Abstract
Oral health is vital to overall well-being, with the human mouth being home to a myriad of microorganisms. Plaque biofilms, predominantly responsible for dental cavities, consist of diverse bacteria and fungi. These biofilms can lead to oral diseases, such as dental caries and periodontal diseases. In recent times, the spotlight has shifted to inorganic nanoparticles (NPs) as potential dental materials, attributed to their potent antibacterial properties which arise from their expansive-specific area, heightened charge density, and catalytic features. This review aims to explore the antimicrobial efficacy of inorganic NPs, discussing the range of oral diseases they combat and their underlying antibacterial mechanisms. Furthermore, it highlights the distinctive characteristics and applications of various inorganic NPs, with a particular emphasis on metal oxides and calcium phosphates. The review concludes by considering future prospects and developments in the realm of antibacterial inorganic NPs.









Similar content being viewed by others
References
H. Tuominen, J. Rautava, Oral microbiota and cancer development. Pathobiology 88, 116–126 (2020). https://doi.org/10.1159/000510979
S. Kitamoto, H. Nagao-Kitamoto, R. Hein, T.M. Schmidt, N. Kamada, The bacterial connection between the oral cavity and the gut diseases. J. Dent. Res. 99, 1021–1029 (2020). https://doi.org/10.1177/0022034520924633
M. Kim, H. Ashida, M. Ogawa, Y. Yoshikawa, H. Mimuro, C. Sasakawa, Bacterial interactions with the host epithelium. Cell Host Microbe 8, 20–35 (2010). https://doi.org/10.1016/j.chom.2010.06.006
P.D. Marsh, Dental plaque as a biofilm and a microbial community—implications for health and disease. BMC Oral Health 6(Suppl 1), S14 (2006). https://doi.org/10.1186/1472-6831-6-S1-S14
S.A.F.T.V. Hijum, S. Kralj, L.K. Ozimek, L. Dijkhuizen, I.G.H.V. Geel-Schutten, Structure–function relationships of glucansucrase and fructansucrase enzymes from lactic acid bacteria. Microbiol Mol Biol Rev 70, 157–176 (2006). https://doi.org/10.1128/mmbr.70.1.157-176.2006
M.I. Klein, S. Duarte, J. Xiao, S. Mitra, T.H. Foster, H. Koo, Structural and molecular basis of the role of starch and sucrose in Streptococcus mutans biofilm development. Appl. Environ. Microbiol. 75, 837–841 (2009). https://doi.org/10.1128/AEM.01299-08
P.D. Marsh, Dental plaque as a microbial biofilm. Caries Res. 38, 204–211 (2004). https://doi.org/10.1159/000077756
K. Hojo, S. Nagaoka, T. Ohshima, N. Maeda, Bacterial interactions in dental biofilm development. J. Dent. Res. 88, 982–990 (2009). https://doi.org/10.1177/0022034509346811
B. Nyvad, N. Takahashi, Integrated hypothesis of dental caries and periodontal diseases. J. Oral Microbiol. 12, 1710953 (2020). https://doi.org/10.1080/20002297.2019.1710953
P. Makvandi, U. Josic, M. Delfi, F. Pinelli, V. Jahed, E. Kaya, M. Ashrafizadeh, A. Zarepour, F. Rossi, A. Zarrabi, T. Agarwal, E.N. Zare, M. Ghomi, T. Kumar Maiti, L. Breschi, F.R. Tay, Drug delivery (nano)platforms for oral and dental applications: tissue regeneration, infection control, and cancer management. Adv. Sci. 8, 2004014 (2021). https://doi.org/10.1002/advs.202004014
J.M.V. Makabenta, A. Nabawy, C.-H. Li, S. Schmidt-Malan, R. Patel, V.M. Rotello, Nanomaterial-based therapeutics for antibiotic-resistant bacterial infections. Nat. Rev. Microbiol. 19, 23–36 (2021). https://doi.org/10.1038/s41579-020-0420-1
A. Król, P. Pomastowski, K. Rafińska, V. Railean-Plugaru, B. Buszewski, Zinc oxide nanoparticles: synthesis, antiseptic activity and toxicity mechanism. Adv. Colloid Interface Sci. 249, 37–52 (2017). https://doi.org/10.1016/j.cis.2017.07.033
D.-H. Kim, J. Bae, J.H. Heo, C.H. Park, E.B. Kim, J.H. Lee, Nanoparticles as next-generation tooth-whitening agents: progress and perspectives. ACS Nano 16, 10042–10065 (2022). https://doi.org/10.1021/acsnano.2c01412
Y. Wang, Y. Yang, Y. Shi, H. Song, C. Yu, Antibiotic-free antibacterial strategies enabled by nanomaterials: progress and perspectives. Adv. Mater. 32, 1904106 (2020). https://doi.org/10.1002/adma.201904106
I.R. Bordea, S. Candrea, G.T. Alexescu, S. Bran, M. Băciuț, G. Băciuț, O. Lucaciu, C.M. Dinu, D.A. Todea, Nano-hydroxyapatite use in dentistry: a systematic review. Drug Metab. Rev. 52, 319–332 (2020). https://doi.org/10.1080/03602532.2020.1758713
S. Kyrylenko, F. Warchoł, O. Oleshko, Y. Husak, A. Kazek-Kęsik, V. Korniienko, V. Deineka, M. Sowa, A. Maciej, J. Michalska, A. Jakóbik-Kolon, I. Matuła, M. Basiaga, V. Hulubnycha, A. Stolarczyk, M. Pisarek, O. Mishchenko, M. Pogorielov, W. Simka, Effects of the sources of calcium and phosphorus on the structural and functional properties of ceramic coatings on titanium dental implants produced by plasma electrolytic oxidation. Mater. Sci. Eng. C 119, 111607 (2021). https://doi.org/10.1016/j.msec.2020.111607
R.Y. Pelgrift, A.J. Friedman, Nanotechnology as a therapeutic tool to combat microbial resistance. Adv. Drug Deliv. Rev. 65, 1803–1815 (2013). https://doi.org/10.1016/j.addr.2013.07.011
Q. Sun, M. Duan, W. Fan, B. Fan, Ca–Si mesoporous nanoparticles with the optimal Ag–Zn ratio inhibit the Enterococcus faecalis infection of teeth through dentinal tubule infiltration: an in vitro and in vivo study. J. Mater. Chem. B 9, 2200–2211 (2021). https://doi.org/10.1039/D0TB02704A
