Abstract
Background
Unplanned readmissions and reoperations are known to be associated with undesirable costs and potentially inferior outcomes in complex adult spinal deformity (ASD) surgery. A paucity of literature exists on the impact of readmissions/reoperations on patient-reported outcomes (PRO) in this population.
Methods
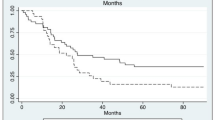
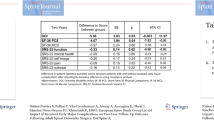
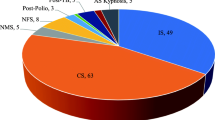
Consecutively treated adult patients who underwent complex ASD surgery at a single institution from 2015–2018 and minimum 2-year follow-up were studied. Demographics/comorbidities, operative factors, inpatient complications, and postoperative clinical and patient-reported outcomes (SRS-22r, ODI) were assessed for those with and without readmission/reoperation.
Results
175 patients (72% female, mean age 52.6 ± 16.4) were included. Mean total instrumented/fused levels was 13.3 ± 4.1, range 6–25. The readmission and reoperation rates were 16.6% and 12%, respectively. The two most common causes of reoperation were pseudarthrosis (5.1%) and PJK (4.0%). Predictors for readmission within 2 years following surgery included pulmonary, cardiac, depression and gastrointestinal comorbidities, along with performance of a VCR, and TLIF. At 2 years postoperatively, those who required a readmission/reoperation had significant increases in SRS and reductions in ODI compared to 1-year and preoperative values. Inpatient complications did not negatively impact 2-year PRO’s. The 2-year MCID in PROs was not significantly different between those with and without readmission/reoperation.
Conclusion
Complex ASD surgery carries risk, but the vast majority can achieve MCID (SRS-86.4%, ODI-68.2%) in PROs by 2 years. Importantly, even those with inpatient complications and those who required unplanned readmission/reoperation can improve PROs by 2-year follow-up compared to preoperative baseline and 1-year follow-up and achieve similar improvements compared to those who did not require a readmission.
Level of evidence
III.




Similar content being viewed by others
References
Zanirato A, Damilano M, Formica M, Piazzolla A, Lovi A, Villafane JH, Berjano P (2018) Complications in adult spine deformity surgery: a systematic review of the recent literature with reporting of aggregated incidences. Eur Spine J 27(9):2272–2284
How NE, Street JT, Dvorak MF, Fisher CG, Kwon BK, Paquette S, Smith JS, Shaffrey CI, Ailon T (2019) Pseudarthrosis in adult and pediatric spinal deformity surgery: a systematic review of the literature and meta-analysis of incidence, characteristics, and risk factors. Neurosurg Rev 42(2):319–336
Hyun SJ, Lee BH, Park JH, Kim KJ, Jahng TA, Kim HJ (2017) Proximal junctional kyphosis and proximal junctional failure following adult spinal deformity surgery. Korean J Spine 14(4):126–132
Sebaaly A, Gehrchen M, Silvestre C, Kharrat K, Bari TJ, Kreichati G, Rizkallah M, Roussouly P (2019) Mechanical complications in adult spinal deformity and the effect of restoring the spinal shapes according to the Roussouly classification: a multicentric study. Eur Spine J 29:904–913
Lee NJ, Shin JI, Kothari P, Kim JS, Leven DM, Steinberger J, Guzman JZ, Skovrlj B, Caridi JM, Cho SK (2017) Incidence, impact, and risk factors for 30-day wound complications following elective adult spinal deformity surgery. Global Spine J 7(5):417–424
Soroceanu A, Burton DC, Oren JH, Smith JS, Hostin R, Shaffrey CI, Akbarnia BA, Ames CP, Errico TJ, Bess S, Gupta MC, Deviren V, Schwab FJ, Lafage V (2016) Medical complications after adult spinal deformity surgery: incidence, risk factors, and clinical impact. Spine (Phila Pa 1976) 41(22):1718–1723
