Abstract
Purpose
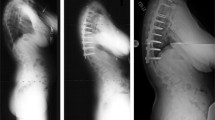
To assess if the preservation of preoperative kyphosis within the cephalad two motion segments of instrumented posterior spinal fusions (PSF), for idiopathic scoliosis (IS), would be associated with lower frequency of proximal junctional kyphosis (PJK) at 2 years postoperatively. Previous studies on PJK in IS have reported conflicting findings; none has evaluated the relationship between segmental kyphosis within the cephalad instrumented construct and PJK.
Methods
One hundred consecutive patients undergoing PSF for IS by a single surgeon with minimum 2-year follow-up were evaluated. Radiographic evaluation focused on sagittal alignment of the upper instrumented vertebrae (UIV), the 1 and 2 vertebrae cephalad (UIV + 1, UIV + 2) and caudal (UIV − 1, UIV − 2). This was measured between the inferior endplate of the UIV and the superior endplate of the UIV + 1 and UIV + 2 or between the superior endplate of the UIV and the inferior endplate of the UIV − 1 and UIV − 2. PJK was defined as present if the final UIV + 2 ≥ 10° and final UIV + 2—preop UIV + 2 ≥ 10°.
Results
There were 78 females and 22 males whose mean age was 14.6 (± 2.1) years at surgery; mean follow-up was 3.9 (2–9.3) years. The overall frequency of PJK was 25% (25/100) at final follow-up. Preoperative mean coronal curve measured 63° (40°–107°) with a mean 66% correction at final follow-up. UIV was T2 (n = 15), T3 (n = 47) or T4 (n = 38). More caudal UIVs were associated with PJK development (p = 0.04): T2 (13%), T3 (21%) and T4 (34%). Greater preoperative T5–T12 thoracic kyphosis and UIV − 2, and lower major curve apex (below T12) were more likely to develop PJK (p = 0.019, p = 0.004 and p = 0.007, respectively). Post-operatively, larger values for UIV − 1 (p ≤ 0.001) and UIV − 2 (p = 0.002) were associated with PJK at final follow-up. Longer fusion lengths (10–13 vs. 6–9 segments, p = 0.02) and the presence of thoracolumbar/lumbar structural curves (Lenke 3–6 vs. 1–2, p = 0.032) had higher rates of PJK (32% vs 10% and 37% vs 18%, respectively). Changes in UIV − 1 and UIV − 2 (preoperatively to immediately post-op) did not influence the development of PJK. At final follow-up, no patient required revision surgery for symptomatic proximal junctional kyphosis.
Conclusions
In this study, changes in UIV − 1 and UIV − 2 at surgery were not related to PJK. Greater preoperative T5–T12 thoracic kyphosis and UIV − 2, lower major curve apex (T12 and below), and greater post-operative UIV − 1 and UIV − 2 were associated with higher frequencies of PJK. Higher UIV (T2 vs. T4) and LIV levels had a protective effect against PJK. Based on this study, the preservation of segmental kyphosis within the instrumented cephalad two levels of the PSF did not minimize the occurrence of radiographic PJK.
Level of evidence
Level IV.