Y. Gao, P. Huang, R. Chen, M. Wang, Y. Wang, Y. Sa, T. Jiang, Mesoporous calcium silicate nanoparticles for superficial dental tissue reconstruction, in vitro and in vivo. RSC Adv. 11, 24681–24693 (2021). https://doi.org/10.1039/D1RA02114A
C. Wu, J. Chang, W. Fan, Bioactive mesoporous calcium–silicate nanoparticles with excellent mineralization ability, osteostimulation, drug-delivery and antibacterial properties for filling apex roots of teeth. J. Mater. Chem. 22, 16801–16809 (2012). https://doi.org/10.1039/C2JM33387B
M. Duan, W. Fan, B. Fan, Mesoporous calcium–silicate nanoparticles loaded with low-dose triton-100+Ag+ to achieve both enhanced antibacterial properties and low cytotoxicity for dentin disinfection of human teeth. Pharmaceutics 13, 1518 (2021). https://doi.org/10.3390/pharmaceutics13091518
X. Li, M. Qi, C. Li, B. Dong, J. Wang, M.D. Weir, S. Imazato, L. Du, C.D. Lynch, L. Xu, Y. Zhou, L. Wang, H.H.K. Xu, Novel nanoparticles of cerium-doped zeolitic imidazolate frameworks with dual benefits of antibacterial and anti-inflammatory functions against periodontitis. J. Mater. Chem. B 7, 6955–6971 (2019). https://doi.org/10.1039/C9TB01743G
N. Li, L. Xie, Y. Wu, Y. Wu, Y. Liu, Y. Gao, J. Yang, X. Zhang, L. Jiang, Dexamethasone-loaded zeolitic imidazolate frameworks nanocomposite hydrogel with antibacterial and anti-inflammatory effects for periodontitis treatment. Mater. Today Bio 16, 100360 (2022). https://doi.org/10.1016/j.mtbio.2022.100360
L. Wang, F. Dai, Y. Yang, Z. Zhang, Zeolitic imidazolate framework-8 with encapsulated naringin synergistically improves antibacterial and osteogenic properties of Ti implants for osseointegration. ACS Biomater. Sci. Eng. 8, 3797–3809 (2022). https://doi.org/10.1021/acsbiomaterials.2c00154
P.D. Marsh, Dental plaque: biological significance of a biofilm and community life-style. J. Clin. Periodontol. 32(Suppl 6), 7–15 (2005). https://doi.org/10.1111/j.1600-051X.2005.00790.x
R. Huang, M. Li, R.L. Gregory, Bacterial interactions in dental biofilm. Virulence 2, 435–444 (2011). https://doi.org/10.4161/viru.2.5.16140
P.I. Diaz, N.I. Chalmers, A.H. Rickard, C. Kong, C.L. Milburn, R.J. Palmer Jr., P.E. Kolenbrander, Molecular characterization of subject-specific oral microflora during initial colonization of enamel. Appl. Environ. Microbiol. 72, 2837–2848 (2006). https://doi.org/10.1128/AEM.72.4.2837-2848.2006
B. Nyvad, M. Kilian, Microbiology of the early colonization of human enamel and root surfaces in vivo. Scand. J. Dent. Res. 95, 369–380 (1987). https://doi.org/10.1111/j.1600-0722.1987.tb01627.x
P.E. Kolenbrander, R.J. Palmer Jr., A.H. Rickard, N.S. Jakubovics, N.I. Chalmers, P.I. Diaz, Bacterial interactions and successions during plaque development. Periodontol. 2000(42), 47–79 (2006). https://doi.org/10.1111/j.1600-0757.2006.00187.x
P.D. Marsh, Are dental diseases examples of ecological catastrophes? Microbiology (Reading) 149, 279–294 (2003). https://doi.org/10.1099/mic.0.26082-0
J.A. Aas, B.J. Paster, L.N. Stokes, I. Olsen, F.E. Dewhirst, Defining the normal bacterial flora of the oral cavity. J. Clin. Microbiol. 43, 5721–5732 (2005). https://doi.org/10.1128/jcm.43.11.5721-5732.2005
B.E. Costa Oliveira, A.P. Ricomini Filho, R.A. Burne, L. Zeng, The route of sucrose utilization by Streptococcus mutans affects intracellular polysaccharide metabolism. Front. Microbiol. 12, 636684 (2021). https://doi.org/10.3389/fmicb.2021.636684
N. Takahashi, B. Nyvad, The role of bacteria in the caries process: ecological perspectives. J. Dent. Res. 90, 294–303 (2011). https://doi.org/10.1177/0022034510379602
W.J. Loesche, S.A. Syed, The predominant cultivable flora of carious plaque and carious dentine. Caries Res. 7, 201–216 (1973). https://doi.org/10.1159/000259844
A. Polizzi, M. Donzella, G. Nicolosi, S. Santonocito, P. Pesce, G. Isola, Drugs for the quorum sensing inhibition of oral biofilm: new frontiers and insights in the treatment of periodontitis. Pharmaceutics (2022). https://doi.org/10.3390/pharmaceutics14122740
B.L. Pihlstrom, B.S. Michalowicz, N.W. Johnson, Periodontal diseases. Lancet 366, 1809–1820 (2005). https://doi.org/10.1016/S0140-6736(05)67728-8
S.S. Socransky, A.D. Haffajee, Periodontal microbial ecology. Periodontol. 2000(38), 135–187 (2005). https://doi.org/10.1111/j.1600-0757.2005.00107.x
S.S. Socransky, A.D. Haffajee, M.A. Cugini, C. Smith, R.L. Kent Jr., Microbial complexes in subgingival plaque. J. Clin. Periodontol. 25, 134–144 (1998). https://doi.org/10.1111/j.1600-051X.1998.tb02419.x
R.M. Meffert, Periodontitis vs. peri-implantitis: The same disease? The same treatment? Crit. Rev. Oral Biol. Med. 7, 278–291 (1996). https://doi.org/10.1177/10454411960070030501
A. Skrzypczak-Wiercioch, K. Sałat, Lipopolysaccharide-induced model of neuroinflammation: mechanisms of action, research application and future directions for its use. Molecules (2022). https://doi.org/10.3390/molecules27175481
D. Dymock, A.J. Weightman, C. Scully, W.G. Wade, Molecular analysis of microflora associated with dentoalveolar abscesses. J. Clin. Microbiol. 34, 537–542 (1996). https://doi.org/10.1128/jcm.34.3.537-542.1996
B. Chi, M. Qi, H.K. Kuramitsu, Role of dentilisin in Treponema denticola epithelial cell layer penetration. Res. Microbiol. 154, 637–643 (2003). https://doi.org/10.1016/j.resmic.2003.08.001
