Abstract
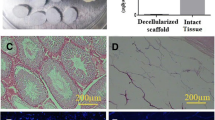
In vitro spermatogenesis and xenotransplantation of the immature testicular tissues (ITT) are the experimental approaches that have been developed for creating seminiferous tubules-like functional structures in vitro and keeping the integrity of the ITTs in vivo, respectively. These strategies are rapidly developing in response to the growing prevalence of infertility in adolescent boys undergoing cancer treatment, by the logic that there is no sperm cryopreservation option for them. Recently, with the advances made in the field of tissue engineering and biomaterials, these methods have achieved promising results for fertility preservation. Due to the importance of extracellular matrix for the formation of vascular bed around the grafted ITTs and also the creation of spatial arrangements between Sertoli cells and germ cells, today it is clear that the scaffold plays a very important role in the success of these methods. Decellularized extracellular matrix (dECM) as a biocompatible, functionally graded, and biodegradable scaffold with having tissue-specific components and growth factors can support reorganization and physiologic processes of originated cells. This review discusses the common protocols for the tissue decellularization, sterilization, and hydrogel formation of the decellularized and lyophilized tissues as well as in vitro and in vivo studies on the use of the testis-derived dECM for testicular organoids.


Similar content being viewed by others
Abbreviations
- ITT:
-
Immature testicular tissues
- dECM:
-
Decellularized extracellular matrix
- SSCs:
-
Spermatogonial stem cells
- ECM:
-
Extracellular matrix
- GAGs:
-
Glycosaminoglycans
- DTM:
-
Decellularized testicular matrix
References
Ibtisham F, Wu J, Xiao M, An L, Banker Z, Nawab A, et al. Progress and future prospect of in vitro spermatogenesis. Oncotarget. 2017;8(39):66709–27.
Stukenborg J-B, Schlatt S, Simoni M, Yeung C-H, Elhija MA, Luetjens CM, et al. New horizons for in vitro spermatogenesis? An update on novel three-dimensional culture systems as tools for meiotic and post-meiotic differentiation of testicular germ cells. 2009;15(9):521–9.
Goossens E, Jahnukainen K, Mitchell R, Van Pelt A, Pennings G, Rives N, et al. Fertility preservation in boys: recent developments and new insights. 2020;2020(3):hoaa016.
Del Vento F, Vermeulen M, De Michele F, Giudice MG, Poels J, Des Rieux A, et al. Tissue engineering to improve immature testicular tissue and cell transplantation outcomes: one step closer to fertility restoration for prepubertal boys exposed to gonadotoxic treatments. 2018;19(1):286.
Gholami K. Experimental approaches for fertility preservation in prepubertal boys undergoing oncological therapy. 2020.
Wyns C, Kanbar M, Giudice MG, Poels JJHru. Fertility preservation for prepubertal boys: lessons learned from the past and update on remaining challenges towards clinical translation. 2021;27(3):433–59.
Giudice MG, De Michele F, Poels J, Vermeulen M, Wyns CJScr. Update on fertility restoration from prepubertal spermatogonial stem cells: how far are we from clinical practice? 2017;21:171–7.
Demeestere I, Simon P, Dedeken L, Moffa F, Tsépélidis S, Brachet C, et al. Live birth after autograft of ovarian tissue cryopreserved during childhood. 2015;30(9):2107–9.
Wyns C, Curaba M, Martinez-Madrid B, Van Langendonckt A, François-Xavier W, Donnez JJHr. Spermatogonial survival after cryopreservation and short-term orthotopic immature human cryptorchid testicular tissue grafting to immunodeficient mice. 2007;22(6):1603–11.
Goossens E, Geens M, De Block G, Tournaye HJF, sterility. Spermatogonial survival in long-term human prepubertal xenografts. 2008;90(5):2019–22.
Sato Y, Nozawa S, Yoshiike M, Arai M, Sasaki C, Iwamoto TJHr. Xenografting of testicular tissue from an infant human donor results in accelerated testicular maturation. 2010;25(5):1113–22.
