Abstract
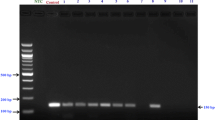
High-risk human papillomaviruses (hr-HPVs) are the key risk factors implicated in the development of a significant proportion of head and neck squamous cell carcinomas (HNSCCs). We aimed to investigate the distribution of hr-HPV types and HPV16 lineages in a sample of patients with HNSCC and the possible association between HPV status and the expression of P16INK4A and NF-κB in Iranian HNSCC patients. We examined 108 formalin-fixed, paraffin-embedded (FFPE) histologically confirmed primary SCC tissue specimens of different head and neck anatomical sites. HPV types and HPV16 lineages were determined by nested PCR and overlapping nested PCR assays, respectively, followed by gene sequencing and phylogenetic analysis. The expression of p16INK4a and NF-κB was evaluated by immunohistochemistry. Twenty-five (23.1%) HNSCC tissue specimens were tested positive for HPV infection. The most prevalent HPV type was HPV-16, followed by HPV18 and HPV11. HPV16 variants belonged to the lineage A and lineage D which were further sorted into sublineages A1, A2, and D2. A significant association between HPV status and p16INK4a immunoreactivity was observed in more than 76% of the HPV-related HNSCCs (P < 0.0001). The overexpression of p16INK4a and cytoplasmic NF-κB was more common in low-grade HNSCC tumors. Our data highlights that HPV16, in particular the A2 sublineage, followed by A1 and D2 sublineages are the major agents associated with HNSCCs in Iran. Based on HPV16 predominance and its lineage distribution pattern, it seems that the prophylactic vaccines developed for cervical cancer prevention could also be applicable for the prevention of HPV-related HNSCCs in our population.


Similar content being viewed by others
References
Wild CP, Weiderpass E, Stewart BW (2020) World cancer report: cancer research for cancer prevention. Lyon: International Agency for Research on Cancer. 2020; Chapter 5.2. ISBN 978-92-832-0448-0
Vigneswaran N, Williams MD (2014) Epidemiologic trends in head and neck cancer and aids in diagnosis. Oral Maxillofac Surg Clin North Am 26(2):123–141. https://doi.org/10.1016/j.coms.2014.01.001
Ndiaye C, Mena M, Alemany L, Arbyn M, Castellsagué X, Laporte L, Bosch FX, de Sanjosé S, Trottier H (2014) HPV DNA, E6/E7 mRNA, and p16INK4a detection in head and neck cancers: a systematic review and meta-analysis. Lancet Oncol 15(12):1319–1331. https://doi.org/10.1016/S1470-2045(14)70471-1
Spence T, Bruce J, Yip KW, Liu FF (2016) HPV associated head and neck cancer. Cancers 8(8):75. https://doi.org/10.3390/cancers8080075
Rautava J, Kuuskoski J, Syrjänen K, Grenman R, Syrjänen S (2012) HPV genotypes and their prognostic significance in head and neck squamous cell carcinomas. J Clin Virol 53(2):116–120. https://doi.org/10.1016/j.jcv.2011.11.005
Burk RD, Harari A, Chen Z (2013) Human papillomavirus genome variants. Virology 445(1–2):232–243. https://doi.org/10.1016/j.virol.2013.07.018
Freitas LB, Chen Z, Muqui EF, Boldrini NA, Miranda AE et al (2014) Human papillomavirus 16 non-European variants are preferentially associated with high-grade cervical lesions. PLoS One 9(7):e100746. https://doi.org/10.1371/journal.pone.0100746
Serrano M, Hannon GJ, Beach D (1993) A new regulatory motif in cell-cycle control causing specific inhibition of cyclin D/CDK4. Nature 366(6456):704–707. https://doi.org/10.1038/366704a0
Romagosa C, Simonetti S, Lopez-Vicente L, Mazo A, Lleonart ME et al (2011) p16 Ink4a overexpression in cancer: a tumor suppressor gene associated with senescence and high-grade tumors. Oncogene 30(18):2087–2097. https://doi.org/10.1038/onc.2010.614
Wang H, Sun R, Lin H, Hu WH (2013) P16INK4A as a surrogate biomarker for human papillomavirus-associated oropharyngeal carcinoma: consideration of some aspects. Cancer Sci 104(12):1553–1559. https://doi.org/10.1111/cas.12287