T. Imamura, The role of gingipains in the pathogenesis of periodontal disease. J. Periodontol. 74, 111–118 (2003). https://doi.org/10.1902/jop.2003.74.1.111
J.C. Fenno, Treponema denticola interactions with host proteins. J. Oral Microbiol. (2012). https://doi.org/10.3402/jom.v4i0.9929
A. Amano, Molecular interaction of Porphyromonas gingivalis with host cells: implication for the microbial pathogenesis of periodontal disease. J. Periodontol. 74, 90–96 (2003). https://doi.org/10.1902/jop.2003.74.1.90
S. Yoon, Y. Chung, J.W. Lee, J. Chang, J.G. Han, J.H. Lee, Biologically benign multi-functional mesoporous silica encapsulated gold/silver nanorods for anti-bacterial applications by on-demand release of silver ions. BioChip J. 13, 362–369 (2019). https://doi.org/10.1007/s13206-019-3407-0
M. Godoy-Gallardo, U. Eckhard, L.M. Delgado, Y.J.D. de Roo Puente, M. Hoyos-Nogués, F.J. Gil, R.A. Perez, Antibacterial approaches in tissue engineering using metal ions and nanoparticles: from mechanisms to applications. Bioact. Mater. 6, 4470–4490 (2021). https://doi.org/10.1016/j.bioactmat.2021.04.033
E.Z. Gomaa, Silver nanoparticles as an antimicrobial agent: a case study on Staphylococcus aureus and Escherichia coli as models for Gram-positive and Gram-negative bacteria. J. Gen. Appl. Microbiol. 63, 36–43 (2017). https://doi.org/10.2323/jgam.2016.07.004
A. Abbaszadegan, Y. Ghahramani, A. Gholami, B. Hemmateenejad, S. Dorostkar, M. Nabavizadeh, H. Sharghi, The effect of charge at the surface of silver nanoparticles on antimicrobial activity against Gram-positive and Gram-negative bacteria: a preliminary study. J. Nanomater. 2015, 720654 (2015). https://doi.org/10.1155/2015/720654
Y. Qiao, L. Ma, Quantification of metal ion induced DNA damage with single cell array based assay. Analyst 138, 5713–5718 (2013). https://doi.org/10.1039/C3AN00967J
J.A. Lemire, J.J. Harrison, R.J. Turner, Antimicrobial activity of metals: mechanisms, molecular targets and applications. Nat. Rev. Microbiol. 11, 371–384 (2013). https://doi.org/10.1038/nrmicro3028
S. Cheeseman, A.J. Christofferson, R. Kariuki, D. Cozzolino, T. Daeneke, R.J. Crawford, V.K. Truong, J. Chapman, A. Elbourne, Antimicrobial metal nanomaterials: from passive to stimuli-activated applications. Adv. Sci. 7, 1902913 (2020). https://doi.org/10.1002/advs.201902913
Q.L. Feng, J. Wu, G.Q. Chen, F.Z. Cui, T.N. Kim, J.O. Kim, A mechanistic study of the antibacterial effect of silver ions on Escherichia coli and Staphylococcus aureus. J. Biomed. Mater. Res. 52, 662–668 (2000). https://doi.org/10.1002/1097-4636(20001215)52:4%3C662::AID-JBM10%3E3.0.CO;2-3
A. Ayala, M.F. Muñoz, S. Argüelles, Lipid peroxidation: production, metabolism, and signaling mechanisms of malondialdehyde and 4-hydroxy-2-nonenal. Oxid. Med. Cell. Longev. 2014, 360438 (2014). https://doi.org/10.1155/2014/360438
L. Wang, C. Hu, L. Shao, The antimicrobial activity of nanoparticles: present situation and prospects for the future. Int. J. Nanomed. 12, 1227–1249 (2017). https://doi.org/10.2147/IJN.S121956
S. Ahmad, H. Khan, U. Shahab, S. Rehman, Z. Rafi, M.Y. Khan, A. Ansari, Z. Siddiqui, J.M. Ashraf, S.M. Abdullah, S. Habib, M. Uddin, Protein oxidation: an overview of metabolism of Sulphur containing amino acid, cysteine. Front. Biosci. (Schol. Ed.) 9, 71–87 (2017). https://doi.org/10.2741/S474
R.L. Auten, J.M. Davis, Oxygen toxicity and reactive oxygen species: the devil is in the details. Pediatr. Res. 66, 121–127 (2009). https://doi.org/10.1203/PDR.0b013e3181a9eafb
W. Yang, C. Shen, Q. Ji, H. An, J. Wang, Q. Liu, Z. Zhang, Food storage material silver nanoparticles interfere with DNA replication fidelity and bind with DNA. Nanotechnology 20, 085102 (2009). https://doi.org/10.1088/0957-4484/20/8/085102
J.K. Patra, G. Das, L.F. Fraceto, E.V.R. Campos, M.D.P. Rodriguez-Torres, L.S. Acosta-Torres, L.A. Diaz-Torres, R. Grillo, M.K. Swamy, S. Sharma, S. Habtemariam, H.S. Shin, Nano based drug delivery systems: recent developments and future prospects. J. Nanobiotechnol. 16, 71 (2018). https://doi.org/10.1186/s12951-018-0392-8
R.P. Pandey, R. Mukherjee, A. Priyadarshini, A. Gupta, A. Vibhuti, E. Leal, U. Sengupta, V.M. Katoch, P. Sharma, C.E. Moore, V.S. Raj, X. Lyu, Potential of nanoparticles encapsulated drugs for possible inhibition of the antimicrobial resistance development. Biomed. Pharmacother. 141, 111943 (2021). https://doi.org/10.1016/j.biopha.2021.111943
M. Liu, X. Fang, Y. Yang, C. Wang, Peptide-enabled targeted delivery systems for therapeutic applications. Front. Bioeng. Biotechnol. (2021). https://doi.org/10.3389/fbioe.2021.701504
Z. Wei, Y. Zhou, R. Wang, J. Wang, Z. Chen, Aptamers as smart ligands for targeted drug delivery in cancer therapy. Pharmaceutics (2022). https://doi.org/10.3390/pharmaceutics14122561
H. Lim, J. Chang, K.-I. Kim, Y. Moon, S. Lee, B. Lee, J.H. Lee, J. Lee, On-chip selection of adenosine aptamer using graphene oxide-coated magnetic nanoparticles. Biomicrofluidics (2022). https://doi.org/10.1063/5.0095419
J.H. Lee, Y. Yeo, Controlled drug release from pharmaceutical nanocarriers. Chem. Eng. Sci. 125, 75–84 (2015). https://doi.org/10.1016/j.ces.2014.08.046
