Abstract
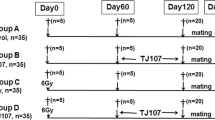
More than 40% of infertile men are diagnosed with oligoasthenozoospermia and the incidence is still rising, but the effective treatments are not been found until now. Astragalin, one of the main active ingredients in traditional Chinese medicine, may be effective in the treatment of oligoasthenozoospermia. This study investigated the pharmacological effects of astragalin for treatment of oligoasthenozoospermia in male mice, induced by cyclophosphamide (CTX). Male mice were intraperitoneally injected by CTX (50 mg/kg), and astragalin (30 mg/kg) was given via oral gavage once daily. RNA-seq analysis highlighted astragalin upregulated gene expression of anti-apoptosis (AKT1and BCL2-XL), cell proliferation (ETV1, MAPKAPK2, and RPS6KA5) and synthesis of testosterone (STAR, CYP11A1, and PRKACB), but downregulated gene expression of cell apoptosis (BAD, BCL-2, CASPASE9, and CASPASE3) in mouse testis. Astragalin also significantly reversed the reduction in body weight, reproductive organs index, and sperm parameters (sperm concentration, viability, and motility) induced by CTX, and restored testicular abnormal histopathologic morphology induced by CTX. Furthermore, astragalin dramatically rescued the gene expression related to spermatogenesis (AKT1, BCL-2, CASPASE9, CASPASE3, MAPKAPK2, RPS6KA5, STAR, and PRKACB), and increased the level of testosterone by improving related proteins (STAR, CYP11A1, PRKACB) for oligoasthenozoospermia induced by CTX. In conclusion, astragalin may be a potential beneficial agent for oligoasthenozoospermia by increasing the testosterone levels in testis.




Similar content being viewed by others
Data Availability
All the data is contained in the manuscript, raw datasets used and/or analyzed during the current study is available from the corresponding author on reasonable request.
Abbreviations
- CTX:
-
Cyclophosphamide
- BAD:
-
BCL2-associated agonist of cell death
- BCL-2:
-
B cell leukemia/lymphoma 2
- CASPASE9:
-
Cysteinyl aspartate specific proteinase 9
- CASPASE3:
-
Cysteinyl aspartate specific proteinase 3
- AKT1:
-
Thymoma viral proto-oncogene 1
- BCL2-XL:
-
BCL2-associated X protein
- ETV1:
-
ETS variant 1
- MAPKAPK2:
-
MAP kinase-activated protein kinase 2
- RPS6KA5/MSK1:
-
Ribosomal protein S6 kinase, polypeptide 5
- STAR:
-
Steroidogenic acute regulatory protein
- PRKACB:
-
Protein kinase, cAMP dependent regulatory, type II alpha
- CYP11A1:
-
Cytochrome P450, family 11, subfamily a, polypeptide 1
- LH:
-
Luteinizing hormone
- DEGs:
-
Differentially expressed genes
- GO:
-
Gene ontology
- BP:
-
Biological process
- MF:
-
Molecular function
- CC:
-
Cellular component
- KEGG:
-
Kyoto Encyclopedia of Genes and Genomes
References
Cooper T, Castilla JA (2009) WHO laboratory manual for the examination and processing of human semen. in 9th International Congress of Andrology.
Jungwirth A, et al. European Association of Urology guidelines on male infertility: the 2012 update. Eur Urol. 2012;62(2):324–32.
Chambers GM, et al. Infertility management in women and men attending primary care-patient characteristics, management actions and referrals. Hum Reprod. 2019;34(11):2173–83.
Foresta C, et al. Genetic abnormalities among severely oligospermic men who are candidates for intracytoplasmic sperm injection. J Clin Endocrinol Metab. 2005;90(1):152–6.
Saito S, et al. Astragalin from Cassia alata induces DNA adducts in vitro and repairable DNA damage in the yeast Saccharomyces cerevisiae. Int J Mol Sci. 2012;13(3):2846–62.
Kumaraswamy D, Puchchakayala G. Evaluation of anti-rheumatoid activity of cuscuta reflexa in freund’s adjuvant induced arthritic rats. Int J Phar Technol. 2016;8(2):13515–30.
Donnapee S, et al. Cuscuta chinensis Lam.: a systematic review on ethnopharmacology, phytochemistry and pharmacology of an important traditional herbal medicine. J Ethnopharmacol. 2014;157:292–308.
Walker WH. Testosterone signaling and the regulation of spermatogenesis. Spermatogenesis. 2011;1(2):116–20.
Wang Q, Zhang P, Gao HB. Luteinizing hormone induces expression of 11beta-hydroxysteroid dehydrogenase type 2 in rat Leydig cells. Reprod Biol Endocrinol. 2009;7:39.
