Key summary points
Aim To provide an updated overview of studies on under-prescription in older subjects, describing its prevalence, causes, consequences as well as potential interventions to reduce it.
AbstractSection FindingsFindings Under-prescription is common in older patients and associated with negative clinical outcomes, such as higher risk of cardiovascular events, worsening disability, hospitalization and death. Promising interventions to correct it include the implementation of explicit under-prescription criteria, the use of comprehensive geriatric assessment by geriatricians, and the involvement of a clinical pharmacist.
AbstractSection MessageMessage Further studies should be performed to provide a better understanding of under-prescription and to confirm the efficacy of corrective interventions.
Abstract
Purpose
Under-prescription is defined as the omission of a medication that is indicated for the treatment of a condition or a disease, without any valid reason for not prescribing it. The aim of this review is to provide an updated overview of under-prescription, summarizing the available evidence concerning its prevalence, causes, consequences and potential interventions to reduce it.
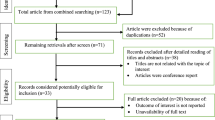
Methods
A PubMed search was performed, using the following keywords: under-prescription; under-treatment; prescribing omission; older adults; polypharmacy; cardiovascular drugs; osteoporosis; anticoagulant. The list of articles was evaluated by two authors who selected the most relevant of them. The reference lists of retrieved articles were screened for additional pertinent studies.
Results
Although several pharmacological therapies are safe and effective in older patients, under-prescription remains widespread in the older population, with a prevalence ranging from 22 to 70%. Several drugs are underused, including cardiovascular, oral anticoagulant and anti-osteoporotic drugs. Many factors are associated with under-prescription, e.g. multi-morbidity, polypharmacy, dementia, frailty, risk of adverse drug events, absence of specific clinical trials in older patients and economic factors. Under-prescription is associated with negative consequences, such as higher risk of cardiovascular events, worsening disability, hospitalization and death. The implementation of explicit criteria for under-prescription, the use of the comprehensive geriatric assessment by geriatricians, and the involvement of a clinical pharmacist seem to be promising options to reduce under-prescription.
Conclusion
Under-prescription remains widespread in the older population. Further studies should be performed, to provide a better comprehension of this phenomenon and to confirm the efficacy of corrective interventions.
Similar content being viewed by others
References
OECD (2019) Health at a Glance 2019: OECD Indicators. OECD Publishing, Paris. https://doi.org/10.1787/4dd50c09-en (Accessed 1 Oct 2020)
Marengoni A, Angleman S, Melis R, Mangialasche F, Karp A, Garmen A, Meinow B, Fratiglioni L (2011) Aging with multimorbidity: a systematic review of the literature. Ageing Res Rev 10(4):430–439. https://doi.org/10.1016/j.arr.2011.03.003 (Epub 2011 Mar 23 PMID: 21402176)
Wolverton D, Elliott DP (2018) Evaluating the evidence behind treating osteoporosis in the oldest adults. Consult Pharm. 33(6):308–316. https://doi.org/10.4140/TCP.n.2018.308
SOLVD Investigators, Yusuf S, Pitt B, Davis CE, Hood WB, Cohn JN (1991) Effect of enalapril on survival in patients with reduced left ventricular ejection fractions and congestive heart failure. N Engl J Med. 325(5):293–302. https://doi.org/10.1056/NEJM199108013250501