R. Wardlow, C. Bing, J. VanOsdol, D. Maples, M. Ladouceur-Wodzak, M. Harbeson, J. Nofiele, R. Staruch, A. Ramachandran, J. Malayer, R. Chopra, A. Ranjan, Targeted antibiotic delivery using low temperature-sensitive liposomes and magnetic resonance-guided high-intensity focused ultrasound hyperthermia. Int. J. Hyperthermia 32, 254–264 (2016). https://doi.org/10.3109/02656736.2015.1134818
M.J. Ndolomingo, N. Bingwa, R. Meijboom, Review of supported metal nanoparticles: synthesis methodologies, advantages and application as catalysts. J. Mater. Sci. 55, 6195–6241 (2020). https://doi.org/10.1007/s10853-020-04415-x
K.-I. Kim, S. Yoon, J. Chang, S. Lee, H.H. Cho, S.H. Jeong, K. Jo, J.H. Lee, Multifunctional heterogeneous carbon nanotube nanocomposites assembled by DNA-binding peptide anchors. Small 16, 1905821 (2020). https://doi.org/10.1002/smll.201905821
S.H. Kim, S. Oh, S. Chae, J.W. Lee, K.H. Choi, K.E. Lee, J. Chang, L. Shi, J.-Y. Choi, J.H. Lee, Exceptional mechanical properties of phase-separation-free Mo3Se3—chain-reinforced hydrogel prepared by polymer wrapping process. Nano Lett. 19, 5717–5724 (2019). https://doi.org/10.1021/acs.nanolett.9b02343
M.-H. Hong, J.H. Lee, H.S. Jung, H. Shin, H. Shin, Biomineralization of bone tissue: calcium phosphate-based inorganics in collagen fibrillar organic matrices. Biomater. Res. 26, 42 (2022). https://doi.org/10.1186/s40824-022-00288-0
J.H. Lee, G.S. Yi, J.W. Lee, D.J. Kim, Physicochemical characterization of porcine bone-derived grafting material and comparison with bovine xenografts for dental applications. J. Periodontal Implant Sci. 47, 388–401 (2017). https://doi.org/10.5051/jpis.2017.47.6.388
J.W. Lee, S. Chae, S. Oh, S.H. Kim, K.H. Choi, M. Meeseepong, J. Chang, N. Kim, K. Yong Ho, N.-E. Lee, J.H. Lee, J.-Y. Choi, Single-chain atomic crystals as extracellular matrix-mimicking material with exceptional biocompatibility and bioactivity. Nano Lett. 18, 7619–7627 (2018). https://doi.org/10.1021/acs.nanolett.8b03201
J.W. Lee, S. Chae, S. Oh, D.-H. Kim, S.H. Kim, S.J. Kim, J.-Y. Choi, J.H. Lee, S.Y. Song, Bioessential inorganic molecular wire-reinforced 3D-printed hydrogel scaffold for enhanced bone regeneration. Adv. Healthc. Mater. 12, 2201665 (2023). https://doi.org/10.1002/adhm.202201665
J.W. Lee, S. Chae, S. Oh, S.H. Kim, M. Meeseepong, K.H. Choi, J. Jeon, N.-E. Lee, S.Y. Song, J.H. Lee, J.-Y. Choi, Bio-essential inorganic molecular nanowires as a bioactive muscle extracellular-matrix-mimicking material. ACS Appl. Mater. Interfaces 13, 39135–39141 (2021). https://doi.org/10.1021/acsami.1c12440
M.J. Kim, D.H. Jung, C.Y. Lee, S. Hong, J.H. Heo, J.H. Lee, Structurally engineered silica shells on gold nanorods for biomedical applications. Small Struct. 4, 2300047 (2023). https://doi.org/10.1002/sstr.202300047
S. Yoon, B. Lee, C. Kim, J.H. Chang, M.J. Kim, H.B. Bae, K.E. Lee, W.K. Bae, J.H. Lee, Surface polarity-insensitive organosilicasome-based clustering of nanoparticles with intragap distance tunability. Chem. Mater. 33, 5257–5267 (2021). https://doi.org/10.1021/acs.chemmater.1c01339
B. Kang, M.-K. Shin, S. Han, I. Oh, E. Kim, J. Park, H.Y. Son, T. Kang, J. Jung, Y.-M. Huh, S. Haam, E.-K. Lim, Magnetic nanochain-based smart drug delivery system with remote tunable drug release by a magnetic field. BioChip J. 16, 280–290 (2022). https://doi.org/10.1007/s13206-022-00072-1
J.H. Heo, M. Sung, T.Q. Trung, Y. Lee, D.H. Jung, H. Kim, S. Kaushal, N.-E. Lee, J.W. Kim, J.H. Lee, S.-Y. Cho, Sensor design strategy for environmental and biological monitoring. EcoMat 5, e12332 (2023). https://doi.org/10.1002/eom2.12332
S. Kannappan, J. Chang, P.R. Sundharbaabu, J.H. Heo, W.-K. Sung, J.C. Ro, K.K. Kim, J.B.B. Rayappan, J.H. Lee, DNA-wrapped CNT sensor for small nucleic acid detection: influence of short complementary sequence. BioChip J. 16, 490–500 (2022). https://doi.org/10.1007/s13206-022-00088-7
R.R. Suresh, A.J. Kulandaisamy, N. Nesakumar, S. Nagarajan, J.H. Lee, J.B.B. Rayappan, Graphene quantum dots—hydrothermal green synthesis, material characterization and prospects for cervical cancer diagnosis applications: a review. ChemistrySelect 7, e202200655 (2022). https://doi.org/10.1002/slct.202200655
S.E. Heo, J.W. Ha, Single-particle study: refractive index sensitivity of localized surface plasmon resonance inflection points in mesoporous silica-coated gold nanorods. BioChip J. 16, 183–190 (2022). https://doi.org/10.1007/s13206-022-00061-4
G. Colon, B.C. Ward, T.J. Webster, Increased osteoblast and decreased Staphylococcus epidermidis functions on nanophase ZnO and TiO2. J. Biomed. Mater. Res. A 78A, 595–604 (2006). https://doi.org/10.1002/jbm.a.30789
P. Shankar, P. Srinivasan, B. Vutukuri, A.J. Kulandaisamy, G.K. Mani, K.J. Babu, J.H. Lee, J.B.B. Rayappan, Boron induced c-axis growth and ammonia sensing signatures of spray pyrolysis deposited ZnO thin films—relation between crystallinity and sensing. Thin Solid Films 746, 139126 (2022). https://doi.org/10.1016/j.tsf.2022.139126
P. Shankar, M.Q.H. Ishak, J.K. Padarti, N. Mintcheva, S. Iwamori, S.O. Gurbatov, J.H. Lee, S.A. Kulinich, ZnO@graphene oxide core@shell nanoparticles prepared via one-pot approach based on laser ablation in water. Appl. Surf. Sci. 531, 147365 (2020). https://doi.org/10.1016/j.apsusc.2020.147365
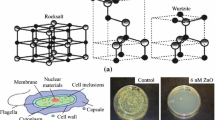
A. Sirelkhatim, S. Mahmud, A. Seeni, N.H.M. Kaus, L.C. Ann, S.K.M. Bakhori, H. Hasan, D. Mohamad, Review on zinc oxide nanoparticles: antibacterial activity and toxicity mechanism. Nanomicro Lett. 7, 219–242 (2015). https://doi.org/10.1007/s40820-015-0040-x