McCarthy IM, Hostin RA, Ames CP, Kim HJ, Smith JS, Boachie-Adjei O, Schwab FJ, Klineberg EO, Shaffrey CI, Gupta MC, Polly DW (2014) Total hospital costs of surgical treatment for adult spinal deformity: an extended follow-up study. Spine J 14(10):2326–2333
Elsamadicy AA, Adogwa O, Vuong VD, Sergesketter A, Reddy G, Cheng J, Bagley CA, Karikari IO (2017) Impact of alcohol use on 30-day complication and readmission rates after elective spinal fusion (>/=2 levels) for adult spine deformity: a single institutional study of 1,010 patients. J Spine Surg 3(3):403–410
Elsamadicy AA, Camara-Quintana J, Kundishora AJ, Lee M, Freedman IG, Long A, Qureshi T, Laurans M, Tomak P, Karikari IO (2019) Reduced impact of obesity on short-term surgical outcomes, patient-reported pain scores, and 30-day readmission rates after complex spinal fusion (>/=7 levels) for adult deformity correction. World Neurosurg 127:e108–e113
De la Garza Ramos R, Nakhla J, Echt M, Gelfand Y, Scoco AN, Kinon MD, Yassari R (2018) Risk factors for 30-day readmissions and reoperations after 3-column osteotomy for spinal deformity. Global Spine J 8(5):483–489
Phan K, Kim JS, Capua JD, Lee NJ, Kothari P, Dowdell J, Overley SC, Guzman JZ, Cho SK (2017) Impact of operation time on 30-day complications after adult spinal deformity surgery. Global Spine J 7(7):664–671
Manoharan SR, Baker DK, Pasara SM, Ponce B, Deinlein D, Theiss SM (2016) Thirty-day readmissions following adult spinal deformity surgery: an analysis of the National Surgical Quality Improvement Program (NSQIP) database. Spine J 16(7):862–866
Algattas H, Cohen J, Agarwal N, Hamilton DK (2017) Trends in the use of patient-reported outcome instruments in neurosurgical adult thoracolumbar deformity and degenerative disease literature. J Craniovertebr Junction Spine 8(2):103–107
Pellise F, Vila-Casademunt A, Ferrer M, Domingo-Sabat M, Bago J, Perez-Grueso FJ, Alanay A, Mannion AF, Acaroglu E (2015) Impact on health related quality of life of adult spinal deformity (ASD) compared with other chronic conditions. Eur Spine J 24(1):3–11
Bridwell KH, Baldus C, Berven S, Edwards C 2nd, Glassman S, Hamill C, Horton W, Lenke LG, Ondra S, Schwab F, Shaffrey C, Wootten D (2010) Changes in radiographic and clinical outcomes with primary treatment adult spinal deformity surgeries from two years to three- to five-years follow-up. Spine (Phila Pa 1976) 35(20):1849–1854
Bridwell KH, Glassman S, Horton W, Shaffrey C, Schwab F, Zebala LP, Lenke LG, Hilton JF, Shainline M, Baldus C, Wootten D (2009) Does treatment (nonoperative and operative) improve the two-year quality of life in patients with adult symptomatic lumbar scoliosis: a prospective multicenter evidence-based medicine study. Spine (Phila Pa 1976) 34(20):2171–2178
Liu S, Schwab F, Smith JS, Klineberg E, Ames CP, Mundis G, Hostin R, Kebaish K, Deviren V, Gupta M, Boachie-Adjei O, Hart RA, Bess S, Lafage V (2014) Likelihood of reaching minimal clinically important difference in adult spinal deformity: a comparison of operative and nonoperative treatment. Ochsner J 14(1):67–77
Smith JS, Lafage V, Shaffrey CI, Schwab F, Lafage R, Hostin R, O’Brien M, Boachie-Adjei O, Akbarnia BA, Mundis GM, Errico T, Kim HJ, Protopsaltis TS, Hamilton DK, Scheer JK, Sciubba D, Ailon T, Fu KM, Kelly MP, Zebala L, Line B, Klineberg E, Gupta M, Deviren V, Hart R, Burton D, Bess S, Ames CP (2016) Outcomes of operative and nonoperative treatment for adult spinal deformity: a prospective, multicenter, propensity-matched cohort assessment with minimum 2-year follow-up. Neurosurgery 78(6):851–861
Smith JS, Shaffrey CI, Lafage V, Schwab F, Scheer JK, Protopsaltis T, Klineberg E, Gupta M, Hostin R, Fu KM, Mundis GM Jr, Kim HJ, Deviren V, Soroceanu A, Hart RA, Burton DC, Bess S, Ames CP (2015) Comparison of best versus worst clinical outcomes for adult spinal deformity surgery: a retrospective review of a prospectively collected, multicenter database with 2-year follow-up. J Neurosurg Spine 23(3):349–359