Van Eyck A-S, Jordan BF, Gallez B, Heilier J-F, Van Langendonckt A, Donnez JJF, et al. Electron paramagnetic resonance as a tool to evaluate human ovarian tissue reoxygenation after xenografting. 2009;92(1):374–81.
Poels J, Abou-Ghannam G, Herman S, Van Langendonckt A, Wese F-X, Wyns CJFis. In search of better spermatogonial preservation by supplementation of cryopreserved human immature testicular tissue xenografts with N-acetylcysteine and testosterone. 2014;1:47.
Poels J, Abou-Ghannam G, Decamps A, Leyman M, des Rieux A, Wyns CJJoCR. Transplantation of testicular tissue in alginate hydrogel loaded with VEGF nanoparticles improves spermatogonial recovery. 2016;234:79–89.
Del Vento F, Vermeulen M, Ucakar B, Poels J, des Rieux A, Wyns CJIjoms. Significant benefits of nanoparticles containing a necrosis inhibitor on mice testicular tissue autografts outcomes. 2019;20(23):5833.
Del Vento F, Poels J, Vermeulen M, Ucakar B, Giudice MG, Kanbar M, et al. Accelerated and improved vascular maturity after transplantation of testicular tissue in hydrogels supplemented with VEGF-and PDGF-loaded nanoparticles. 2021;22(11):5779.
Del Vento F, Vermeulen M, Poels J, Wyns C, editors. Encapsulation of mice immature testicular tissue in alginate supplemented with nanoparticles delivering a necrosis inhibitor improved spermatogonial survival and seminiferous tubule integrity in autografts. Human Reproduction. Oxford: Oxford Univ Press; 2019
Stukenborg J-B, Jahnukainen K. In vitro spermatogenesis and its potential clinical implication for patients. Genetics of Human Infertility. 21: Karger Publishers; 2017. p. 162–72.
Lee J-H, Gye MC, Choi KW, Hong JY, Lee YB, Park D-W, et al. In vitro differentiation of germ cells from nonobstructive azoospermic patients using three-dimensional culture in a collagen gel matrix. 2007;87(4):824–33.
Lee JH, Kim HJ, Kim H, Lee SJ, Gye MCJB. In vitro spermatogenesis by three-dimensional culture of rat testicular cells in collagen gel matrix. 2006;27(14):2845–53.
Baert Y, Dvorakova-Hortova K, Margaryan H, Goossens EJB. Mouse in vitro spermatogenesis on alginate-based 3D bioprinted scaffolds. 2019;11(3):035011.
Huleihel M, Nourashrafeddin S, Plant TM. Application of three-dimensional culture systems to study mammalian spermatogenesis, with an emphasis on the rhesus monkey (Macaca mulatta). Asian J Androl. 2015;17(6):972.
Gholami K, Pourmand G, Koruji M, Ashouri S, Abbasi MJScr, therapy. Organ culture of seminiferous tubules using a modified soft agar culture system. 2018;9(1):249.
Gholami K, Pourmand G, Koruji M, Sadighigilani M, Navid S, Izadyar F, et al. Efficiency of colony formation and differentiation of human spermatogenic cells in two different culture systems. 2018;18(4):397–403.
Jabari A, Gilani MAS, Koruji M, Gholami K, Mohsenzadeh M, Khadivi F, et al. Three-dimensional co-culture of human spermatogonial stem cells with Sertoli cells in soft agar culture system supplemented by growth factors and Laminin. 2020;122(5):151572.
Farmani AR, Nekoofar MH, Ebrahimi Barough S, Azami M, Rezaei N, Najafipour S, et al. Application of platelet rich fibrin in tissue engineering: focus on bone regeneration. 2021;32(2):183–8.
Sato T, Katagiri K, Gohbara A, Inoue K, Ogonuki N, Ogura A, et al. In vitro production of functional sperm in cultured neonatal mouse testes. 2011;471(7339):504–7.
Mendibil U, Ruiz-Hernandez R, Retegi-Carrion S, Garcia-Urquia N, Olalde-Graells B, Abarrategi AJIJoMS. Tissue-specific decellularization methods: rationale and strategies to achieve regenerative compounds. 2020;21(15):5447.