C. Pushpalatha, J. Suresh, V. Gayathri, S. Sowmya, D. Augustine, A. Alamoudi, B. Zidane, N.H. Mohammad-Albar, S. Patil, Zinc oxide nanoparticles: a review on its applications in dentistry. Front. Bioeng. Biotechnol. (2022). https://doi.org/10.3389/fbioe.2022.917990
E.H. Abdulkareem, K. Memarzadeh, R.P. Allaker, J. Huang, J. Pratten, D. Spratt, Anti-biofilm activity of zinc oxide and hydroxyapatite nanoparticles as dental implant coating materials. J. Dent. 43, 1462–1469 (2015). https://doi.org/10.1016/j.jdent.2015.10.010
Y. Wang, H. Hua, W. Li, R. Wang, X. Jiang, M. Zhu, Strong antibacterial dental resin composites containing cellulose nanocrystal/zinc oxide nanohybrids. J. Dent. 80, 23–29 (2019). https://doi.org/10.1016/j.jdent.2018.11.002
M.F. Gutiérrez, L.F. Alegría-Acevedo, L. Méndez-Bauer, J. Bermudez, A. Dávila-Sánchez, S. Buvinic, N. Hernández-Moya, A. Reis, A.D. Loguercio, P.V. Farago, J. Martin, E. Fernández, Biological, mechanical and adhesive properties of universal adhesives containing zinc and copper nanoparticles. J. Dent. 82, 45–55 (2019). https://doi.org/10.1016/j.jdent.2019.01.012
V. Andrade, A. Martínez, N. Rojas, H. Bello-Toledo, P. Flores, G. Sánchez-Sanhueza, A. Catalán, Antibacterial activity against Streptococcus mutans and diametrical tensile strength of an interim cement modified with zinc oxide nanoparticles and terpenes: an in vitro study. J. Prosthet. Dent. 119(862), e861-862.e867 (2018). https://doi.org/10.1016/j.prosdent.2017.09.015
P. Bhattacharya, A. Dey, S. Neogi, An insight into the mechanism of antibacterial activity by magnesium oxide nanoparticles. J. Mater. Chem. B 9, 5329–5339 (2021). https://doi.org/10.1039/D1TB00875G
D. Bouras, M. Fellah, A. Mecif, R. Barillé, A. Obrosov, M. Rasheed, High photocatalytic capacity of porous ceramic-based powder doped with MgO. J. Korean Ceram. Soc. 60, 155–168 (2023). https://doi.org/10.1007/s43207-022-00254-5
Y. He, S. Ingudam, S. Reed, A. Gehring, T.P. Strobaugh, P. Irwin, Study on the mechanism of antibacterial action of magnesium oxide nanoparticles against foodborne pathogens. J. Nanobiotechnol. 14, 54 (2016). https://doi.org/10.1186/s12951-016-0202-0
M.A. Kaiyum, A. Ahmed, M.H. Hasnat, S. Rahman, Effect of MgO on physical and mechanical properties of dental porcelain. J. Korean Ceram. Soc. 58, 42–49 (2021). https://doi.org/10.1007/s43207-020-00083-4
S. Varshney, A. Nigam, N. Mishra, S.J. Pawar, Microwave-assisted synthesis of magnesium oxide nanoflakes via green chemistry approach using Ficus Racemosa leaf extract: characterization and antibacterial activity. J. Korean Ceram. Soc. 60, 62–74 (2023). https://doi.org/10.1007/s43207-022-00236-7
A.-P. Rodríguez-Hernández, A.L. Vega-Jiménez, A.R. Vázquez-Olmos, M. Ortega-Maldonado, L.-A. Ximenez-Fyvie, Antibacterial properties in vitro of magnesium oxide nanoparticles for dental applications. Nanomaterials 13, 502 (2023). https://doi.org/10.3390/nano13030502
Y. Wang, Z. Wu, T. Wang, W. Tang, T. Li, H. Xu, H. Sun, Y. Lin, B.S.H. Tonin, Z. Ye, J. Fu, Bioactive dental resin composites with MgO nanoparticles. ACS Biomater. Sci. Eng. 9, 4632–4645 (2023). https://doi.org/10.1021/acsbiomaterials.3c00490
G.H. Naguib, H.M. Nassar, M.T. Hamed, Antimicrobial properties of dental cements modified with zein-coated magnesium oxide nanoparticles. Bioact. Mater. 8, 49–56 (2022). https://doi.org/10.1016/j.bioactmat.2021.06.011
A. Rangrazi, M.S. Daneshmand, K. Ghazvini, H. Shafaee, Effects of magnesium oxide nanoparticles incorporation on shear bond strength and antibacterial activity of an orthodontic composite: an in vitro study. Biomimetics 7, 133 (2022). https://doi.org/10.3390/biomimetics7030133
J. Choi, J. Kim, K. Han, U. Kim, Antibacterial behavior of copper glazes: effect of copper(II) oxide concentrations and sintering atmospheres. J. Korean Ceram. Soc. 58, 287–296 (2021). https://doi.org/10.1007/s43207-021-00112-w
S. Meghana, P. Kabra, S. Chakraborty, N. Padmavathy, Understanding the pathway of antibacterial activity of copper oxide nanoparticles. RSC Adv. 5, 12293–12299 (2015). https://doi.org/10.1039/C4RA12163E
M. Eshed, J. Lellouche, S. Matalon, A. Gedanken, E. Banin, Sonochemical coatings of ZnO and CuO nanoparticles inhibit Streptococcus mutans biofilm formation on teeth model. Langmuir 28, 12288–12295 (2012). https://doi.org/10.1021/la301432a
B. Ramazanzadeh, A. Jahanbin, M. Yaghoubi, N. Shahtahmassbi, K. Ghazvini, M. Shakeri, H. Shafaee, Comparison of antibacterial effects of ZnO and CuO nanoparticles coated brackets against Streptococcus Mutans. J. Dent. (Shiraz) 16, 200–205 (2015)
M. Eshed, J. Lellouche, A. Gedanken, E. Banin, A Zn-doped CuO nanocomposite shows enhanced antibiofilm and antibacterial activities against Streptococcus mutans compared to nanosized CuO. Adv. Funct. Mater. 24, 1382–1390 (2014). https://doi.org/10.1002/adfm.201302425
N.-D. Jaji, H.L. Lee, M.H. Hussin, H.M. Akil, M.R. Zakaria, M.B.H. Othman, Advanced nickel nanoparticles technology: from synthesis to applications. Nanotechnol. Rev. 9, 1456–1480 (2020). https://doi.org/10.1515/ntrev-2020-0109
J. Iqbal, B.A. Abbasi, T. Mahmood, S. Hameed, A. Munir, S. Kanwal, Green synthesis and characterizations of Nickel oxide nanoparticles using leaf extract of Rhamnus virgata and their potential biological applications. Appl. Organomet. Chem. 33, e4950 (2019). https://doi.org/10.1002/aoc.4950