Similar content being viewed by others
References
Lee GA, Betz RR, Clements DH 3rd, Huss GK (1999) Proximal kyphosis after posterior spinal fusion in patients with idiopathic scoliosis. Spine (Phila Pa 1976) 24:795–799
Hollenbeck SM, Glattes RC, Asher MA, Lai SM, Burton DC (2008) The prevalence of increased proximal junctional flexion following posterior instrumentation and arthrodesis for adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 33:1675–1681
Rhee JM, Bridwell KH, Won DS et al (2002) Sagittal plane analysis of adolescent idiopathic scoliosis: the effect of anterior versus posterior instrumentation. Spine (Phila Pa 1976) 27:2350–2356
Kim YJ, Bridwell KH, Lenke LG, Kim J, Cho SK (2005) Proximal junctional kyphosis in adolescent idiopathic scoliosis following segmental posterior spinal instrumentation and fusion: minimum 5-year follow-up. Spine (Phila Pa 1976) 30:2045–2050
Kim YJ, Lenke LG, Bridwell KH et al (2007) Proximal junctional kyphosis in adolescent idiopathic scoliosis after 3 different types of posterior segmental spinal instrumentation and fusions: incidence and risk factor analysis of 410 cases. Spine (Phila Pa 1976) 32:2731–2738
Anderson AL, McIff TE, Asher MA, Burton DC, Glattes RC (2009) The effect of posterior thoracic spine anatomical structures on motion segment flexion stiffness. Spine (Phila Pa 1976) 34:441–446
Sponseller PD, Betz R, Newton PO et al (2009) Differences in curve behavior after fusion in adolescent idiopathic scoliosis patients with open triradiate cartilages. Spine (Phila Pa 1976) 34:827–831
Glattes RC, Bridwell KH, Lenke LG et al (2005) Proximal junctional kyphosis in adult spinal deformity following long instrumented posterior spinal fusion: incidence, outcomes, and risk factor analysis. Spine (Phila Pa 1976) 30:1643–1649
Hilibrand AS, Tannenbaum DA, Graziano GP, Loder RT, Hensinger RN (1995) The sagittal alignment of the cervical spine in adolescent idiopathic scoliosis. J Pediatr Orthop 15:627–632
Al Khudairy A, Gauthier L, Heflin JA et al (2014) Reliability of proximal junctional kyphosis measurements for young children with scoliosis. Spine Deform 2:448–453
Rastegar F, Contag A, Daniels A et al (2018) Proximal junctional kyphosis: inter- and intraobserver reliability of radiographic measurements in adult spinal deformity. Spine (Phila Pa 1976) 43:E40–E44
Sacramento-Dominguez C, Vayas-Diez R, Coll-Mesa L et al (2009) Reproducibility measuring the angle of proximal junctional kyphosis using the first or the second vertebra above the upper instrumented vertebrae in patients surgically treated for scoliosis. Spine (Phila Pa 1976) 34:2787–2791
Lenke LG, Betz RR, Harms J et al (2001) Adolescent idiopathic scoliosis: a new classification to determine extent of spinal arthrodesis. J Bone Jt Surg Am 83:1169–1181
Lonner BS, Newton P, Betz R et al (2007) Operative management of Scheuermann’s kyphosis in 78 patients: radiographic outcomes, complications, and technique. Spine (Phila Pa 1976) 32:2644–2652
Denis F, Sun EC, Winter RB (2009) Incidence and risk factors for proximal and distal junctional kyphosis following surgical treatment for Scheuermann kyphosis: minimum five-year follow-up. Spine (Phila Pa 1976) 34:E729–E734
Funding
No funding was received for this work.
Author information
Authors and Affiliations
Contributions
SJL: Substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work. Drafting the work or revising it critically for important intellectual content. Final approval of the version to be published. Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. JR: Substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work. Drafting the work or revising it critically for important intellectual content, Final approval of the version to be published. Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. DF: Substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work. Drafting the work or revising it critically for important intellectual content. Final approval of the version to be published. Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. SM: Substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work. Drafting the work or revising it critically for important intellectual content. Final approval of the version to be published. Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Conflict of interest
No conflicts exist for any of the authors pertaining to the submitted work.
Ethical approval
No human subjects or animals participated; therefore, no informed consent was obtained. IRB approval was obtained from Washington University Institutional Review Board.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Luhmann, S.J., Roth, J., DeFreitas, D. et al. The impact of segmental spinal alignment on the development of proximal junctional kyphosis after instrumented posterior spinal fusions for idiopathic scoliosis. Spine Deform 10, 369–375 (2022). https://doi.org/10.1007/s43390-021-00407-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43390-021-00407-2