Hernandez MJ, Yakutis GE, Zelus EI, Hill RC, Dzieciatkowska M, Hansen KC, et al. Manufacturing considerations for producing and assessing decellularized extracellular matrix hydrogels. 2020;171:20–7.
Cartmell JS, Dunn MGJJoBMRAOJoTSfB, The Japanese society for biomaterials, biomaterials TASf, Biomaterials tKSf. Effect of chemical treatments on tendon cellularity and mechanical properties. 2000;49(1):134–40.
Woods T, Gratzer PFJB. Effectiveness of three extraction techniques in the development of a decellularized bone–anterior cruciate ligament–bone graft. 2005;26(35):7339–49.
Luo Z, Bian Y, Su W, Shi L, Li S, Song Y, et al. Comparison of various reagents for preparing a decellularized porcine cartilage scaffold. 2019;11(3):1417.
Chen R-N, Ho H-O, Tsai Y-T, Sheu M-TJB. Process development of an acellular dermal matrix (ADM) for biomedical applications. 2004;25(13):2679–86.
Schmitt A, Csiki R, Tron A, Saldamli B, Tübel J, Florian K, et al. Optimized protocol for whole organ decellularization. 2017;22(1):1–9.
Giraldo-Gomez D, Leon-Mancilla B, Del Prado-Audelo M, Sotres-Vega A, Villalba-Caloca J, Garciadiego-Cazares D, et al. Trypsin as enhancement in cyclical tracheal decellularization: morphological and biophysical characterization. 2016;59:930–7.
Caralt M, Uzarski JS, Iacob S, Obergfell KP, Berg N, Bijonowski BM, et al. Optimization and critical evaluation of decellularization strategies to develop renal extracellular matrix scaffolds as biological templates for organ engineering and transplantation. 2015;15(1):64-75.
Waletzko J, Dau M, Seyfarth A, Springer A, Frank M, Bader R, et al. Devitalizing effect of high hydrostatic pressure on human cells—influence on cell death in osteoblasts and chondrocytes. 2020;21(11):3836.
Rieder E, Kasimir M-T, Silberhumer G, Seebacher G, Wolner E, Simon P, et al. Decellularization protocols of porcine heart valves differ importantly in efficiency of cell removal and susceptibility of the matrix to recellularization with human vascular cells. 2004;127(2):399-405.
Poon CJ, Cotta MVPE, Sinha S, Palmer JA, Woods AA, Morrison WA, et al. Preparation of an adipogenic hydrogel from subcutaneous adipose tissue. 2013;9(3):5609-20.
Cheng J, Wang C, Gu YJB. Combination of freeze-thaw with detergents: a promising approach to the decellularization of porcine carotid arteries. 2019;30(2):191-205.
Cornelison R, Wellman S, Park J, Porvasnik S, Song Y, Wachs R, et al. Development of an apoptosis-assisted decellularization method for maximal preservation of nerve tissue structure. 2018;77:116-26.
Vermeulen M, Del Vento F, Kanbar M, Pyr dit Ruys S, Vertommen D, Poels J, et al. Generation of organized porcine testicular organoids in solubilized hydrogels from decellularized extracellular matrix. 2019;20(21):5476.
Tao M, Ao T, Mao X, Yan X, Javed R, Hou W, et al. Sterilization and disinfection methods for decellularized matrix materials: review, consideration and proposal. 2021;6(9):2927–45.
Somers P, Cuvelier CA, Somer FD, Cornelissen M, Cox E, Verloo M, et al. Gamma radiation alters the ultrastructure in tissue-engineered heart valve scaffolds. 2009;15(11):3597-604.
Yaldiz B, Saglam-Metiner P, Cam SB, Korkusuz P, Yesil-Celiktas OJTJoSF. Effect of sterilization methods on the mechanical stability and extracellular matrix constituents of decellularized brain tissues. 2021:105299.
White LJ, Keane TJ, Smoulder A, Zhang L, Castleton AA, Reing JE, et al. The impact of sterilization upon extracellular matrix hydrogel structure and function. 2018;2:11-20.