N.C.Z. Moghadam, S.A. Jasim, F. Ameen, D.H. Alotaibi, M.A.L. Nobre, H. Sellami, M. Khatami, Nickel oxide nanoparticles synthesis using plant extract and evaluation of their antibacterial effects on Streptococcus mutans. Bioprocess Biosyst. Eng. 45, 1201–1210 (2022). https://doi.org/10.1007/s00449-022-02736-6
E. Nazaripour, F. Mosazadeh, S.S. Rahimi, H.Q. Alijani, E. Isaei, F. Borhani, S. Iravani, M. Ghasemi, M.R. Akbarizadeh, E. Azizi, F. Sharifi, M. Haghighat, S. Hadizadeh, M.D. Moghadam, M. Abdollahpour-Alitappeh, M. Khatami, Ferromagnetic nickel (II) oxide (NiO) nanoparticles: biosynthesis, characterization and their antibacterial activities. Rend. Lincei Sci. Fis. Nat. 33, 127–134 (2022). https://doi.org/10.1007/s12210-021-01042-9
S.V. Gudkov, D.A. Serov, M.E. Astashev, A.A. Semenova, A.B. Lisitsyn, Ag2O nanoparticles as a candidate for antimicrobial compounds of the new generation. Pharmaceuticals 15, 968 (2022). https://doi.org/10.3390/ph15080968
W. Shen, P. Li, H. Feng, Y. Ge, Z. Liu, L. Feng, The bactericidal mechanism of action against Staphylococcus aureus for AgO nanoparticles. Mater. Sci. Eng. C 75, 610–619 (2017). https://doi.org/10.1016/j.msec.2017.02.080
B.A. Abbasi, J. Iqbal, J.A. Nasir, S.A. Zahra, A. Shahbaz, S. Uddin, S. Hameed, F. Gul, S. Kanwal, T. Mahmood, Environmentally friendly green approach for the fabrication of silver oxide nanoparticles: characterization and diverse biomedical applications. Microsc. Res. Tech. 83, 1308–1320 (2020). https://doi.org/10.1002/jemt.23522
V. Manikandan, P. Velmurugan, J.-H. Park, W.-S. Chang, Y.-J. Park, P. Jayanthi, M. Cho, B.-T. Oh, Green synthesis of silver oxide nanoparticles and its antibacterial activity against dental pathogens. 3 Biotech 7, 72 (2017). https://doi.org/10.1007/s13205-017-0670-4
D. Carol López de, C. Matias Guerrero, B.M. Fernanda, S. Camilo, G. Maria José, Antimicrobial effect of titanium dioxide nanoparticles in antimicrobial resistance, ed. By M. Mihai, L. Swee Hua Erin, L. Kok-Song, C. Romeo-Teodor (IntechOpen, Rijeka, 2020). https://doi.org/10.5772/intechopen.90891
A.A. EL-Awady, H.N. Al-Khalifa, R.E. Mohamed, M.M. Ali, K.F. Abdallah, M.M. Hosny, A.A.S. Mohamed, K.S. ElHabbak, F.A. Hussein, Shear bond strength and antibacterial efficacy of cinnamon and titanium dioxide nanoparticles incorporated experimental orthodontic adhesive—an in vitro comparative study. Appl. Sci. 13, 6294 (2023). https://doi.org/10.3390/app13106294
F.L. Esteban Florez, R.D. Hiers, P. Larson, M. Johnson, E. O’Rear, A.J. Rondinone, S.S. Khajotia, Antibacterial dental adhesive resins containing nitrogen-doped titanium dioxide nanoparticles. Mater. Sci. Eng. C 93, 931–943 (2018). https://doi.org/10.1016/j.msec.2018.08.060
A. Zane, R. Zuo, F.A. Villamena, A. Rockenbauer, A.M. Digeorge Foushee, K. Flores, P.K. Dutta, A. Nagy, Biocompatibility and antibacterial activity of nitrogen-doped titanium dioxide nanoparticles for use in dental resin formulations. Int. J. Nanomed. 11, 6459–6470 (2016). https://doi.org/10.2147/IJN.S117584
C. Chambers, S.B. Stewart, B. Su, H.F. Jenkinson, J.R. Sandy, A.J. Ireland, Silver doped titanium dioxide nanoparticles as antimicrobial additives to dental polymers. Dent. Mater. 33, e115–e123 (2017). https://doi.org/10.1016/j.dental.2016.11.008
H.B. Dias, M.I.B. Bernardi, T.M. Bauab, A.C. Hernandes, A.N. de Souza Rastelli, Titanium dioxide and modified titanium dioxide by silver nanoparticles as an anti biofilm filler content for composite resins. Dent. Mater. 35, e36–e46 (2019). https://doi.org/10.1016/j.dental.2018.11.002
J. Sun, Y. Xu, B. Zhu, G. Gao, J. Ren, H. Wang, Y. Lin, B. Cao, Synergistic effects of titanium dioxide and cellulose on the properties of glassionomer cement. Dent. Mater. J. 38, 41–51 (2019). https://doi.org/10.4012/dmj.2018-001
L.S. Jairam, A. Chandrashekar, T.N. Prabhu, S.B. Kotha, M.S. Girish, I.M. Devraj, M. Dhanya-Shri, K. Prashantha, A review on biomedical and dental applications of cerium oxide nanoparticles—unearthing the potential of this rare earth metal. J. Rare Earths (2023). https://doi.org/10.1016/j.jre.2023.04.009
A. Arumugam, C. Karthikeyan, A.S. Haja Hameed, K. Gopinath, S. Gowri, V. Karthika, Synthesis of cerium oxide nanoparticles using Gloriosa superba L. leaf extract and their structural, optical and antibacterial properties. Mater. Sci. Eng. C 49, 408–415 (2015). https://doi.org/10.1016/j.msec.2015.01.042
R. Pol, K. Ashwini, Cerium oxide nanoparticles: synthesis, characterization and study of antimicrobial activity. J. Nanomater. Mol. Nanotechnol. (2017). https://doi.org/10.4172/2324-8777.1000219
M. Zhang, C. Zhang, X. Zhai, F. Luo, Y. Du, C. Yan, Antibacterial mechanism and activity of cerium oxide nanoparticles. Sci. China Mater. 62, 1727–1739 (2019). https://doi.org/10.1007/s40843-019-9471-7
D. Sanju, V.A. Kumari, T. Thomas, J.T. Thomas, R. Sujeer, Comparative evaluation of cerium oxide nanoparticles and calcium hydroxide as intracanal medicament against Enterococcus faecalis on tooth substrate: an: in vitro: study. Endodontology (2022). https://doi.org/10.4103/endo.endo_25_22