Vandermark ER, Deluca KA, Gardner CR, Marker DF, Schreiner CN, Strickland DA, Wilton KM, Mondal S, Woodworth CD (2012) Human papillomavirus type 16 E6 and E 7 proteins alter NF-kB in cultured cervical epithelial cells and inhibition of NF-kB promotes cell growth and immortalization. Virology 425(1):53–60. https://doi.org/10.1016/j.virol.2011.12.023
Anbo N, Ogi K, Sogabe Y, Shimanishi M, Kaneko T, Dehari H, Miyazaki A, Hiratsuka H (2013) Suppression of NF-κB/p65 inhibits the proliferation in oral squamous cancer cells. J Cancer Ther 4:891–897. https://doi.org/10.4236/jct.2013.44100
Monisha J, Kishor Roy N, Bordoloi D, Kumar A, Golla R, Kotoky J, Padmavathi G, B. Kunnumakkara A (2017) A. Nuclear factor kappa B: a potential target to persecute head and neck cancer. Curr Drug Targets 18(2):232–253. https://doi.org/10.2174/1389450117666160201112330
Kreimer AR, Clifford GM, Boyle P, Franceschi S (2005) Human papillomavirus types in head and neck squamous cell carcinomas worldwide: a systematic review. Cancer Epidemiol Biomark Prev 14(2):467–475. https://doi.org/10.1158/1055-9965.EPI-04-0551
Saiki RK, Bugawan TL, Horn GT, Mullis KB, Erlich HA (1986) Analysis of enzymatically amplified β-globin and HLA-DQα DNA with allele-specific oligonucleotide probes. Nature 324(6093):163–166. https://doi.org/10.1038/324163a0
Farhadi A, Behzad-Behbahani A, Geramizadeh B, Sekawi Z, Rahsaz M, Sharifzadeh S (2014) High-risk human papillomavirus infection in different histological subtypes of renal cell carcinoma. J Med Virol 86(7):1134–1144. https://doi.org/10.1002/jmv.23945
Manos MM (1989) The use of polymerase chain reaction amplification for the detection of genital human papillomavirus. Cancer Cells 7:209–214
de Roda Husman AM, Walboomers JM, van den Brule AJ, Meijer CJ, Snijders PJ (1995) The use of general primers GP5 and GP6 elongated at their 3′ ends with adjacent highly conserved sequences improves human papillomavirus detection by PCR. J Gen Virol 76(4):1057–1062. https://doi.org/10.1099/0022-1317-76-4-1057
De Boer MA, Peters LA, Aziz MF, Siregar B, Cornain S et al (2004) Human papillomavirus type 16 E6, E7, and L1 variants in cervical cancer in Indonesia, Suriname, and The Netherlands. Gynecol Oncol 94(2):488–494. https://doi.org/10.1016/j.ygyno.2004.05.037
Pientong C, Wongwarissara P, Ekalaksananan T, Swangphon P, Kleebkaow P, Kongyingyoes B, Siriaunkgul S, Tungsinmunkong K, Suthipintawong C (2013) Association of human papillomavirus type 16 long control region mutation and cervical cancer. Virol J 10(1):30. https://doi.org/10.1186/1743-422X-10-30
Tamura K, Stecher G, Peterson D, Filipski A, Kumar S (2013) MEGA6: molecular evolutionary genetics analysis version 6.0. Mol Biol Evol 30(12):2725–2729. https://doi.org/10.1093/molbev/mst197
Duncan LD, Winkler M, Carlson ER, Heidel RE, Kang E, Webb D (2013) p16 immunohistochemistry can be used to detect human papillomavirus in oral cavity squamous cell carcinoma. J Oral Maxillofac Surg 71(8):1367–1375. https://doi.org/10.1016/j.joms.2013.02.019
Zhou S, Ye W, Shao Q, Qi Y, Zhang M, Liang J (2013) Prognostic significance of XIAP and NF-κB expression in esophageal carcinoma with postoperative radiotherapy. World J Surg Oncol 11(1):288. https://doi.org/10.1186/1477-7819-11-288
Baud V, Karin M (2009) Is NF-κB a good target for cancer therapy? Hopes and pitfalls. Nat Rev Drug Discov 8(1):33–40. https://doi.org/10.1038/nrd2781
Gillison ML, Koch WM, Capone RB, Spafford M, Westra WH, Wu L, Zahurak ML, Daniel RW, Viglione M, Symer DE, Shah KV, Sidransky D (2000) Evidence for a causal association between human papillomavirus and a subset of head and neck cancers. J Natl Cancer Inst 92(9):709–720. https://doi.org/10.1093/jnci/92.9.709