Giobbe GG, Crowley C, Luni C, Campinoti S, Khedr M, Kretzschmar K, et al. Extracellular matrix hydrogel derived from decellularized tissues enables endodermal organoid culture. 2019;10(1):1-14.
Claudio-Rizo JA, Delgado J, Quintero-Ortega IA, Mata-Mata JL, Mendoza-Novelo BJH. Decellularized ECM-derived hydrogels: modification and properties. 2018;1.
Gaetani R, Aude S, DeMaddalena LL, Strassle H, Dzieciatkowska M, Wortham M, et al. Evaluation of different decellularization protocols on the generation of pancreas-derived hydrogels. 2018;24(12):697-708.
Reuter K, Schlatt S, Ehmcke J, Wistuba JJS. Fact or fiction: in vitro spermatogenesis. 2012;2(4):245-52.
Kanbar M, De Michele F, Giudice MG, Desmet L, Poels J, Wyns CJHR. Long-term follow-up of boys who have undergone a testicular biopsy for fertility preservation. 2021;36(1):26-39.
Oliver E, Stukenborg JBJA. Rebuilding the human testis in vitro. 2020;8(4):825-34.
Sato T, Katagiri K, Kojima K, Komeya M, Yao M, Ogawa TJPo. In vitro spermatogenesis in explanted adult mouse testis tissues. 2015;10(6):e0130171.
Komeya M, Kimura H, Nakamura H, Yokonishi T, Sato T, Kojima K, et al. Long-term ex vivo maintenance of testis tissues producing fertile sperm in a microfluidic device. 2016;6(1):1-10.
Yokonishi T, Sato T, Komeya M, Katagiri K, Kubota Y, Nakabayashi K, et al. Offspring production with sperm grown in vitro from cryopreserved testis tissues. 2014;5(1):1-6.
Edmondson R, Broglie JJ, Adcock AF, Yang LJA. Three-dimensional cell culture systems and their applications in drug discovery and cell-based biosensors. 2014;12(4):207-18.
Yokonishi T, Sato T, Katagiri K, Komeya M, Kubota Y, Ogawa TJBor. In vitro reconstruction of mouse seminiferous tubules supporting germ cell differentiation. 2013;89(1):15, 1–6.
Nelson SR, Zhang C, Roche S, O’Neill F, Swan N, Luo Y, et al. Modelling of pancreatic cancer biology: transcriptomic signature for 3D PDX-derived organoids and primary cell line organoid development. 2020;10(1):1–12.
Zhang W, Huang G, Xu FJFiB, Biotechnology. Engineering biomaterials and approaches for mechanical stretching of cells in three dimensions. 2020;8.
Saydé T, El Hamoui O, Alies B, Gaudin K, Lespes G, Battu SJN. Biomaterials for three-dimensional cell culture: from applications in oncology to nanotechnology. 2021;11(2):481.
Liu Y, Hsu S-hJFic. Synthesis and biomedical applications of self-healing hydrogels. 2018;6:449.
Varaprasad K, Jayaramudu T, Kanikireddy V, Toro C, Sadiku ERJCp. Alginate-based composite materials for wound dressing application: a mini review. 2020;236:116025.
Kaczmarek-Pawelska A. Alginate-based hydrogels in regenerative medicine. Alginates-recent uses of this natural polymer: IntechOpen; 2019.
Kanbar M, Vermeulen M, Wyns CJR. Organoids as tools to investigate the molecular mechanisms of male infertility and its treatments. 2021;161(5):R103-R12.
Kusindarta DL, Wihadmadyatami HJTr. The role of extracellular matrix in tissue regeneration. 2018;65.
Nair M, Best SM, Cameron REJAS. Crosslinking collagen constructs: achieving cellular selectivity through modifications of physical and chemical properties. 2020;10(19):6911.
Lee J, Edwards H, Pereira C, Samii SJJoMSMiM. Crosslinking of tissue-derived biomaterials in 1-ethyl-3-(3-dimethylaminopropyl)-carbodiimide (EDC). 1996;7(9):531–41.