S. Qi, J. Wu, Y. Xu, Y. Zhang, R. Wang, K. Li, Y. Xu, Chemical stability and antimicrobial activity of plasma-sprayed cerium oxide-incorporated calcium silicate coating in dental implants. Implant Dent. 28, 564–570 (2019). https://doi.org/10.1097/id.0000000000000937
C.C.L. Dos-Santos, I.A. Passos-Farias, A.D.J.D. Reis-Albuquerque, P.M.D.F.E. Silva, G.M.D. Costa-One, F.C. Sampaio, Antimicrobial activity of nano cerium oxide (IV) (CeO2) against Streptococcus mutans. BMC Proc. 8, 48 (2014). https://doi.org/10.1186/1753-6561-8-S4-P48
F. Ostadhossein, S.K. Misra, I. Tripathi, V. Kravchuk, G. Vulugundam, D. LoBato, L.E. Selmic, D. Pan, Dual purpose hafnium oxide nanoparticles offer imaging Streptococcus mutans dental biofilm and fight it In vivo via a drug free approach. Biomaterials 181, 252–267 (2018). https://doi.org/10.1016/j.biomaterials.2018.07.053
N. Eliaz, N. Metoki, Calcium phosphate bioceramics: a review of their history, structure, properties, coating technologies and biomedical applications. Materials (Basel) (2017). https://doi.org/10.3390/ma10040334
S.V. Dorozhkin, A detailed history of calcium orthophosphates from 1770s till 1950. Mater. Sci. Eng. C Mater. Biol. Appl. 33, 3085–3110 (2013). https://doi.org/10.1016/j.msec.2013.04.002
M.I. Kay, R.A. Young, A.S. Posner, Crystal structure of hydroxyapatite. Nature 204, 1050–1052 (1964). https://doi.org/10.1038/2041050a0
A.S. Posner, F. Betts, Synthetic amorphous calcium phosphate and its relation to bone mineral structure. Acc. Chem. Res. 8, 273–281 (1975). https://doi.org/10.1021/ar50092a003
S.H. Kim, C.H. Park, J.H. Heo, J.H. Lee, Progress and perspectives of metal-ion-substituted hydroxyapatite for bone tissue engineering: comparison with hydroxyapatite. J. Korean Ceram. Soc. 59, 271–288 (2022). https://doi.org/10.1007/s43207-022-00198-w
C. Kim, J.W. Lee, J.H. Heo, C. Park, D.-H. Kim, G.S. Yi, H.C. Kang, H.S. Jung, H. Shin, J.H. Lee, Natural bone-mimicking nanopore-incorporated hydroxyapatite scaffolds for enhanced bone tissue regeneration. Biomater. Res. 26, 7 (2022). https://doi.org/10.1186/s40824-022-00253-x
J. Biggemann, P. Müller, D. Köllner, S. Simon, P. Hoffmann, P. Heik, J.H. Lee, T. Fey, Hierarchical surface texturing of hydroxyapatite ceramics: influence on the adhesive bonding strength of polymeric polycaprolactone. J. Funct. Biomater. 11, 73 (2020). https://doi.org/10.3390/jfb11040073
D.H. Kim, K.I. Kim, S. Yoon, H.J. Kim, J.S. Ahn, S.H. Jun, H.C. Kang, C. Pang, J. Kim, H.J. Cha, K.H. Han, D.M. Kim, J.H. Lee, Dental hetero-graft materials with nano hydroxyapatite surface treatment. J. Nanosci. Nanotechnol. 15, 7942–7949 (2015). https://doi.org/10.1166/jnn.2015.11197
N. Strutynska, A. Malyshenko, N. Tverdokhleb, M. Evstigneev, L. Vovchenko, Y. Prylutskyy, N. Slobodyanik, U. Ritter, Design, characterization and mechanical properties of new Na+, CO32−-apatite/alginate/C60 fullerene hybrid biocomposites. J. Korean Ceram. Soc. 58, 422–429 (2021). https://doi.org/10.1007/s43207-020-00107-z
A.A. Lopera, V.D.N. Bezzon, V. Ospina, J.L. Higuita-Castro, F.J. Ramirez, H.G. Ferraz, M.T.A. Orlando, C.G. Paucar, S.M. Robledo, C.P. Garcia, Obtaining a fused PLA-calcium phosphate-tobramycin-based filament for 3D printing with potential antimicrobial application. J. Korean Ceram. Soc. 60, 169–182 (2023). https://doi.org/10.1007/s43207-022-00255-4
Q. Guan, B. He, J. Huang, H.H. Lu, M. Wang, Hybrid ceramics-based cancer theranostics. J. Korean Ceram. Soc. 59, 401–426 (2022). https://doi.org/10.1007/s43207-022-00217-w
S.J. Kashyap, R. Sankannavar, G.M. Madhu, Hydroxyapatite nanoparticles synthesized with a wide range of Ca/P molar ratios and their structural, optical, and dielectric characterization. J. Korean Ceram. Soc. 59, 846–858 (2022). https://doi.org/10.1007/s43207-022-00225-w
K. Alagarsamy, V. Vishwakarma, G.S. Kaliaraj, V. Kanagasabai, S. Ramasamy, Investigating biological impact of HAp from goat femur reinforced with Zr–Ag for bone tissue engineering application. J. Korean Ceram. Soc. 59, 480–493 (2022). https://doi.org/10.1007/s43207-022-00199-9
M. Mudhafar, I. Zainol, H.A. Alsailawi, C.N. Aiza Jaafar, Synthesis and characterization of fish scales of hydroxyapatite/collagen–silver nanoparticles composites for the applications of bone filler. J. Korean Ceram. Soc. 59, 229–239 (2022). https://doi.org/10.1007/s43207-021-00154-0
A. Kovtun, D. Kozlova, K. Ganesan, C. Biewald, N. Seipold, P. Gaengler, W.H. Arnold, M. Epple, Chlorhexidine-loaded calcium phosphate nanoparticles for dental maintenance treatment: combination of mineralising and antibacterial effects. RSC Adv. 2, 870–875 (2012). https://doi.org/10.1039/C1RA00955A
J. Wu, M.D. Weir, M.A.S. Melo, H.H.K. Xu, Development of novel self-healing and antibacterial dental composite containing calcium phosphate nanoparticles. J. Dent. 43, 317–326 (2015). https://doi.org/10.1016/j.jdent.2015.01.009
Y. Li, X. Hu, J. Ruan, D.D. Arola, C. Ji, M.D. Weir, T.W. Oates, X. Chang, K. Zhang, H.H.K. Xu, Bonding durability, antibacterial activity and biofilm pH of novel adhesive containing antibacterial monomer and nanoparticles of amorphous calcium phosphate. J. Dent. 81, 91–101 (2019). https://doi.org/10.1016/j.jdent.2018.12.013
R. AlSahafi, A.A. Balhaddad, H. Mitwalli, M.S. Ibrahim, M.A.S. Melo, T.W. Oates, H.H.K. Xu, M.D. Weir, Novel crown cement containing antibacterial monomer and calcium phosphate nanoparticles. Nanomaterials (Basel) (2020). https://doi.org/10.3390/nano10102001