Deedwania PC, Gottlieb S, Ghali JK, Waagstein F, Wikstrand JCM (2004) Efficacy, safety and tolerability of β-adrenergic blockade with metoprolol CR/XL in elderly patients with heart failure. Eur Heart J. 25(15):1300–1309. https://doi.org/10.1016/j.ehj.2004.05.022
Hindricks G, Potpara T, Dagres N, Arbelo E, Bax JJ, Blomström-Lundqvist C, Boriani G, Castella M, Dan GA, Dilaveris PE, Fauchier L, Filippatos G, Kalman JM, La Meir M, Lane DA, Lebeau JP, Lettino M, Lip GYH, Pinto FJ, Thomas GN, Valgimigli M, Van Gelder IC, Van Putte BP, Watkins CL, ESC Scientific Document Group (2021) 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association of Cardio-Thoracic Surgery (EACTS). Eur Heart J 42(5):373–498. https://doi.org/10.1093/eurheartj/ehaa612
Zhang N, Sundquist J, Sundquist K, Ji J (2020) An increasing trend in the prevalence of polypharmacy in sweden: a nationwide register-based study. Front Pharmacol. 11:326. https://doi.org/10.3389/fphar.2020.00326
Qato DM, Wilder J, Schumm LP, Gillet V, Alexander GC (2016) Changes in prescription and over-the-counter medication and dietary supplement use among older adults in the United States, 2005 vs 2011. JAMA Intern Med 176(4):473–482. https://doi.org/10.1001/jamainternmed.2015.8581
Moriarty F, Hardy C, Bennett K, Smith SM, Fahey T (2015) Trends and interaction of polypharmacy and potentially inappropriate prescribing in primary care over 15 years in Ireland: a repeated cross-sectional study. BMJ Open 5(9):e008656. https://doi.org/10.1136/bmjopen-2015-008656
Melzer D, Tavakoly B, Winder RE et al (2015) Much more medicine for the oldest old: trends in UK electronic clinical records. Age Ageing. 44(1):46–53. https://doi.org/10.1093/ageing/afu113
Blanco-Reina E, Ariza-Zafra G, Ocaña-Riola R, León-Ortíz M, Bellido-Estévez I (2015) Optimizing elderly pharmacotherapy: polypharmacy vs. undertreatment. Are these two concepts related? Eur J Clin Pharmacol 71(2):199–207. https://doi.org/10.1007/s00228-014-1780-0
Cherubini A, Corsonello A, Lattanzio F (2012) Underprescription of beneficial medicines in older people: causes, consequences and prevention. Drugs Aging. 29(6):463–475. https://doi.org/10.2165/11631750-000000000-00000
Ryan C, O’Mahony D, Kennedy J, Weedle P, Byrne S (2009) Potentially inappropriate prescribing in an Irish elderly population in primary care. Br J Clin Pharmacol. 68(6):936–947. https://doi.org/10.1111/j.1365-2125.2009.03531.x
Barry PJ, Gallagher P, Ryan C, O’mahony D (2007) START (screening tool to alert doctors to the right treatment)—an evidence-based screening tool to detect prescribing omissions in elderly patients. Age Ageing 36(6):632–638. https://doi.org/10.1093/ageing/afm118
Gorup EC, Šter MP (2017) Number of medications or number of diseases: what influences underprescribing? Eur J Clin Pharmacol 73(12):1673–1679. https://doi.org/10.1007/s00228-017-2336-x
Beer C, Hyde Z, Almeida OP et al (2011) Quality use of medicines and health outcomes among a cohort of community dwelling older men: an observational study. Br J Clin Pharmacol 71(4):592–599. https://doi.org/10.1111/j.1365-2125.2010.03875.x
Wright RM, Sloane R, Pieper CF et al (2009) Underuse of indicated medications among physically frail older US veterans at the time of hospital discharge: results of a cross-sectional analysis of data from the Geriatric Evaluation and Management Drug Study. Am J Geriatr Pharmacother. 7(5):271–280. https://doi.org/10.1016/j.amjopharm.2009.11.002
Manias E, Kusljic S, Lam DL (2015) Use of the screening tool of older persons’ prescriptions (STOPP) and the screening tool to alert doctors to the right treatment (START) in hospitalised older people. Australas J Ageing 34(4):252–258. https://doi.org/10.1111/ajag.12186
