Abstract
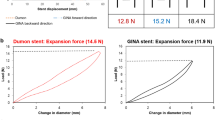
Tracheal stents are an important form of treatment for benign or malignant central airway obstruction. However, the mechanical behavior of current tracheal stents is significantly different from that of the native trachea, which leads to a variety of serious complications. In this study, inspired by the structure of the native trachea, a wavy non-uniform ligament chiral tracheal stent is proposed, in which J-shaped stress–strain behavior and negative Poisson's ratio response are achieved by replacing the tangential ligament of tetrachiral and anti-tetrachiral hybrid structure with a wavy non-uniform ligament. Through the combination of theoretical analysis, finite element analysis and experimental tests, a wide range of desired J-shaped stress–strain curves are explored to mimic the native porcine trachea by tailoring the stent geometry. Besides, the negative Poisson’s ratio and auxetic diameter curves versus axial strain of the stent are also studied in detail, thus contributing to the enhancement of cross-section ventilation and reducing the migration of the stent. This novel tracheal stent with a unique microstructure shows a potential to perfectly match the physiological activities of the native trachea and thereby reduce potential complications.
Graphic abstract







Similar content being viewed by others
References
Murgu SD, Egressy K, Laxmanan B et al (2016) Central airway obstruction benign strictures, tracheobronchomalacia, and malignancy-related obstruction. Chest 150(2):426–441. https://doi.org/10.1016/j.chest.2016.02.001
Milian RD, Foley E, Bauer M et al (2019) Expiratory central airway collapse in adults: corrective treatment (part 2). J Cardiothorac Vasc Anesth 33(9):2555–2560. https://doi.org/10.1053/j.jvca.2018.09.009
Avasarala SK, Freitag L, Mehta AC (2019) Metallic endobronchial stents a contemporary resurrection. Chest 155(6):1246–1259. https://doi.org/10.1016/j.chest.2018.12.001
Guibert N, Saka H, Dutau H (2020) Airway stenting: technological advancements and its role in interventional pulmonology. Respirology 25(9):953–962. https://doi.org/10.1111/resp.13801
Kamel KS, Beckert LE, Stringer MD (2009) Novel insights into the elastic and muscular components of the human trachea. Clin Anat 22(6):689–697. https://doi.org/10.1002/ca.20841
Boazak EM, Auguste DT (2018) Trachea mechanics for tissue engineering design. Acs Biomater Sci Eng 4(4):1272–1284. https://doi.org/10.1021/acsbiomaterials.7b00738
Baiguera S, Del Gaudio C, Jaus MO et al (2012) Long-term changes to in vitro preserved bioengineered human trachea and their implications for decellularized tissues. Biomaterials 33(14):3662–3672. https://doi.org/10.1016/j.biomaterials.2012.01.064
Guimaraes CF, Gasperini L, Marques AP et al (2020) The stiffness of living tissues and its implications for tissue engineering. Nat Rev Mater 5(5):351–370. https://doi.org/10.1038/s41578-019-0169-1
Wong VW, Paterno J, Sorkin M et al (2011) Mechanical force prolongs acute inflammation via T-cell-dependent pathways during scar formation. FASEB J 25(12):4498–4510. https://doi.org/10.1096/fj.10-178087
Karush JM, Seder CW, Raman A et al (2017) Durability of silicone airway stents in the management of benign central airway obstruction. Lung 195(5):601–606. https://doi.org/10.1007/s00408-017-0023-4
Wu XD, Zhang X, Zhang W et al (2019) Long-term outcome of metallic stenting for central airway involvement in relapsing polychondritis. Ann Thorac Surg 108(3):897–904. https://doi.org/10.1016/j.athoracsur.2019.02.039
Yang W, Sherman VR, Gludovatz B et al (2015) On the tear resistance of skin. Nat Commun 6:10. https://doi.org/10.1038/ncomms7649
Kwansa AL, Empson YM, Ekwueme EC et al (2010) Novel matrix based anterior cruciate ligament (ACL) regeneration. Soft Matter 6(20):5016–5025. https://doi.org/10.1039/c0sm00182a
Chamiot-Clerc P, Copie X, Renaud JF et al (1998) Comparative reactivity and mechanical properties of human isolated internal mammary and radial arteries. Cardiovasc Res 37(3):811–819. https://doi.org/10.1016/s0008-6363(97)00267-8
Meyers AD, Bishop HE, Peters S (1980) Biomechanical characteristscs of the human trchea. Otolaryngology-Head Neck Surg 88(4):409–411. https://doi.org/10.1177/019459988008800416