C. Chen, M.D. Weir, L. Cheng, N.J. Lin, S. Lin-Gibson, L.C. Chow, X. Zhou, H.H.K. Xu, Antibacterial activity and ion release of bonding agent containing amorphous calcium phosphate nanoparticles. Dent. Mater. 30, 891–901 (2014). https://doi.org/10.1016/j.dental.2014.05.025
Y. Li, X. Hu, Y. Xia, Y. Ji, J. Ruan, M.D. Weir, X. Lin, Z. Nie, N. Gu, R. Masri, X. Chang, H.H.K. Xu, Novel magnetic nanoparticle-containing adhesive with greater dentin bond strength and antibacterial and remineralizing capabilities. Dent. Mater. 34, 1310–1322 (2018). https://doi.org/10.1016/j.dental.2018.06.001
M.A.S. Melo, L. Cheng, K. Zhang, M.D. Weir, L.K.A. Rodrigues, H.H.K. Xu, Novel dental adhesives containing nanoparticles of silver and amorphous calcium phosphate. Dent. Mater. 29, 199–210 (2013). https://doi.org/10.1016/j.dental.2012.10.005
A. Shakerimoghaddam, H. Safardoust-Hojaghan, O. Amiri, M. Salavati-Niasari, A. Khorshidi, A. Khaledi, Ca19Zn2(PO4)14 Nanoparticles: synthesis, characterization and its effect on the colonization of Streptococcus mutans on tooth surface. J. Mol. Liq. 350, 118507 (2022). https://doi.org/10.1016/j.molliq.2022.118507
Q. Wang, P. Li, P. Tang, X. Ge, F. Ren, C. Zhao, J. Fang, K. Wang, L. Fang, Y. Li, C. Bao, X. Lu, K. Duan, Experimental and simulation studies of strontium/fluoride-codoped hydroxyapatite nanoparticles with osteogenic and antibacterial activities. Colloids Surf. B 182, 110359 (2019). https://doi.org/10.1016/j.colsurfb.2019.110359
X. Ge, Y. Leng, C. Bao, S.L. Xu, R. Wang, F. Ren, Antibacterial coatings of fluoridated hydroxyapatite for percutaneous implants. J. Biomed. Mater. Res. A 95A, 588–599 (2010). https://doi.org/10.1002/jbm.a.32862
M. Ai, Z. Du, S. Zhu, H. Geng, X. Zhang, Q. Cai, X. Yang, Composite resin reinforced with silver nanoparticles–laden hydroxyapatite nanowires for dental application. Dent. Mater. 33, 12–22 (2017). https://doi.org/10.1016/j.dental.2016.09.038
Y. Zhou, J. Deng, Y. Zhang, C. Li, Z. Wei, J. Shen, J. Li, F. Wang, B. Han, D. Chen, C. Fan, H. Zhang, K. Liu, Y. Wei, Engineering DNA-guided hydroxyapatite bulk materials with high stiffness and outstanding antimicrobial ability for dental inlay applications. Adv. Mater. 34, 2202180 (2022). https://doi.org/10.1002/adma.202202180
A.C.P. Janini, G.F. Bombarda, L.E. Pelepenko, M.A. Marciano, Antimicrobial activity of calcium silicate-based dental materials: a literature review. Antibiotics 10, 865 (2021). https://doi.org/10.3390/antibiotics10070865
O.M. Yaghi, G. Li, H. Li, Selective binding and removal of guests in a microporous metal–organic framework. Nature 378, 703–706 (1995). https://doi.org/10.1038/378703a0
B. Chen, Z. Yang, Y. Zhu, Y. Xia, Zeolitic imidazolate framework materials: recent progress in synthesis and applications. J. Mater. Chem. A 2, 16811–16831 (2014). https://doi.org/10.1039/C4TA02984D
N. Batool, S. Yoon, S. Imdad, M. Kong, H. Kim, S. Ryu, J.H. Lee, A.K. Chaurasia, K.K. Kim, An antibacterial nanorobotic approach for the specific targeting and removal of multiple drug-resistant Staphylococcus aureus. Small 17, 2100257 (2021). https://doi.org/10.1002/smll.202100257
K.M. Reddy, K. Feris, J. Bell, D.G. Wingett, C. Hanley, A. Punnoose, Selective toxicity of zinc oxide nanoparticles to prokaryotic and eukaryotic systems. Appl. Phys. Lett. (2007). https://doi.org/10.1063/1.2742324
G. Applerot, J. Lellouche, A. Lipovsky, Y. Nitzan, R. Lubart, A. Gedanken, E. Banin, Understanding the antibacterial mechanism of CuO nanoparticles: revealing the route of induced oxidative stress. Small 8, 3326–3337 (2012). https://doi.org/10.1002/smll.201200772
A. Morgan, Vital guide to preventing dental caries. Vital 5, 21–24 (2008). https://doi.org/10.1038/vital840
P. Abbott, C. Yu, A clinical classification of the status of the pulp and the root canal system. Aust. Dent. J. 52, S17–S31 (2007). https://doi.org/10.1111/j.1834-7819.2007.tb00522.x
T. Madiba, A. Bhayat, Periodontal disease—risk factors and treatment options. S. Afr. Dent. J. 73, 571–575 (2018). https://doi.org/10.17159/2519-0105/2018/v73no9a5
D. Rokaya, V. Srimaneepong, W. Wisitrasameewon, M. Humagain, P. Thunyakitpisal, Peri-implantitis update: risk indicators, diagnosis, and treatment. Eur. J. Dent 14, 672–682 (2020). https://doi.org/10.1055/s-0040-1715779
Acknowledgements
This research was supported by the Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Science and ICT (NRF-2020R1A2C2006100) and the Ministry of Education (NRF-2019R1A6A1A03033215). In addition, this study was supported by the Bio & Medical Technology Development Program (NRF-2022M3A9G8017220) of the National Research Foundation (NRF), funded by the Ministry of Science and ICT. J.H.H. acknowledges the support of the NRF funded by the Ministry of Education through the Basic Science Research Program (NRF2022R1C1C2002823).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no known conflicting financial interests or personal relationships that could have influenced the work reported in this paper.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kim, DH., Kim, J., Lee, C.Y. et al. Advancing oral health: the antimicrobial power of inorganic nanoparticles. J. Korean Ceram. Soc. 61, 201–223 (2024). https://doi.org/10.1007/s43207-023-00358-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43207-023-00358-6