Hu F, et al. Smad ubiquitylation regulatory factor 1 promotes LIM-homeobox gene 9 degradation and represses testosterone production in Leydig cells. Faseb j. 2018;32(9):4627–40.
Singh J, O’Neill C, Handelsman DJ. Induction of spermatogenesis by androgens in gonadotropin-deficient (hpg) mice. Endocrinology. 1995;136(12):5311–21.
Ye L, et al. Insights into the development of the adult Leydig cell lineage from stem Leydig cells. Front Physiol. 2017;8:430.
Payne AH, Hales DB. Overview of steroidogenic enzymes in the pathway from cholesterol to active steroid hormones. Endocr Rev. 2004;25(6):947–70.
Colpi GM, et al. European Academy of Andrology guideline Management of oligo-astheno-teratozoospermia. Andrology. 2018;6(4):513–24.
Egozcue S, et al. Human male infertility: chromosome anomalies, meiotic disorders, abnormal spermatozoa and recurrent abortion. Hum Reprod Update. 2000;6(1):93–105.
Ajduk A, Zernicka-Goetz M. Quality control of embryo development. Mol Aspects Med. 2013;34(5):903–18.
Zhou SH, et al. Traditional Chinese medicine as a remedy for male infertility: a review. World J Mens Health. 2019;37(2):175–85.
Yuan D, et al. Protective effects of total flavonoids from Epimedium on the male mouse reproductive system against cyclophosphamide-induced oxidative injury by up-regulating the expressions of SOD3 and GPX1. Phytother Res. 2014;28(1):88–97.
Lu WP, et al. Zn(II)-curcumin protects against oxidative stress, deleterious changes in sperm parameters and histological alterations in a male mouse model of cyclophosphamide-induced reproductive damage. Environ Toxicol Pharmacol. 2015;39(2):515–24.
Kim YH, et al. Astragalin inhibits allergic inflammation and airway thickening in ovalbumin-challenged mice. J Agric Food Chem. 2017;65(4):836–45.
Zhang W, et al. Inhibitory effects of emodin, thymol, and astragalin on leptospira interrogans-induced inflammatory response in the uterine and endometrium epithelial cells of mice. Inflammation. 2017;40(2):666–75.
Alblihed MA. Astragalin attenuates oxidative stress and acute inflammatory responses in carrageenan-induced paw edema in mice. Mol Biol Rep. 2020;47(9):6611–20.
Peng L, et al. Astragalin attenuates dextran sulfate sodium (DSS)-induced acute experimental colitis by alleviating gut microbiota dysbiosis and inhibiting NF-κB activation in mice. Front Immunol. 2020;11:2058.
Han XX, et al. Protective effects of Astragalin on spermatogenesis in streptozotocin-induced diabetes in male mice by improving antioxidant activity and inhibiting inflammation. Biomed Pharmacother. 2019;110:561–70.
Jamal M, et al. Ethanol and acetaldehyde after intraperitoneal administration to Aldh2-knockout mice-reflection in blood and brain levels. Neurochem Res. 2016;41(5):1029–34.
Yu S, et al. Chestnut polysaccharides benefit spermatogenesis through improvement in the expression of important genes. Aging (Albany NY). 2020;12(12):11431–45.
Ritchie ME, et al. limma powers differential expression analyses for RNA-sequencing and microarray studies. Nucleic Acids Res. 2015;43(7):e47.
Ashburner M, et al. Gene ontology: tool for the unification of biology. The Gene Ontology Consortium. Nat Genet. 2000;25(1):25–9.
Kanehisa M, et al. KEGG: new perspectives on genomes, pathways, diseases and drugs. Nucleic Acids Res. 2017;45(D1):D353-d361.
Yu G, et al. clusterProfiler: an R package for comparing biological themes among gene clusters. OMICS. 2012;16(5):284–7.
Wang YF, et al. Protective effects of melatonin against nicotine-induced disorder of mouse early folliculogenesis. Aging (Albany NY). 2018;10(3):463–80.
Zhang P, et al. Murine folliculogenesis in vitro is stage-specifically regulated by insulin via the Akt signaling pathway. Histochem Cell Biol. 2010;134(1):75–82.
Liu H, et al. Evaluation of decalcification techniques for rat femurs using HE and immunohistochemical staining. Biomed Res Int. 2017;2017:9050754.
Castaneda JM, et al. TCTE1 is a conserved component of the dynein regulatory complex and is required for motility and metabolism in mouse spermatozoa. Proc Natl Acad Sci U S A. 2017;114(27):E5370-e5378.
Wang Y, et al. Regulation of steroid hormones and energy status with cysteamine and its effect on spermatogenesis. Toxicol Appl Pharmacol. 2016;313:149–58.