Výborný K, Vallová J, Kočí Z, Kekulová K, Jiráková K, Jendelová P, et al. Genipin and EDC crosslinking of extracellular matrix hydrogel derived from human umbilical cord for neural tissue repair. 2019;9(1):1-15.
Zhang W, Du A, Liu S, Lv M, Chen SJRT. Research progress in decellularized extracellular matrix-derived hydrogels. 2021;18:88-96.
Lee HJ, Mun S, Pham DM, Kim PJABS, Engineering. Extracellular matrix-based hydrogels to tailoring tumor organoids. 2021.
Vermeulen M, Del Vento F, De Michele F, Poels J, Wyns CJIjoms. Development of a cytocompatible scaffold from pig immature testicular tissue allowing human Sertoli cell attachment, proliferation and functionality. 2018;19(1):227.
Pendergraft SS, Sadri-Ardekani H, Atala A, Bishop CEJBoR. Three-dimensional testicular organoid: a novel tool for the study of human spermatogenesis and gonadotoxicity in vitro. 2017;96(3):720-32.
Sakib S, Uchida A, Valenzuela-Leon P, Yu Y, Valli-Pulaski H, Orwig K, et al. Formation of organotypic testicular organoids in microwell culture. 2019;100(6):1648-60.
Baert Y, De Kock J, Alves-Lopes JP, Söder O, Stukenborg J-B, Goossens EJSCR. Primary human testicular cells self-organize into organoids with testicular properties. 2017;8(1):30-8.
Alves-Lopes JP, Söder O, Stukenborg J-BJB. Testicular organoid generation by a novel in vitro three-layer gradient system. 2017;130:76-89.
Zhang J, Hatakeyama J, Eto K, Abe S-iJG, endocrinology c. Reconstruction of a seminiferous tubule-like structure in a 3 dimensional culture system of re-aggregated mouse neonatal testicular cells within a collagen matrix. 2014;205:121–32.
Strange DP, Zarandi NP, Trivedi G, Atala A, Bishop CE, Sadri-Ardekani H, et al. Human testicular organoid system as a novel tool to study Zika virus pathogenesis. 2018;7(1):1-7.
Goldsmith TM, Sakib S, Webster D, Carlson DF, Van der Hoorn F, Dobrinski IJC, et al. A reduction of primary cilia but not hedgehog signaling disrupts morphogenesis in testicular organoids. 2020;380(1):191-200.
Bhang DH, Kim B-J, Kim BG, Schadler K, Baek K-H, Kim YH, et al. Testicular endothelial cells are a critical population in the germline stem cell niche. 2018;9(1):1-16.
Huleihel M, Nourashrafeddin S, Plant TMJAjoa. Application of three-dimensional culture systems to study mammalian spermatogenesis, with an emphasis on the rhesus monkey (Macaca mulatta). 2015;17(6):972.
Abofoul-Azab M, Lunenfeld E, Levitas E, Zeadna A, Younis JS, Bar-Ami S, et al. Identification of premeiotic, meiotic, and postmeiotic cells in testicular biopsies without sperm from Sertoli cell-only syndrome patients. 2019;20(3):470.
Elhija MA, Lunenfeld E, Schlatt S, Huleihel MJAjoa. Differentiation of murine male germ cells to spermatozoa in a soft agar culture system. 2012;14(2):285.
Stukenborg JB, Wistuba J, Luetjens CM, Elhija MA, Huleihel M, Lunenfeld E, et al. Coculture of spermatogonia with somatic cells in a novel three‐dimensional soft‐agar‐culture‐system. 2008;29(3):312-29.
Movassagh SA, Movassagh SA, Dehkordi MB, Pourmand G, Gholami K, Talebi A, et al. Isolation, identification and differentiation of human spermatogonial cells on three-dimensional decellularized sheep testis. 2020;122(8):151623.
Legendre A, Froment P, Desmots S, Lecomte A, Habert R, Lemazurier EJB. An engineered 3D blood-testis barrier model for the assessment of reproductive toxicity potential. 2010;31(16):4492–505.
