Abstract
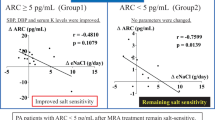
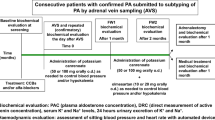
Mild hyperkalemia is a common side effect of mineralocorticoid receptor antagonist (MRA) treatment of patients with primary aldosteronism (PA), which can be worsened by instructions to minimize salt intake. Our objective was to evaluate the effect of salt consumption on serum potassium levels and mean, mean minimal, and mean maximal systolic and diastolic blood pressure (BP) in MRA-treated hyperkalemic PA patients under relative salt restriction. Seventeen consecutive mildly hyperkalemic MRA-treated PA patients aged 66.3 ± 8.37 years were recruited. Body mass index (BMI) and BP were assessed, and serum and 24-h urinary sodium and potassium levels, plasma renin, and serum aldosterone were measured, while patients followed a relatively salt-restricted diet, after 1 month of controlled salt supplementation (usual salt-restricted diet plus 4 g salt/day) and after 6 months on instructions for free dietary salt consumption. Baseline salt consumption was additionally evaluated in two more patient groups (normotensive subjects and normokalemic MRA-treated PA patients). One month of controlled salt supplementation (24-h urine sodium (median, min, max): 195.2 (120.30–275.20) vs 110.13 (34.30–139.20) mEq/day, p < 0.001) resulted in increased kaliuresis (62.25 (40.69–97.0) vs 54.0 (23.28–79.60) mEq/day, p = 0.001) and a decrease of serum potassium (5.2 (5–5.70) vs 4.6 (3.8–5.1) mEq/L, p < 0.001), while serum sodium (139 (133–141) vs 1 39 (135–144) mEq/L) and mean systolic (130 (105–141 vs. 130 (106–141) mmHg) and diastolic (76 (53–85) vs75 (53–84) mmHg) BP remained stable. These findings were unchanged after 6 months of free salt consumption. BMI remained constant, while plasma renin and serum aldosterone decreased following salt repletion. Adequate salt consumption attenuates MRA-induced hyperkalemia in relatively salt-restricted PA patients without affecting BP or BMI.



Similar content being viewed by others
References
Rossi GP, Bernini G, Caliumi C, Desideri G, Fabris B, Ferri C, Ganzaroli C, Giacchetti G, Letizia C, Maccario M, Mallamaci F, Mannelli M, Mattarello MJ, Moretti A, Palumbo G, Parenti G, Porteri E, Semplicini A, Rizzoni D, Rossi E, Boscaro M, Pessina AC, Mantero F, PAPY Study Investigators (2006) A prospective study of the prevalence of primary aldosteronism in 1,125 hypertensive patients. J Am Coll Cardiol 48(11):2293–2300
Markou A, Sertedaki A, Kaltsas G, Androulakis II, Marakaki C, Pappa T, Gouli A, Papanastasiou L, Fountoulakis S, Zacharoulis A, Karavidas A, Ragkou D, Charmandari E, Chrousos GP, Piaditis GP (2015) Stress-induced aldosterone hyper-secretion in a substantial subset of patients with essential hypertension. J Clin Endocrinol Metab 100(8):2857–2864. https://doi.org/10.1210/jc.2015-1268
Papanastasiou L, Markou A, Pappa T, Gouli A, Tsounas P, Fountoulakis S, Kounadi T, Tsiama V, Dasou A, Gryparis A, Samara C, Zografos G, Kaltsas G, Chrousos G, Piaditis G (2014) Primary aldosteronism in hypertensive patients: clinical implications and target therapy. Eur J Clin Investig 44(8):697–706. https://doi.org/10.1111/eci.12286
Milliez P, Girerd X, Plouin PF, Blacher J, Safar ME, Mourad JJ (2005) Evidence for an increased rate of cardiovascular events in patients with primary aldosteronism. J Am Coll Cardiology 45(8):1243–1248. https://doi.org/10.1016/j.jacc.2005.01.015
Monticone S, D’Ascenzo F, Moretti C, Williams TA, Veglio F, Gaita F, Mulatero P (2018) Cardiovascular events and target organ damage in primary aldosteronism compared with essential hypertension: a systematic review and meta-analysis. Lancet Diabetes Endocrinol 6(1):41–50. https://doi.org/10.1016/S2213-8587(17)30319-4
Lim PO, Jung RT, MacDonald TM (1999) Raised aldosterone to renin ratio predicts antihypertensive efficacy of spironolactone: a prospective cohort follow-up study. Br J ClinPharmacol 48(5):756–760