Green DM, et al. Cumulative alkylating agent exposure and semen parameters in adult survivors of childhood cancer: a report from the St Jude Lifetime Cohort Study. Lancet Oncol. 2014;15(11):1215–23.
Choy JT, Eisenberg ML. Male infertility as a window to health. Fertil Steril. 2018;110(5):810–4.
Cheng X, Ferrell JE Jr. Apoptosis propagates through the cytoplasm as trigger waves. Science. 2018;361(6402):607–12.
Ho HJ, et al. A novel function of geranylgeraniol in regulating testosterone production. Biosci Biotechnol Biochem. 2018;82(6):956–62.
Kalkavan H, Green DR. MOMP, cell suicide as a BCL-2 family business. Cell Death Differ. 2018;25(1):46–55.
Fleisher TA (1997) Apoptosis. Ann Allergy Asthma Immunol 78(3): p. 245–9; quiz 249–50
Im YH, et al. EWS-FLI1, EWS-ERG, and EWS-ETV1 oncoproteins of Ewing tumor family all suppress transcription of transforming growth factor beta type II receptor gene. Cancer Res. 2000;60(6):1536–40.
Guo YJ, et al. ERK/MAPK signalling pathway and tumorigenesis. Exp Ther Med. 2020;19(3):1997–2007.
Sharpe RM. Intratesticular factors controlling testicular function. Biol Reprod. 1984;30(1):29–49.
Fraiser LH, Kanekal S, Kehrer JP. Cyclophosphamide toxicity. Characterising and avoiding the problem. Drugs. 1991;42(5):781–95.
Zhou Q, et al. Complete meiosis from embryonic stem cell-derived germ cells in vitro. Cell Stem Cell. 2016;18(3):330–40.
Kumar S, et al (2021) Leydig cell-specific DAX1-deleted mice has higher testosterone level in the testis during pubertal development. Reprod Sci
Afshar A, et al. Curcumin-loaded iron particle improvement of spermatogenesis in azoospermic mouse induced by long-term scrotal hyperthermia. Reprod Sci. 2021;28(2):371–80.
Tanaka T, et al. The luteinizing hormone-testosterone pathway regulates mouse spermatogonial stem cell self-renewal by suppressing WNT5A expression in Sertoli cells. Stem Cell Reports. 2016;7(2):279–91.
Baburski AZ, Andric SA, Kostic TS. Luteinizing hormone signaling is involved in synchronization of Leydig cell’s clock and is crucial for rhythm robustness of testosterone production†. Biol Reprod. 2019;100(5):1406–15.
Scott HM, et al. Role of androgens in fetal testis development and dysgenesis. Endocrinology. 2007;148(5):2027–36.
Stocco DM. StAR protein and the regulation of steroid hormone biosynthesis. Annu Rev Physiol. 2001;63:193–213.
Gonzalez E, Guengerich FP. Kinetic processivity of the two-step oxidations of progesterone and pregnenolone to androgens by human cytochrome P450 17A1. J Biol Chem. 2017;292(32):13168–85.
Lin D, et al. Role of steroidogenic acute regulatory protein in adrenal and gonadal steroidogenesis. Science. 1995;267(5205):1828–31.
Funding
This study was supported by the National Natural Science Foundation of China (No. 81960278), the Outstanding Youth Funds of Science and Technology Department of Gansu Province (No. 20JR5RA371), the Gansu Provincial Health and Family Planning Commission (GSWSKY2017-34), and the Science Foundation of the Gansu Province, China (20YF3FA030), Fundamental Research Funds for the Central Universities (No. lzujbky-2021-kd38).
Author information
Authors and Affiliations
Contributions
Xiaolei Liang, Qigang Fan, Qing Meng, and Hongli Li designed the study. Qigang Fan, Pu Gao, and Fengqin Shen performed the animal studies and finished all the experiments. Zhongying Zhao, Ruifeng He, and Meigui Zhang analyzed the data. Yi Li, Qinying Zhu, Hongli Li, and Xinlong Li prepared the draft figures and tables. Xiaolei Liang, Qigang Fan, and Qing Meng prepared the manuscript. All authors have reviewed the final manuscript.
Corresponding author
Ethics declarations
Ethics Approval and Consent to Participate
This study makes the use of male C57BL/6 N mice, and all the experimental protocol for the use of animal was approved the Ethics Committee of The First Hospital of Lanzhou University (LDYYLL2019-44).
Consent for Publication
Not applicable.
Competing Interests
The authors declare no competing interests.
Rights and permissions
About this article
Cite this article
Fan, Q., Zhao, Z., Meng, Q. et al. Improvement of Astragalin on Spermatogenesis in Oligoasthenozoospermia Mouse Induced by Cyclophosphamide. Reprod. Sci. 29, 1738–1748 (2022). https://doi.org/10.1007/s43032-021-00808-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43032-021-00808-8