Lomeli-Mejia PA, Cruz-Orea A, Araujo-Monsalvo VM et al (2020) Evaluation of tensile force in a porcine trachea using a reflective optical method. J Spectroscopy 2020:7816969. https://doi.org/10.1155/2020/7816969
Yan DJ, Chang JH, Zhang H et al (2020) Soft three-dimensional network materials with rational bio-mimetic designs. Nat Commun 11(1):11. https://doi.org/10.1038/s41467-020-14996-5
Ma YJ, Feng X, Rogers JA et al (2017) Design and application of ‘J-shaped’ stress-strain behavior in stretchable electronics: a review. Lab Chip 17(10):1689–1704. https://doi.org/10.1039/c7lc00289k
Ma Q, Cheng H, Jang KI et al (2016) A nonlinear mechanics model of bio-inspired hierarchical lattice materials consisting of horseshoe microstructures. J Mech Phys Solids 90:179–202. https://doi.org/10.1016/j.jmps.2016.02.012
Yan ZG, Wang BL, Wang KF et al (2019) A novel cellular substrate for flexible electronics with negative Poisson ratios under large stretching. Int J Mech Sci 151:314–321. https://doi.org/10.1016/j.ijmecsci.2018.11.026
Zhalmuratova D, La TG, Yu KTT et al (2019) Mimicking “J-Shaped” and anisotropic stress-strain behavior of human and porcine aorta by fabric-reinforced elastomer composites. ACS Appl Mater Interf 11(36):33323–33335. https://doi.org/10.1021/acsami.9b10524
Ray TR, Choi J, Bandodkar AJ et al (2019) Bio-integrated wearable systems: a comprehensive review. Chem Rev 119(8):5461–5533. https://doi.org/10.1021/acs.chemrev.8b00573
Ma YJ, Zhang YC, Cai SS et al (2020) Flexible hybrid electronics for digital healthcare. Adv Mater 32(15):23. https://doi.org/10.1002/adma.201902062
Lei M, Hong W, Zhao Z et al (2019) 3D printing of auxetic metamaterials with digitally reprogrammable shape. ACS Appl Mater Interf 11(25):22768–22776. https://doi.org/10.1021/acsami.9b06081
Xin X, Liu L, Liu Y et al (2020) 4D printing auxetic metamaterials with tunable, programmable, and reconfigurable mechanical properties. Adv Funct Mater 30(43):2004226. https://doi.org/10.1002/adfm.202004226
Wu WW, Hu WX, Qian GA et al (2019) Mechanical design and multifunctional applications of chiral mechanical metamaterials: a review. Mater Des 180:13. https://doi.org/10.1016/j.matdes.2019.107950
Wang ZW, Luan CC, Liao GX et al (2020) Progress in auxetic mechanical metamaterials: structures, characteristics, manufacturing methods, and applications. Adv Eng Mater 22(10):23. https://doi.org/10.1002/adem.202000312
Yu HB, Wu WW, Zhang JX et al (2019) Drastic tailorable thermal expansion chiral planar and cylindrical shell structures explored with finite element simulation. Compos Struct 210:327–338. https://doi.org/10.1016/j.compstruct.2018.11.043
Ruan X, Yuan W, Hu Y et al (2020) Chiral constrained stent: effect of structural design on the mechanical and intravascular stent deployment performances. Mech Mater 148:103509. https://doi.org/10.1016/j.mechmat.2020.103509
Farrugia PS, Gatt R, Grima-Cornish JN et al (2020) Tuning the mechanical properties of the anti-tetrachiral system using nonuniform ligament thickness. Phys Status Solidi B-Basic Solid State Phys 257(10):1900507. https://doi.org/10.1002/pssb.201900507
Liu J, Yao X, Wang Z et al (2021) A flexible porous chiral auxetic tracheal stent with ciliated epithelium. Acta Biomater 124:153–165. https://doi.org/10.1016/j.actbio.2021.01.044
Geng LC, Ruan XL, Wu WW et al (2019) Mechanical properties of selective laser sintering (SLS) additive manufactured chiral auxetic cylindrical stent. Exp Mech 59(6):913–925. https://doi.org/10.1007/s11340-019-00489-0
Liu J, Yan D, Zhang Y (2021) Mechanics of unusual soft network materials with rotatable structural nodes. J Mech Phys Solids 146:104210. https://doi.org/10.1016/j.jmps.2020.104210
Tufekci E, Ozdemirci O (2006) Exact solution of free in-plane vibration of a stepped circular arch. J Sound Vib 295(3–5):725–738. https://doi.org/10.1016/j.jsv.2006.01.048
Fan Z, Zhang Y, Ma Q et al (2016) A finite deformation model of planar serpentine interconnects for stretchable electronics. Int J Solids Struct 91:46–54. https://doi.org/10.1016/j.ijsolstr.2016.04.030