Parthasarathy HK, Menard J, White WB, Young WF, Jr., Williams GH, Williams B, Ruilope LM, McInnes GT, Connell JM, MacDonald TM. A (2011) A double-blind, randomized study comparing the antihypertensive effect of eplerenone and spironolactone in patients with hypertension and evidence of primary aldosteronism. J Hypertens 29(5):980–990. https://doi.org/10.1097/HJH.0b013e3283455ca5
Funder JW (2013) Primary aldosteronism and low renin hypertension: a continuum? Nephrol Dial Transplant 28(7):1625–1627. https://doi.org/10.1093/ndt/gft052
Karagiannis A, Tziomalos K, Papageorgiou A, Kakafika AI, Pagourelias ED, Anagnostis P, Athyros VG, Mikhailidis DP (2008) Spironolactone versus eplerenone for the treatment of idiopathic hyperaldosteronism. Expert OpinPharmacother9(4):509–515. https://doi.org/10.1517/14656566.9.4.509
Wada N, Shibayama Y, Umakoshi H, Ichijo T, Fujii Y, Kamemura K, Kai T, Sakamoto R, Ogo A, Matsuda Y, Fukuoka T, Tsuiki M, Suzuki T, Naruse M (2017) Hyperkalemia in both surgically and medically treated patients with primary aldosteronism. J Hum Hypertens 31(10):627–632. https://doi.org/10.1038/jhh.2017.38
Desai A (2008) Hyperkalemia associated with inhibitors of the renin-angiotensin-aldosterone system: balancing risk and benefit. Circulation 118(16):1609–1611. https://doi.org/10.1161/CIRCULATIONAHA.108.807917
Williams JS, Williams GH, Raji A, Jeunemaitre X, Brown NJ, Hopkins PN, Conlin PR (2006) Prevalence of primary hyperaldosteronism in mild to moderate hypertension without hypokalaemia. J Hum Hypertens 20(2):129–136. https://doi.org/10.1038/sj.jhh.1001948
Christensen BM, Perrier R, Wang Q, Zuber AM, Maillard M, Mordasini D, Malsure S, Ronzaud C, StehleJC RBC, Hummler E (2010) Sodium and potassium balance depends on αENaC expression in connecting tubule. J Am Soc Nephrol 21(11):1942–1951. https://doi.org/10.1681/ASN.2009101077
Perrier R, Boscardin E, Malsure S, Sergi C, Maillard MP, Loffing J, Loffing-Cueni D, Sørensen MV, Koesters R, Rossier BC, Frateschi S, Hummler E (2016) Severe salt-losing syndrome and hyperkalemia induced by adult nephron-specific knockout of the epithelial sodium channel α-subunit. J Am Soc Nephrol 27(8):2309–2318. https://doi.org/10.1681/ASN.2015020154
Markou A, Pappa T, Kaltsas G, Gouli A, Mitsakis K, Tsounas P, Prevoli A, Tsiavos V, Papanastasiou L, Zografos G, Chrousos GP, Piaditis GP (2013) Evidence of primary aldosteronism in a predominantly female cohort of normotensive individuals: a very high odds ratio for progression into arterial hypertension. J Clin Endocrinol Metab 98(4):1409–1416. https://doi.org/10.1210/jc.2012-3353
Eckel RH, JakicicJM AJD, de Jesus JM, Houston Miller N, Hubbard VS, Lee IM, Lichtenstein AH, Loria CM, Millen BE, Nonas CA, Sacks FM, Smith SC Jr, Svetkey LP, Wadden TA, Yanovski SZ, Kendall KA, Morgan LC, Trisolini MG, Velasco G, Wnek J, Anderson JL, Halperin JL, Albert NM, Bozkurt B, Brindis RG, Curtis LH, DeMets D, Hochman JS, Kovacs RJ, Ohman EM, Pressler SJ, Sellke FW, Shen WK, Smith SC Jr, Tomaselli GF (2014) American College of Cardiology/American Heart Association Task Force on Practice Guidelines.2013 AHA/ACC guideline on lifestyle management to reduce cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines. Circulation 129(25 Suppl 2):S76–S99. https://doi.org/10.1161/01.cir.0000437740.48606.d1
Dolci A, Panteghini M (2014) Harmonization of automated hemolysis index assessment and use: is it possible? Clin Chim Acta 432:38–43. https://doi.org/10.1016/j.cca.2013.10.012
Vasara E, Marakis G, Breda J, Skepastianos P, Hassapidou M, Kafatos A, Rodopaios N, Koulouri AA, Cappuccio FP (2017) Sodium and potassium intake in healthy adults in Thessaloniki Greater Metropolitan Area-The Salt Intake in Northern Greece (SING) Study. Nutrients 9(4):E417. https://doi.org/10.3390/nu9040417