Gallagher P, Lang PO, Cherubini A et al (2011) Prevalence of potentially inappropriate prescribing in an acutely ill population of older patients admitted to six European hospitals. Eur J Clin Pharmacol 67(11):1175–1188. https://doi.org/10.1007/s00228-011-1061-0
Steinman MA, Seth Landefeld C, Rosenthal GE, Berthenthal D, Sen S, Kaboli PJ (2006) Polypharmacy and prescribing quality in older people. J Am Geriatr Soc 54(10):1516–1523. https://doi.org/10.1111/j.1532-5415.2006.00889.x
Gutiérrez-Valencia M, Izquierdo M, Lacalle-Fabo E et al (2018) Relationship between frailty, polypharmacy, and underprescription in older adults living in nursing homes. Eur J Clin Pharmacol 74(7):961–970. https://doi.org/10.1007/s00228-018-2452-2
García-Gollarte F, Baleriola-Júlvez J, Ferrero-López I, Cruz-Jentoft AJ (2012) Inappropriate drug prescription at nursing home admission. J Am Med Dir Assoc 13(1):83.e9-83.e15. https://doi.org/10.1016/j.jamda.2011.02.009
Lang PO, Hasso Y, Dramé M et al (2010) Potentially inappropriate prescribing including under-use amongst older patients with cognitive or psychiatric co-morbidities. Age Ageing 39(3):373–381. https://doi.org/10.1093/ageing/afq031
Galvin R, Moriarty F, Cousins G et al (2014) Prevalence of potentially inappropriate prescribing and prescribing omissions in older Irish adults: Findings from the Irish LongituDinal Study on Ageing study (TILDA). Eur J Clin Pharmacol 70(5):599–606. https://doi.org/10.1007/s00228-014-1651-8
Storms H, Marquet K, Aertgeerts B, Claes N (2017) Prevalence of inappropriate medication use in residential long-term care facilities for the elderly: a systematic review. Eur J Gen Pract 23(1):69–77. https://doi.org/10.1080/13814788.2017.1288211
San-José A, Agustí A, Vidal X et al (2015) Inappropriate prescribing to the oldest old patients admitted to hospital: Prevalence, most frequently used medicines, and associated factors. BMC Geriatr 15(1):1–9. https://doi.org/10.1186/s12877-015-0038-8
Soumerai SB, McLaughlin TJ, Spiegelman D, Hertzmark E, Thibault G, Goldman L (1997) Adverse outcomes of underuse of β-blockers in elderly survivors of acute myocardial infarction. JAMA 277(2):115–121. https://doi.org/10.1001/jama.277.2.115
Vitagliano G, Curtis JP, Concato J, Feinstein AR, Radford MJ, Krumholz HM (2004) Association between functional status and use and effectiveness of beta-blocker prophylaxis in elderly survivors of acute myocardial infarction. J Am Geriatr Soc. 52(4):495–501. https://doi.org/10.1111/j.1532-5415.2004.52153.x
Zullo AR, Sharmin S, Lee Y et al (2017) Secondary prevention medication use after myocardial infarction in U.S. nursing home residents. J Am Geriatr Soc. 65(11):2397–2404. https://doi.org/10.1111/jgs.15144
Meid AD, Quinzler R, Freigofas J et al (2015) Medication underuse in aging outpatients with cardiovascular disease: prevalence, determinants, and outcomes in a prospective cohort study. PLoS ONE 10(8):1–12. https://doi.org/10.1371/journal.pone.0136339
Ponte Márquez PH, Torres OH, San-José A et al (2017) Potentially inappropriate antihypertensive prescriptions to elderly patients: results of a prospective, observational study on behalf of the potentially inappropriate prescription in older patients in Spain (PIPOPS) investigators’ project. Drugs Aging. 34(6):453–466. https://doi.org/10.1007/s40266-017-0452-z
Strandberg TE (2019) Role of statin therapy in primary prevention of cardiovascular disease in elderly patients. Curr Atheroscler Rep 21(8):28. https://doi.org/10.1007/s11883-019-0793-7
Collaboration CTT (2019) Efficacy and safety of statin therapy in older people: a meta-analysis of individual participant data from 28 randomised controlled trials. Lancet 393(10170):407–415. https://doi.org/10.1016/S0140-6736(18)31942-1