Klussmann JP, Weissenborn SJ, Wieland U, Dries V, Kolligs J, Jungehuelsing M, Eckel HE, Dienes HP, Pfister HJ, Fuchs PG (2001) Prevalence, distribution, and viral load of human papillomavirus 16 DNA in tonsillar carcinomas. Cancer 92(11):2875–2884. https://doi.org/10.1002/1097-0142(20011201)92:11<2875::aid-cncr10130>3.0.co;2-7
Singhi AD, Califano J, Westra WH (2012) High-risk human papillomavirus in nasopharyngeal carcinoma. Head Neck 34(2):213–218. https://doi.org/10.1002/hed.21714
Lee LA, Huang CG, Liao CT, Lee LY, Hsueh C, Chen TC, Lin CY, Fan KH, Wang HM, Huang SF, Chen IH, Kang CJ, Ng SH, Yang SL, Tsao KC, Chang YL, Yen TC Human papillomavirus-16 infection in advanced oral cavity cancer patients is related to an increased risk of distant metastases and poor survival. PLoS One 2012;7(7). https://doi.org/10.1371/journal.pone.0040767
Duray A, Descamps G, Decaestecker C, Remmelink M, Sirtaine N, Lechien J, Ernoux-Neufcoeur P, Bletard N, Somja J, Depuydt CE, Delvenne P, Saussez S (2012) Human papillomavirus DNA strongly correlates with a poorer prognosis in oral cavity carcinoma. Laryngoscope 122(7):1558–1565. https://doi.org/10.1002/lary.23298
Götz C, Bischof C, Wolff KD, Kolk A (2019) Detection of HPV infection in head and neck cancers: promise and pitfalls in the last ten years: a meta-analysis. Mol Clin Oncol 10(1):17–28. https://doi.org/10.3892/mco.2018.1749
Termine N, Panzarella V, Falaschini S, Russo A, Matranga D, Lo Muzio L, Campisi G (2008) HPV in oral squamous cell carcinoma vs head and neck squamous cell carcinoma biopsies: a meta-analysis (1988–2007). Ann Oncol 19(10):1681–1690. https://doi.org/10.1093/annonc/mdn372
Guo L, Yang F, Yin Y, Liu S, Li P, Zhang X, Chen D, Liu Y, Wang J, Wang K, Zhu Y, Lv Q, Wang X, Sun X (2018) Prevalence of human papillomavirus type-16 in head and neck cancer among the Chinese population: a meta-analysis. Front Oncol 8:619. https://doi.org/10.3389/fonc.2018.00619
Jalilvand S, Shoja Z, Hamkar R (2014) Human papillomavirus burden in different cancers in Iran: a systematic assessment. Asian Pac J Cancer Prev 15(17):7029–7035. https://doi.org/10.7314/apjcp.2014.15.17.7029
Kingma DW, Allen RA, Moore W, Caughron SK, Melby M, Gillies EM, Marlar RA, Dunn ST (2010) HPV genotype distribution in oral and oropharyngeal squamous cell carcinoma using seven in vitro amplification assays. Anticancer Res 30(12):5099–5104
Nauta IH, Rietbergen MM, van Bokhoven AA, Bloemena E, Lissenberg-Witte BI et al (2018) Evaluation of the eighth TNM classification on p16-positive oropharyngeal squamous cell carcinomas in the Netherlands and the importance of additional HPV DNA testing. Ann Oncol 29(5):1273–1279. https://doi.org/10.1093/annonc/mdy060
Ni G, Huang K, Luan Y, Cao Z, Chen S, Ma B, Yuan J, Wu X, Chen G, Wang T, Li H, Walton S, Liu F, Chen B, Wang Y, Pan X, Liu X, Frazer IH (2019) Human papillomavirus infection among head and neck squamous cell carcinomas in southern China. PLoS One 14(9). https://doi.org/10.1371/journal.pone.0221045
Michaud DS, Langevin SM, Eliot M, Nelson HH, Pawlita M, McClean MD, Kelsey KT (2014) High-risk HPV types and head and neck cancer. Int J Cancer 135(7):1653–1661. https://doi.org/10.1002/ijc.28811
Mineta H, Ogino T, Amano HM, Ohkawa Y, Araki K, Takebayashi S, Miura K (1998) Human papilloma virus (HPV) type 16 and 18 detected in head and neck squamous cell carcinoma. Anticancer Res 18(6B):4765–4768
Syrjänen S (2010) The role of human papillomavirus infection in head and neck cancers. Ann Oncol 21(suppl_7):vii243–vii245. https://doi.org/10.1093/annonc/mdq454
D’Souza G, Westra WH, Wang SJ, Van Zante A, Wentz A et al (2017) Differences in the prevalence of human papillomavirus (HPV) in head and neck squamous cell cancers by sex, race, anatomic tumor site, and HPV detection method. JAMA Oncol 3(2):169–177. https://doi.org/10.1001/jamaoncol.2016.3067