Maiolino G, Rossitto G, Bisogni V, Cesari M, Seccia TM, Plebani M, Rossi GP, PAPY Study Investigators (2017) Quantitative Value of aldosterone-renin ratio for detection of aldosterone-producing adenoma: the Aldosterone-Renin Ratio for Primary Aldosteronism (AQUARR) Study. J Am Heart Assoc 6(5):e005574. https://doi.org/10.1161/JAHA.117.005574
Ori Y, Chagnac A, Korzets A, Zingerman B, Herman-Edelstein M, Bergman M, Gafter U, Salman H (2013) Regression of left ventricular hypertrophy in patients with primary aldosteronism/low hypertension on low dose spironolactone. Nephrol Dial Transplant 28(7):1787–1793. https://doi.org/10.1093/ndt/gfs587
Bansal S, Lindenfeld J, Schrier RW (2009) Sodium retention in heart failure and cirrhosis: potential role of natriuretic doses of mineralocorticoid antagonist? Circ Heart Fail 2(4):370–376. https://doi.org/10.1161/CIRCHEARTFAILURE.108.821199
Hundemer GL, Curhan GC, Yozamp N, Wang M, Vaidya A (2017) Cardiometabolic outcomes and mortality in medically treated primary aldosteronism: a retrospective cohort study. Lancet Diabetes Endrocrinol 6(1):51–59. https://doi.org/10.1016/S2213-8587(17)30367-4
Weir MR, Rolfe M (2010) Potassium homeostasis and renin-angiotensin-aldosterone system inhibitors. Clin J Am SocNephrol 5(3):531–548. https://doi.org/10.2215/CJN.07821109
Juurlink DN, Mamdani MM, Lee DS, Kopp A, Austin PC, Laupacis A, Redelmeier DA (2004) Rates of hyperkalemia after publication of the randomized aldactone evaluation study. N Engl J Med 351(6):543–551
Vardeny O, Claggett B, Anand I, Rossignol P, Desai AS, Zannad F, Pitt B, Solomon SD (2014) Randomized Aldactone evaluation study (RALES) investigators. Incidence, predictors, and outcomes related to hypo- and hyperkalemia in patients with severe heart failure treated with a mineralocorticoid receptor antagonist. Circ Heart Fail 7(4):573–579. https://doi.org/10.1161/CIRCHEARTFAILURE
Khosla N, Kalaitzidis R, Bakris GL (2009) Predictors of hyperkalemia risk following hypertension control with aldosterone blockade. Am J Nephrol 30(5):418–424. https://doi.org/10.1159/000237742
Pelliccia F, Patti G, Rosano G, Greco C, Gaudio C (2014) Efficacy and safety of eplerenone in the management of mild to moderate arterial hypertension: systematic review and meta-analysis. Int J Cardiol 177(1):219–228. https://doi.org/10.1016/j.ijcard.2014.09.091
Eschalier R, McMurray JJ, Swedberg K, van Veldhuisen DJ, Krum H, PocockSJ SH, Vincent J, Rossignol P, Zannad F, Pitt B (2013) Safety and efficacy of eplerenone in patients at high risk for hyperkalemia and/or worsening renal function: analyses of the EMPHASIS-HF study subgroups (Eplerenone in Mild Patients Hospitalization And SurvIval Study in Heart Failure). J Am Coll Cardiol 62(17):1585–1593. https://doi.org/10.1016/j.jacc.2013.04.086
Pitt B, Bakris G, Ruilope LM, DiCarlo L, Mukherjee R (2008) Serum potassium and clinical outcomes in the eplerenone post-acute myocardial infarction heart failure efficacy and survival study (EPHESUS). Circulation 118(16):1643–1650. https://doi.org/10.1161/CIRCULATIONAHA.108.778811
Lai L, Feng X, Liu D, Chen J, Zhang Y, Niu B, Gu Y, Cai H (2012) Dietary salt modulates the sodium chloride cotransporter expression likely through an aldosterone-mediated WNK4-ERK1/2 signaling pathway. Pflugers Arch 463(3):477–485. https://doi.org/10.1007/s00424-011-1062-y
Schiessl IM, Rosenauer A, Kattler V, Minuth WW, Oppermann M, Castrop H (2013) Dietary salt intake modulates differential splicing of the Na-K-2ClcotransporterNKCC2. Am J Physiol Renal Physiol 305(8):F1139–F1148. https://doi.org/10.1152/ajprenal.00259.2013
Mente A, O'Donnell M, Rangarajan S, Dagenais G, Lear S, McQueen M, Diaz R, Avezum A, Lopez-Jaramillo P, Lanas F, Li W, Lu Y, Yi S, Rensheng L, Iqbal R, Mony P, Yusuf R, Yusoff K, Szuba A, Oguz A, Rosengren A, Bahonar A, Yusufali A, Schutte AE, Chifamba J, Mann JF, Anand SS, Teo K, Yusuf S, PURE, EPIDREAM and ONTARGET/TRANSCEND Investigators (2016) Associations of urinary sodium excretion with cardiovascular events in individuals with and without hypertension: a pooled analysis of data from four studies. Lancet 388(10043):465–475. https://doi.org/10.1016/S0140-6736(16)30467-6
