Abstract
Study design
Retrospective case series.
Objectives
To describe how pediatric patients with spinal and pelvic osteomyelitis are diagnosed and treated and assess the diagnostic value of magnetic resonance imaging (MRI), needle aspiration biopsy (NAB), and blood cultures in this population.
Summary of background data
Spinal and pelvic osteomyelitis de novo are uncommon in children and minimal literature exists on the subject. Research has shown that NAB and blood cultures have variable diagnostic yield in adult native osteomyelitis. At our institution, there is no standard protocol for diagnosing and treating pediatric spinal and pelvic osteomyelitis de novo.
Methods
All diagnoses of spinal and pelvic osteomyelitis at a pediatric tertiary care center from 2003 to 2017 were reviewed. Patients aged 0–21 at diagnosis were included. Patients with osteomyelitis resulting from prior spinal operations, wounds, or infections and those with chronic recurrent multifocal osteomyelitis were eliminated. All eligible patients’ diagnoses were confirmed by MRI.
Results
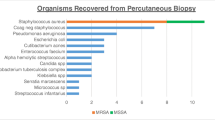
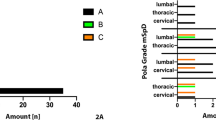
29 patients (18 men, 11 women) met the inclusion criteria. The median age at diagnosis was 11 years old (range 1–18). More than half of all cases (17/29, 59%) affected the lumbar spine. The most common symptoms were back pain (20/29, 69%), fever (18/29, 62%), hip pain (11/29, 38%), and leg pain (8/29, 28%). The majority of NABs and blood cultures performed were negative, but of the positive tests Staphylococcus aureus was the most prevalent bacteria. 86% (25/29) had an MRI before a diagnosis was made and 72% (13/18) had an NAB performed post-diagnosis.
Conclusions
MRI is a popular and helpful tool in diagnosing spinal osteomyelitis de novo. NAB cultures are often negative but can be useful in determining antibiotic treatment.
Level of evidence
Level IV.



Similar content being viewed by others
References
Sapico FL, Montgomerie JZ (1990) Vertebral osteomyelitis. Infect Dis Clin North Am 4(3):539–550
Zimmerli W (2010) Vertebral osteomyelitis. N Engl J Med 362:1022–1029
Grammatico L, Baron S, Rusch E et al (2008) Epidemiology of vertebral osteomyelitis (VO) in France: analysis of hospital-discharge data 2002–2003. Epidemiol Infect 136(5):653–660
McHenry MC, Easley KA, Locker GA (2002) Vertebral osteomyelitis: long-term outcome for 253 patients from 7 cleveland-area hospitals. Clin Infect Dis 34(10):1342–1350
Mylona E, Samarkos M, Kakalou E et al (2009) Pyogenic vertebral osteomyelitis: a systematic review of clinical characteristics. Semin Arthritis Rheum 39(1):10–17
Marco de Lucas E, Mandly AG, Gutiérrez A et al (2009) CT-guided fine-needle aspiration in vertebral osteomyelitis: true usefulness of a common practice. Clin Rheumatol 28(3):315–320
Riise OR, Kirkhus E, Handeland KS et al (2008) Childhood osteomyelitis-incidence and differentiation from other acute onset musculoskeletal features in a population-based study. BMC Pediatr 8:45
Jaramillo D, Treves ST, Kasser JR et al (1995) Osteomyelitis and septic arthritis in children: appropriate use of imaging to guide treatment. AJR Am J Roentgenol 165(2):399–403
Blickman JG, van Die CE, de Rooy JWJ (2004) Current imaging concepts in pediatric osteomyelitis. Eur Radiol 14(4):55–64
Thomson I, Creech CB (2011) Advances in the diagnosis and management of pediatric osteomyelitis. Curr Infect Dis Rep 13(5):451–460
Fernandez M, Carrol CL, Baker CJ (2000) Discitis and vertebral osteomyelitis in children: an 18-year review. Pediatrics 105(6):1299–1304
Davidson D, Letts M, Khoshhal K (2003) Pelvic osteomyelitis in children: a comparison of decades from 1980–1989 with 1990–2001. J Pediatr Orthop 23(4):514–521
Thomsen I, Creech CB (2011) Advances in the diagnosis and management of pediatric osteomyelitis. Curr Infect Dis Rep 13:451–460
Palestro CJ, Love C, Miller TT (2006) Infection and musculoskeletal conditions: imaging of musculoskeletal infections. Best Pract Res Clin Rehumatol 20(6):1197–1218