Scheer JK, Smith JS, Clark AJ, Lafage V, Kim HJ, Rolston JD, Eastlack R, Hart RA, Protopsaltis TS, Kelly MP, Kebaish K, Gupta M, Klineberg E, Hostin R, Shaffrey CI, Schwab F, Ames CP (2015) Comprehensive study of back and leg pain improvements after adult spinal deformity surgery: analysis of 421 patients with 2-year follow-up and of the impact of the surgery on treatment satisfaction. J Neurosurg Spine 22(5):540–553
Teles AR, Mattei TA, Righesso O, Falavigna A (2017) Effectiveness of operative and nonoperative care for adult spinal deformity: systematic review of the literature. Global Spine J 7(2):170–178
Yanik EL, Kelly MP, Lurie JD, Baldus CR, Shaffrey CI, Schwab FJ, Bess S, Lenke LG, LaBore A, Bridwell KH (2020) Effect modifiers for patient-reported outcomes in operatively and nonoperatively treated patients with adult symptomatic lumbar scoliosis: a combined analysis of randomized and observational cohorts. J Neurosurg Spine 33:1–10
Arima H, Glassman SD, Bridwell K, Yamato Y, Yagi M, Watanabe K, Matsumoto M, Inami S, Taneichi H, Matsuyama Y, Carreon LY (2020) Reaching minimal clinically important difference in adult spinal deformity surgery: a comparison of patients from North America and Japan. J Neurosurg Spine 32:1–6
Repo JP, Ponkilainen VT, Hakkinen AH, Ylinen J, Bergman P, Kyrola K (2019) Assessment of Construct Validity of the Oswestry Disability Index and the Scoliosis Research Society-30 Questionnaire (SRS-30) in Patients With Degenerative Spinal Disease. Spine Deform 7(6):929–936
Baldus C, Bridwell KH, Harrast J, Edwards C 2nd, Glassman S, Horton W, Lenke LG, Lowe T, Mardjetko S, Ondra S, Schwab F, Shaffrey C (2008) Age-gender matched comparison of SRS instrument scores between adult deformity and normal adults: are all SRS domains disease specific? Spine (Phila Pa 1976) 33(20):2214–2218
Norman GR, Sloan JA, Wyrwich KW (2003) Interpretation of changes in health-related quality of life: the remarkable universality of half a standard deviation. Med Care 41(5):582–592
Copay AG, Subach BR, Glassman SD, Polly DW Jr, Schuler TC (2007) Understanding the minimum clinically important difference: a review of concepts and methods. Spine J 7(5):541–546
Smith JS, Klineberg E, Lafage V, Shaffrey CI, Schwab F, Lafage R, Hostin R, Mundis GM Jr, Errico TJ, Kim HJ, Protopsaltis TS, Hamilton DK, Scheer JK, Soroceanu A, Kelly MP, Line B, Gupta M, Deviren V, Hart R, Burton DC, Bess S, Ames CP (2016) Prospective multicenter assessment of perioperative and minimum 2-year postoperative complication rates associated with adult spinal deformity surgery. J Neurosurg Spine 25(1):1–14
Smith JS, Shaffrey CI, Klineberg E, Lafage V, Schwab F, Lafage R, Kim HJ, Hostin R, Mundis GM Jr, Gupta M, Liabaud B, Scheer JK, Diebo BG, Protopsaltis TS, Kelly MP, Deviren V, Hart R, Burton D, Bess S, Ames CP (2017) Complication rates associated with 3-column osteotomy in 82 adult spinal deformity patients: retrospective review of a prospectively collected multicenter consecutive series with 2-year follow-up. J Neurosurg Spine 27(4):444–457
Fakurnejad S, Scheer JK, Lafage V, Smith JS, Deviren V, Hostin R, Mundis GM Jr, Burton DC, Klineberg E, Gupta M, Kebaish K, Shaffrey CI, Bess S, Schwab F, Ames CP (2015) The likelihood of reaching minimum clinically important difference and substantial clinical benefit at 2 years following a 3-column osteotomy: analysis of 140 patients. J Neurosurg Spine 23(3):340–348
Faldini C, Di Martino A, Borghi R, Perna F, Toscano A, Traina F (2015) Long vs. short fusions for adult lumbar degenerative scoliosis: does balance matters? Eur Spine J 24(Suppl 7):887–892