Aburto NJ, Ziolkovska A, Hooper L, Elliott P, Cappuccio FP, Meerpohl JJ (2013) Effect of lower sodium intake on health: systematic review and meta-analyses. BMJ 346:f1326. https://doi.org/10.1136/bmj.f1326
Elliott P, Stamler J, Nichols R, Dyer AR, Stamler R, Kesteloot H, Marmot M (1996) Intersalt revisited: further analyses of 24 hour sodium excretion and blood pressure within and across populations. BMJ 312(7041):1249–1253
Mancia G, Fagard R, Narkiewicz K, Redon J, Zanchetti A, Böhm M, Christiaens T, Cifkova R, De Backer G, Dominiczak A, Galderisi M, Grobbee DE, Jaarsma T, Kirchhof P, Kjeldsen SE, Laurent S, Manolis AJ, Nilsson PM, Ruilope LM, Schmieder RE, Sirnes PA, Sleight P, Viigimaa M, Waeber B, Zannad F, Redon J, Dominiczak A, Narkiewicz K, Nilsson PM, Burnier M, Viigimaa M, Ambrosioni E, Caufield M, Coca A, Olsen MH, Schmieder RE, Tsioufis C, van de Borne P, Zamorano JL, Achenbach S, Baumgartner H, Bax JJ, Bueno H, Dean V, Deaton C, Erol C, Fagard R, Ferrari R, Hasdai D, Hoes AW, Kirchhof P, Knuuti J, Kolh P, Lancellotti P, Linhart A, Nihoyannopoulos P, Piepoli MF, Ponikowski P, Sirnes PA, TamargoJL TM, Torbicki A, Wijns W, Windecker S, Clement DL, Coca A, Gillebert TC, Tendera M, Rosei EA, Ambrosioni E, Anker SD, Bauersachs J, HitijJB CM, De Buyzere M, De Geest S, Derumeaux GA, Erdine S, Farsang C, Funck-Brentano C, Gerc V, Germano G, Gielen S, Haller H, Hoes AW, Jordan J, Kahan T, Komajda M, Lovic D, Mahrholdt H, Olsen MH, Ostergren J, Parati G, Perk J, Polonia J, Popescu BA, Reiner Z, Rydén L, Sirenko Y, Stanton A, Struijker-Boudier H, Tsioufis C, van de Borne P, Vlachopoulos C, Volpe M, Wood DA (2013) ESH/ESC Guidelines for the management of arterial hypertension: the task force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J 34(28):2159–2219. https://doi.org/10.1093/eurheartj/eht151
Vos M, Wylie-Rosett J, Kris-Etherton P (2016) American Heart Association Nutrition Committee of the Council on Lifestyle and Cardiometabolic Health; Council on Cardiovascular Disease in the Young; Council on Cardiovascular and Stroke Nursing; Council on Clinical Cardiology; and Stroke Council. Recommended Dietary Pattern to Achieve Adherence to the American Heart Association/American College of Cardiology (AHA/ACC) Guidelines: a Scientific Statement From the American Heart Association. Circulation 134(22):e505–e529. https://doi.org/10.1161/CIR.0000000000000462
Ghazi L, Dudenbostel T, Lin CP, Oparil S, Calhoun DA (2016) Urinary sodium excretion predicts blood pressure response to spironolactone in patients with resistant hypertension independent of aldosterone status. J Hypertens 34(5):1005–1010. https://doi.org/10.1097/HJH.0000000000000870
Author information
Authors and Affiliations
Contributions
SF examined the patients and wrote the article. LP organized the study, analyzed the data, and wrote the article. NV collected the data. TK carried out laboratory work. AM collected the data. GC contributed intellectually and edited the article. GP designed the study and assigned duties. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Informed consent
Informed consent was obtained from all subjects.
Ethical approval
All procedures performed were in accordance with the ethical standards of General Hospital of Athens ‘G. Gennimatas’ research committee and with the 1964 Helsinki declaration and its later amendments.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Fountoulakis, S., Papanastasiou, L., Voulgaris, N. et al. Salt intake in mineralocorticoid receptor antagonist-treated primary aldosteronism: foe or ally?. Hormones 19, 223–232 (2020). https://doi.org/10.1007/s42000-019-00167-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s42000-019-00167-9