Chaturvedi AK, Engels EA, Pfeiffer RM, Hernandez BY, Xiao W, Kim E, Jiang B, Goodman MT, Sibug-Saber M, Cozen W, Liu L, Lynch CF, Wentzensen N, Jordan RC, Altekruse S, Anderson WF, Rosenberg PS, Gillison ML (2011) Human papillomavirus and rising oropharyngeal cancer incidence in the United States. J Clin Oncol 29(32):4294–4301. https://doi.org/10.1200/JCO.2011.36.4596
Field N, Lechner M (2015) Exploring the implications of HPV infection for head and neck cancer. Sex Transm Dis 91:229–230. https://doi.org/10.1136/sextrans-2014-051808
Yamada T, Wheeler CM, Halpern AL, Stewart AC, Hildesheim A, Jenison SA (1995) Human papillomavirus type 16 variant lineages in United States populations characterized by nucleotide sequence analysis of the E6, L2, and L1 coding segments. J Virol 69(12):7743–7753
Vaezi T, Shoja Z, Hamkar R, Shahmahmoodi S, Nozarian Z, Marashi SM, Jalilvand S (2017) Human papillomavirus type 16 lineage analysis based on E6 region in cervical samples of Iranian women. Infect Genet Evol 55:26–30. https://doi.org/10.1016/j.meegid.2017.08.025
Schiffman M, Rodriguez AC, Chen Z, Wacholder S, Herrero R, Hildesheim A, Desalle R, Befano B, Yu K, Safaeian M, Sherman ME, Morales J, Guillen D, Alfaro M, Hutchinson M, Solomon D, Castle PE, Burk RD (2010) A population-based prospective study of carcinogenic human papillomavirus variant lineages, viral persistence, and cervical neoplasia. Cancer Res 70(8):3159–3169. https://doi.org/10.1158/0008-5472.CAN-09-4179
Zuna RE, Moore WE, Shanesmith RP, Dunn ST, Wang SS, Schiffman M, Blakey GL, Teel T (2009) Association of HPV16 E6 variants with diagnostic severity in cervical cytology samples of 354 women in a US population. Int J Cancer 125(11):2609–2613. https://doi.org/10.1002/ijc.24706
Nicolás-Párraga S, Alemany L, De Sanjosé S, Bosch FX, Bravo IG et al (2017) Differential HPV16 variant distribution in squamous cell carcinoma, adenocarcinoma and adenosquamous cell carcinoma. Int J Cancer 140(9):2092–2100. https://doi.org/10.1002/ijc.30636
Mirabello L, Yeager M, Cullen M, Boland JF, Chen Z et al (2016) HPV16 sublineage associations with histology-specific cancer risk using HPV whole-genome sequences in 3200 women. J Natl Cancer Inst 108(9):djw100. https://doi.org/10.1093/jnci/djw100
Rietbergen MM, Snijders PJ, Beekzada D, Braakhuis BJ, Brink A et al (2014) Molecular characterization of p16-immunopositive but HPV DNA-negative oropharyngeal carcinomas. Int J Cancer 134(10):2366–2372. https://doi.org/10.1002/ijc.28580
Gheit T, Anantharaman D, Holzinger D, Alemany L, Tous S, Lucas E, Prabhu PR, Pawlita M, Ridder R, Rehm S, Bogers J, Maffini F, Chiocca S, Lloveras B, Kumar RV, Somanathan T, de Sanjosé S, Castellsagué X, Arbyn M, Brennan P, Sankaranarayanan R, Pillai MR, Gangane N, Tommasino M, the HPV-AHEAD study group (2017) Role of mucosal high-risk human papillomavirus types in head and neck cancers in central India. Int J Cancer 141(1):143–151. https://doi.org/10.1002/ijc.30712
Castellsagué X, Alemany L, Quer M, Halec G, Quirós B et al (2016) HPV involvement in head and neck cancers: comprehensive assessment of biomarkers in 3680 patients. J Natl Cancer Inst 108(6):djv403. https://doi.org/10.1093/jnci/djv403
Porceddu SV, Milne R, Brown E, Bernard A, Rahbari R, Cartmill B, Foote M, McGrath M, Coward J, Panizza B (2017) Validation of the ICON-S staging for HPV-associated oropharyngeal carcinoma using a pre-defined treatment policy. Oral Oncol 66:81–86. https://doi.org/10.1016/j.oraloncology.2017.01.002
Yan M, Xu Q, Zhang P, Zhou XJ, Zhang ZY, Chen WT (2010) Correlation of NF-κB signal pathway with tumor metastasis of human head and neck squamous cell carcinoma. BMC Cancer 10(1):437. https://doi.org/10.1186/1471-2407-10-437