Elsamadicy AA, Adogwa O, Sergesketter A, Vuong VD, Lydon E, Behrens S, Cheng J, Bagley CA, Karikari IO (2017) Reduced impact of smoking status on 30-day complication and readmission rates after elective spinal fusion (>/=3 levels) for adult spine deformity: a single institutional study of 839 patients. World Neurosurg 107:233–238
Elsamadicy AA, Adogwa O, Behrens S, Sergesketter A, Chen A, Mehta AI, Vasquez RA, Cheng J, Bagley CA, Karikari IO (2017) Impact of surgical approach on complication rates after elective spinal fusion (>/=3 levels) for adult spine deformity. J Spine Surg 3(1):31–37
Passias PG, Klineberg EO, Jalai CM, Worley N, Poorman GW, Line B, Oh C, Burton DC, Kim HJ, Sciubba DM, Hamilton DK, Ames CP, Smith JS, Shaffrey CI, Lafage V, Bess S (2016) Hospital readmission within 2 years following adult thoracolumbar spinal deformity surgery: prevalence, predictors, and effect on patient-derived outcome measures. Spine (Phila Pa 1976) 41(17):1355–1364
Riley MS, Bridwell KH, Lenke LG, Dalton J, Kelly MP (2018) Health-related quality of life outcomes in complex adult spinal deformity surgery. J Neurosurg Spine 28(2):194–200
Auerbach JD, Lenke LG, Bridwell KH, Sehn JK, Milby AH, Bumpass D, Crawford CH 3rd, O’Shaughnessy BA, Buchowski JM, Chang MS, Zebala LP, Sides BA (2012) Major complications and comparison between 3-column osteotomy techniques in 105 consecutive spinal deformity procedures. Spine (Phila Pa 1976) 37(14):1198–1210
Glassman SD, Hamill CL, Bridwell KH, Schwab FJ, Dimar JR, Lowe TG (2007) The impact of perioperative complications on clinical outcome in adult deformity surgery. Spine (Phila Pa 1976) 32(24):2764–2770
Funding
There was no financial support for this research project.
Author information
Authors and Affiliations
Contributions
NL and MC: substantial contributions to the conception and design of the work; the acquisition, analysis, and interpretation of data for the work, drafting the work and revising it critically for important intellectual content, final approval of the version to be published, contributed effort to the study; EL and ZS: substantial contributions to the conception and design of the work; the acquisition, analysis, and interpretation of data for the work, revising the work critically for important intellectual content, final approval of the version to be published, contributed effort to the study; RAL and LGL: substantial contributions to the conception and design of the work, revising the work critically for important intellectual content, final approval of the version to be published, contributed cases or effort to the study.
Corresponding author
Ethics declarations
Conflict of interest
LGL reports being a consultant for Medtronic (money donated to charity); receiving royalties from Medtronic and Quality Medical Publishing; receiving reimbursement for airfare and hotels from Broadwater, the Seattle Science Foundation, Stryker Spine, the Spinal Research Foundation, AOSpine, and the Scoliosis Research Society; receiving grant support from the Scoliosis Research Society (money to his institution), EOS Imaging (money to his institution), the Setting Scoliosis Straight Foundation (money to his institution); and receiving grant and fellowship support from AOSpine (money to his institution). Authors RAL/ZMS/EL/NJL/MC report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lee, N.J., Cerpa, M., Leung, E. et al. Do readmissions and reoperations adversely affect patient-reported outcomes following complex adult spinal deformity surgery at a minimum 2 years postoperative?. Spine Deform 9, 789–801 (2021). https://doi.org/10.1007/s43390-020-00235-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43390-020-00235-w