Shinohara T, Inoue K, Ogonuki N, Kanatsu-Shinohara M, Miki H, Nakata K, et al. Birth of offspring following transplantation of cryopreserved immature testicular pieces and in-vitro microinsemination. 2002;17(12):3039-45.
Jahnukainen K, Ehmcke J, Nurmio M, Schlatt SJCr. Autologous ectopic grafting of cryopreserved testicular tissue preserves the fertility of prepubescent monkeys that receive sterilizing cytotoxic therapy. 2012;72(20):5174-8.
Honaramooz A, Snedaker A, Boiani M, Schöler H, Dobrinski I, Schlatt SJN. Sperm from neonatal mammalian testes grafted in mice. 2002;418(6899):778-81.
Ohta H, Wakayama TJBor. Generation of normal progeny by intracytoplasmic sperm injection following grafting of testicular tissue from cloned mice that died postnatally. 2005;73(3):390-5.
Liu J, Cheng KM, Silversides FGJBor. Production of live offspring from testicular tissue cryopreserved by vitrification procedures in Japanese quail (Coturnix japonica). 2013;88(5):124, 1-6.
Schlatt S, Honaramooz A, Ehmcke J, Goebell P, Rübben H, Dhir R, et al. Limited survival of adult human testicular tissue as ectopic xenograft. 2006;21(2):384-9.
Wyns C, Wese F-X, Donnez J, Van Langendonckt A, Curaba MJTJoU. Long-term spermatogonial survival in cryopreserved and xenografted immature human testicular tissue editorial comment. 2009;181(5):2249.
Kuhn HE, Frontera MA, Demers LM, Bartholomew MJ, Lloyd TAJAJoDoC. The onset of sperm production in pubertal boys: relationship to gonadotropin excretion. 1989;143(2):190-3.
Chiti MC, Dolmans M-M, Donnez J, Amorim CJAobe. Fibrin in reproductive tissue engineering: a review on its application as a biomaterial for fertility preservation. 2017;45(7):1650-63.
Tian R, Yang S, Zhu Y, Zou S, Li P, Wang J, et al. VEGF/VEGFR2 signaling regulates germ cell proliferation in vitro and promotes mouse testicular regeneration in vivo. 2016;201(1):1–13.
Schmidt JA, de Avila JM, McLean DJJBor. Effect of vascular endothelial growth factor and testis tissue culture on spermatogenesis in bovine ectopic testis tissue xenografts. 2006;75(2):167-75.
Navid S, Rastegar T, Baazm M, Alizadeh R, Talebi A, Gholami K, et al. In vitro effects of melatonin on colonization of neonate mouse spermatogonial stem cells. 2017;63(6):370-81.
Gholami M, Saki G, Hemadi M, Khodadadi AJIjobms. Effect of melatonin on the expression of apoptotic genes in vitrified-thawed spermatogonia stem cells type A of 6-day-old mice. 2013;16(8):906.
Najjar M, Manzoli V, Abreu M, Villa C, Martino MM, Molano RD, et al. Fibrin gels engineered with pro‐angiogenic growth factors promote engraftment of pancreatic islets in extrahepatic sites in mice. 2015;112(9):1916-26.
Acknowledgements
The authors thank all the staff members of the Urology Research Center, especially, Zeinab Ahadi for conceiving and generating the figure.
Author information
Authors and Affiliations
Contributions
Keykavos Gholami performed the literature review and wrote the manuscript. Somayeh Solhjoo participated in the review of the literature. Seyed Mohammad Kazem Aghamir was responsible for the critical review of the manuscript.
Corresponding author
Ethics declarations
Ethics Approval
Not applicable.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Conflict of Interest
The authors declare no competing interests.
Rights and permissions
About this article
Cite this article
Gholami, K., Solhjoo, S. & Aghamir, S.M.K. Application of Tissue-Specific Extracellular Matrix in Tissue Engineering: Focus on Male Fertility Preservation. Reprod. Sci. 29, 3091–3099 (2022). https://doi.org/10.1007/s43032-021-00823-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43032-021-00823-9