2504_4
Eaton KP, Levy K, Soong C, Pahwa AK, Petrilli C, Ziemba JB, Cho HJ, Alban R, Blanck JF, Parsons AS (2017) Evidence-based guidelines to eliminate repetitive laboratory testing. JAMA Intern Med 177:1833–1839. https://doi.org/10.1001/JAMAINTERNMED.2017.5152
Yoshihara H, Yoneoka D (2014) Predictors of allogeneic blood transfusion in spinal fusion for pediatric patients with idiopathic scoliosis in the United States, 2004–2009. Spine (Phila Pa 1976) 39:1860–1867. https://doi.org/10.1097/BRS.0000000000000530
Thompson ME, Kohring JM, McFann K, McNair B, Hansen JK, Miller NH (2014) Predicting excessive hemorrhage in adolescent idiopathic scoliosis patients undergoing posterior spinal instrumentation and fusion. Spine J 14:1392–1398. https://doi.org/10.1016/J.SPINEE.2013.08.022
Yilmaz G, Borkhuu B, Dhawale AA, Oto M, Littleton AG, Mason DE, Gabos PG, Shah SA (2012) Comparative analysis of hook, hybrid, and pedicle screw instrumentation in the posterior treatment of adolescent idiopathic scoliosis. J Pediatr Orthop 32:490–499. https://doi.org/10.1097/BPO.0B013E318250C629
Kim HJ, Park HS, Jang MJ, Koh WU, Song JG, Lee CS, Yang HS, Ro YJ (2018) Predicting massive transfusion in adolescent idiopathic scoliosis patients undergoing corrective surgery: association of preoperative radiographic findings. Medicine. https://doi.org/10.1097/MD.0000000000010972
Hassan N, Halanski M, Wincek J, Reischman D, Sanfilippo D, Rajasekaran S, Wells C, Tabert D, Kurt B, Mitchell D, Huntington J, Cassidy J (2011) Blood management in pediatric spinal deformity surgery: review of a 2-year experience. Transfusion (Paris) 51:2133–2141. https://doi.org/10.1111/J.1537-2995.2011.03175.X
Li C, Yang M, Wang C, Wang C, Fan J, Chen Z, Wei X, Zhang G, Bai Y, Zhu X, Xie Y, Li M (2015) Preoperative factors predicting intraoperative blood loss in female patients with adolescent idiopathic scoliosis. Medicine 94:e359. https://doi.org/10.1097/MD.0000000000000359
Soini V, Syvänen J, Helenius I, Helenius L, Raitio A (2023) Perioperative risk factors for bleeding in adolescents undergoing pedicle screw instrumentation for scoliosis. Children. https://doi.org/10.3390/CHILDREN10020381
Funding
Funding was not obtained for this study.
Author information
Authors and Affiliations
Contributions
DL: visualization, supervision. AF: conceptualization, methodology, data collection, data analysis, visualization, supervision. GL: conceptualization, methodology, data analysis, visualization, writing: original draft preparation, supervision. DC: conceptualization, methodology, data collection, writing: reviewing and editing, supervision. CB: conceptualization, methodology, data collection, data analysis, visualization, writing: original draft preparation, supervision. TH: conceptualization, methodology, data collection, data analysis, visualization, writing: original draft preparation, supervision. DH: conceptualization, methodology, data collection, data analysis, visualization, writing: original draft preparation, supervision. GH: data collection, visualization, writing: original draft preparation.
Corresponding author
Ethics declarations
Conflict of interest
DL, AF, GL, DC, CB, and TH have no conflicts of interest to declare. DH: educational consultant and member of advisory board, Medtronic. GH: educational consultant and member of advisory board, Medtronic; founding partner, Tether Implant Corporation.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Liu, D.S., Farid, A.R., Linden, G.S. et al. Utility of postoperative laboratory testing after posterior spinal fusion for adolescent idiopathic scoliosis. Spine Deform 12, 375–381 (2024). https://doi.org/10.1007/s43390-023-00771-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43390-023-00771-1