Sawhney M, Rohatgi N, Kaur J, Shishodia S, Sethi G, Gupta SD, Deo SVS, Shukla NK, Aggarwal BB, Ralhan R (2007) Expression of NF-kappaB parallels COX-2 expression in oral precancer and cancer: association with smokeless tobacco. Int J Cancer 120:2545–2556. https://doi.org/10.1002/ijc.22657
Kamperos G, Nikitakis N, Sfakianou A, Avgoustidis D, Sklavounou-Andrikopoulou A (2016) Expression of NF-κB and IL-6 in oral precancerous and cancerous lesions: an immunohistochemical study. Medicina Oral Patologia Oral y Cirugia Bucal 21(1):e6. https://doi.org/10.4317/medoral.20570
Nakahara T, Tanaka K, Ohno SI, Egawa N, Yugawa T, Kiyono T (2015) Activation of NF-κB by human papillomavirus 16 E1 limits E1-dependent viral replication through degradation of E1. J Virol 89(9):5040–5059. https://doi.org/10.1128/JVI.00389-15
Li J, Jia H, Xie L, Wang X, Wang X, He H, Lin Y, Hu L (2009) Association of constitutive nuclear factor-κB activation with aggressive aspects and poor prognosis in cervical cancer. Int J Gynecol Cancer 19(8):1421–1426. https://doi.org/10.1111/IGC.0b013e3181b70445
Du J, Chen GG, Vlantis AC, Xu H, Tsang RK et al (2003) The nuclear localization of NFκB and p53 is positively correlated with HPV16 E7 level in laryngeal squamous cell carcinoma. J Histochem Cytochem 51(4):533–539. https://doi.org/10.1177/002215540305100415
Gupta S, Kumar P, Kaur H, Sharma N, Gupta S et al (2018) Constitutive activation and overexpression of NF-κB/c-Rel in conjunction with p50 contribute to aggressive tongue tumorigenesis. Oncotarget 9(68):33011. https://doi.org/10.18632/oncotarget.26041
Senba M, Mori N, Fujita S, Jutavijittum P, Yousukh A et al (2010) Relationship among human papillomavirus infection, p16INK4a, p53 and NF-κB activation in penile cancer from northern Thailand. Oncol Lett 1(4):599–603. https://doi.org/10.3892/ol_00000106
Hajek M, Sewell A, Kaech S, Burtness B, Yarbrough WG, Issaeva N (2017) TRAF3/CYLD mutations identify a distinct subset of human papillomavirus associated head and neck squamous cell carcinoma. Cancer 123:1778–1790. https://doi.org/10.1002/cncr.30570
Pan C, Issaeva N, Yarbrough WG (2018) HPV-driven oropharyngeal cancer: current knowledge of molecular biology and mechanisms of carcinogenesis. Cancers Head Neck 3(1):12. https://doi.org/10.1186/s41199-018-0039-3
Acknowledgments
The authors would like to thank the staff of the Diagnostic Laboratory Sciences and Technology Research Center (DLSTRC) and Oral & Maxillofacial Pathology Laboratory, school of Dentistry, Shiraz University of Medical Sciences, Shiraz, Iran.
Funding
This study was supported by a grant from Shiraz University of Medical Sciences, Shiraz, Iran, under the agreement no. 93-01-45-8241.
Author information
Authors and Affiliations
Contributions
Writing—original draft preparation, methodology, and investigation: F.P. Conceptualization, methodology, writing review and editing, supervision, and visualization: A.F. Methodology and validation: T.P. Methodology and investigation: A.A.T. Project administration, software, and formal analysis: P.A. Resources and methodology: A.B.B. and M.J.A. All the authors provided a critical revision of this manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethical statement
The Ethical Committee of Shiraz University of Medical Sciences approved this study (SUMS, ethical reference No. IR.SUMS.REC.1393.8241) given the retrospective nature of the study.
Additional information
Responsible Editor: Flavio Guimaraes Fonseca.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Pakdel, F., Farhadi, A., Pakdel, T. et al. The frequency of high-risk human papillomavirus types, HPV16 lineages, and their relationship with p16INK4a and NF-κB expression in head and neck squamous cell carcinomas in Southwestern Iran. Braz J Microbiol 52, 195–206 (2021). https://doi.org/10.1007/s42770-020-00391-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s42770-020-00391-1