Chew FS, Kline MJ (2001) Diagnostic yield of CT-guided percutaneous aspiration procedures in suspected spontaneous infectious diskitis. Radiology 218(1):211–214
Jensen AG, Espersen F, Skinhoj P et al (1998) Bacteremic Staphylococcus aureus spondylitis. Arch Intern Med 158(5):509–517
Marschall J, Bhavan KP, Olsen MA et al (2011) The impact of prebiopsy antibiotics on pathogen recovery in hematogenous vertebral osteomyelitis. Clin Infect Dis 52(7):867–872
Peltola H, Pääkkönen M (2014) Acute osteomyelitis in children. N Engl J Med 370(4):352–360
Bolivar R, Kohl S, Pickering LK (1978) Vertebral osteomyelitis in children: report of four cases. Pediatrics 62(4):549–553
Mete B, Kurt C, Yilmaz MH et al (2012) Vertebral osteomyelitis: 8 years’ experience of 100 cases. Rheumatol Int 32(11):3591–3597
Priest DH, Peacock JE (2005) Hematogenous vertebral osteomyelitis due to Staphylococcus aureus in the adult: clinical features and therapeutic outcomes. South Med J 98(9):854–862
Kumar A, Sandoe J, Kumar N (2005) Three cases of vertebral osteomyelitis caused by Streptococcus dysgalactiae subsp equisimilis. J Med Microbiol 54(11):1103–1105
Quesnele J, Dufton J, Stern P (2012) Spinal infection: a case report. J Can Chiropr Assoc 56(3):209–215
Sendi P, Bregenzer T, Zimmerli W (2008) Spinal epidural abscess in clinical practice. QJM 101(1):1–12
Kowalski TJ, Berbari EF, Huddleston PM et al (2006) Do follow-up imaging examinations provide useful prognostic information in patients with spine infection? Clin Infect Dis 43(2):172–179
Pineda C, Espinosa R, Pena A (2009) Radiographic imaging in osteomyelitis: the role of plain radiography, computed tomography, ultrasonography, magnetic resonance imaging, and scintigraphy. Semin Plast Surg 23(2):80–89
Schulte-Uentrop L, Goepfert MS (2010) Anaesthesia or sedation for MRI in children. Curr Opin Anaesthesiol 23(4):513–517
Schmidt MH, Marshall J, Downie J et al (2011) Pediatric magnetic resonance research and te minimal-risk standard. IRB 33(5):1–6
Ahmed SS, Unland T, Slaven JE et al (2014) Successful use of intravenous dexmedetomidine for magnetic resonance imaging sedation in autistic children. South Med J 107(9):559–564
Holland SK, Altaye M, Roberston S et al (2014) Data on the safety of repeated MRI in healthy children. Neuroimage Clin 9(4):526–530
Kitt E, Friderici J, Kleppel R et al (2015) Procedural sedation for MRI in children with ADHD. Paediatr Anaesth 25(10):1026–1032
Funding
No funding was received for this work.
Author information
Authors and Affiliations
Contributions
LLC: data collection, analysis, investigation, methodology, writing- original manuscript, writing- reviewing and editing, final approval. BJS: conceptualization, visualization, writing-reviewing and editing, final approval. KAW: analysis, methodology, writing- original manuscript, final approval. DJH: data acquisition, writing-reviewing and editing, final approval. MTH: data acquisition, writing- reviewing and editing, final approval. JBE: Data acquisition, writing- reviewing and editing, final approval. LIK: data acquisition, writing- reviewing and editing, final approval. BDS: data acquisition, writing- reviewing and editing, final approval. MPG: conceptualization, investigation, methodology, project administration, resources, supervision, visualization, data acquisition, writing- reviewing and editing, final approval.
Corresponding author
Ethics declarations
Conflicts of interest
No conflicts of interest or source of funding to declare.
Ethical approval
IRB approved by Boston Children’s Hospital.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Cohen, L.L., Shore, B.J., Williams, K.A. et al. Diagnosing and treating native spinal and pelvic osteomyelitis in adolescents. Spine Deform 8, 1001–1008 (2020). https://doi.org/10.1007/s43390-020-00110-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43390-020-00110-8