Babu AR, Gundiah N (2014) Role of crosslinking and entanglements in the mechanics of silicone networks. Exp Mech 54(7):1177–1187. https://doi.org/10.1007/s11340-014-9895-x
Nooni AR, Aslan TA, Temel B (2018) An efficient approach for in-plane free and forced vibrations of axially functionally graded parabolic arches with nonuniform cross section. Compos Struct 200:701–710. https://doi.org/10.1016/j.compstruct.2018.05.077
Greaves GN, Greer AL, Lakes RS et al (2011) Poisson’s ratio and modern materials. Nat Mater 10(11):823–837. https://doi.org/10.1038/nmat3134
Wang D, Xiong Y, Zhang B et al (2020) Design framework for mechanically tunable soft biomaterial composites enhanced by modified horseshoe lattice structures. Soft Matter 16(6):1473–1484. https://doi.org/10.1039/c9sm02119a
Hoffman B, Martin M, Brown BN et al (2016) Biomechanical and biochemical characterization of porcine tracheal cartilage. Laryngoscope 126(10):E325–E331. https://doi.org/10.1002/lary.25861
Xue ZG, Song HL, Rogers JA et al (2020) Mechanically-guided structural designs in stretchable inorganic electronics. Adv Mater 32(15):32. https://doi.org/10.1002/adma.201902254
Zhu YZ, Joralmon D, Shan WT et al (2021) 3D printing biomimetic materials and structures for biomedical applications. Bio-Des Manuf 4(2):405–428. https://doi.org/10.1007/s42242-020-00117-0
Safshekan F, Tafazzoli-Shadpour M, Abdouss M et al (2020) Finite element simulation of human trachea: normal vs. surgically treated and scaffold implanted cases. Int J Solids Struct 190:35–46. https://doi.org/10.1016/j.ijsolstr.2019.10.021
Wang YE, Guo Y, Wei QH et al (2021) Current researches on design and manufacture of biopolymer-based osteochondral biomimetic scaffolds. Bio-Des Manuf 4(3):541–567. https://doi.org/10.1007/s42242-020-00119-y
Ahn CB, Son KH, Yu YS et al (2019) Development of a flexible 3D printed scaffold with a cell-adhesive surface for artificial trachea. Biomed Mater 14(5):9. https://doi.org/10.1088/1748-605X/ab2a6c
She YL, Fan ZW, Wang L et al (2021) 3D printed biomimetic pcl scaffold as framework interspersed with collagen for long segment tracheal replacement. Front Cell Dev Biol 9:14. https://doi.org/10.3389/fcell.2021.629796
Askari M, Hutchins DA, Thomas PJ et al (2020) Additive manufacturing of metamaterials: A review. Addit Manuf 36:101562. https://doi.org/10.1016/j.addma.2020.101562
Lin M, Firoozi N, Tsai CT et al (2019) 3D-printed flexible polymer stents for potential applications in inoperable esophageal malignancies. Acta Biomater 83:119–129. https://doi.org/10.1016/j.actbio.2018.10.035
Hamzehei R, Rezaei S, Kadkhodapour J et al (2020) 2D triangular anti-trichiral structures and auxetic stents with symmetric shrinkage behavior and high energy absorption. Mech Mater 142:10. https://doi.org/10.1016/j.mechmat.2019.103291
Acknowledgements
This article was supported by the National Key Research and Development Program of China (No. 2020YFC1107103), the National Natural Science Foundation of China (No. 51821093), and the Research Project of Public Welfare Technology Application of Zhejiang Province, China (No. LGF21H010006).
Author information
Authors and Affiliations
Contributions
JPL contributed to conceptualization, formal analysis, data curation, investigation, methodology, visualization and writing—original draft; XHY and JY contributed to conceptualization, supervision, validation, and writing—review & editing; ZWW and CCL helped in formal analysis and methodology; JZF and YH helped in resources, supervision, validation and project administration.
Corresponding authors
Ethics declarations
Conflict of interest
All authors declare that there is no financial or commercial conflict of interest.
Ethical approval
This article does not contain any studies with human or animal subjects performed by any of the authors.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file1 (MP4 12897 KB)
Rights and permissions
About this article
Cite this article
Liu, J., Yao, X., Wang, Z. et al. A novel wavy non-uniform ligament chiral stent with J-shaped stress–strain behavior to mimic the native trachea. Bio-des. Manuf. 4, 851–866 (2021). https://doi.org/10.1007/s42242-021-00159-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s42242-021-00159-y