Strandberg TE, Kolehmainen L, Vuorio A (2014) Evaluation and treatment of older patients with hypercholesterolemia: a clinical review. JAMA 312(11):1136–1144. https://doi.org/10.1001/jama.2014.10924 (PMID: 25226479)
Chugh SS, Havmoeller R, Narayanan K et al (2014) Worldwide epidemiology of atrial fibrillation: a global burden of disease 2010 study. Circulation. 129(8):837–847. https://doi.org/10.1161/CIRCULATIONAHA.113.005119
Mant J, Hobbs FR, Fletcher K et al (2007) Warfarin versus aspirin for stroke prevention in an elderly community population with atrial fibrillation (the Birmingham Atrial Fibrillation Treatment of the Aged Study, BAFTA): a randomised controlled trial. Lancet. 370(9586):493–503. https://doi.org/10.1016/S0140-6736(07)61233-1
Ruff CT, Giugliano RP, Braunwald E et al (2014) Comparison of the efficacy and safety of new oral anticoagulants with warfarin in patients with atrial fibrillation: a meta-analysis of randomised trials. Lancet. 383(9921):955–962. https://doi.org/10.1016/S0140-6736(13)62343-0
Kirchhof P, Benussi S, Kotecha D, Ahlsson A, Atar D, Casadei B, Castella M, Diener HC, Heidbuchel H, Hendriks J, Hindricks G, Manolis AS, Oldgren J, Popescu BA, Schotten U, Van Putte B, Vardas P, ESC Scientific Document Group (2016) 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur Heart J 37(38):2893–2962. https://doi.org/10.1093/eurheartj/ehw210 (Epub 2016 Aug 27. PMID: 27567408)
Bo M, Grisoglio E, Brunetti E, Falcone Y, Marchionni N (2017) Oral anticoagulant therapy for older patients with atrial fibrillation: a review of current evidence. Eur J Intern Med. 41:18–27. https://doi.org/10.1016/j.ejim.2017.03.012
Villani ER, Tummolo AM, Palmer K et al (2018) Frailty and atrial fibrillation: a systematic review. Eur J Intern Med. 56:33–38. https://doi.org/10.1016/j.ejim.2018.04.018
Damanti S, Braham S, Pasina L (2019) Anticoagulation in frail older people. J Geriatr Cardiol. 16(11):844–846. https://doi.org/10.11909/j.issn.1671-5411.2019.11.005
Qiu C, Fratiglioni L (2018) Aging without dementia is achievable: current evidence from epidemiological research. J Alzheimer’s Dis. 62(3):933–942. https://doi.org/10.3233/JAD-171037
Lee M, Saver JL, Hong KS et al (2014) Cognitive impairment and risk of future stroke: a systematic review and meta-analysis. CMAJ. 186(14):E536–E546. https://doi.org/10.1503/cmaj.140147
Viscogliosi G, Ettorre E, Chiriac IM (2017) Dementia correlates with anticoagulation underuse in older patients with atrial fibrillation. Arch Gerontol Geriatr. 72:108–112. https://doi.org/10.1016/j.archger.2017.05.014
Orkaby AR, Ozonoff A, Reisman JI, Miller DR, Zhao S, Rose AJ (2017) Continued use of warfarin in veterans with atrial fibrillation after dementia diagnosis. J Am Geriatr Soc. 65(2):249–256. https://doi.org/10.1111/jgs.14573
Besford M, Graham S, Sammon C et al (2020) Factors associated with non-prescription of oral anticoagulant treatment in non-valvular atrial fibrillation patients with dementia: a CPRD–HES study. Age Ageing. 49(4):679–682. https://doi.org/10.1093/ageing/afaa045
Man-Son-Hing M, Nichol G, Lau A, Laupacis A (1999) Choosing antithrombotic therapy for elderly patients with atrial fibrillation who are at risk for falls. Arch Intern Med. 159(7):677–685. https://doi.org/10.1001/archinte.159.7.677
Ceccofiglio A, Fumagalli S, Mussi C, Mossello E, Bo M, Martone AM, Bellelli G, Nicosia F, Riccio D, Langellotto A, Tava G, Boccardi V, Tonon E, Abete P, Ungar A (2020) Atrial fibrillation in older patients with syncope and dementia: insights from the syncope and dementia registry. J Am Med Dir Assoc 21(9):1238–1242. https://doi.org/10.1016/j.jamda.2020.01.110 (Epub 2020 Mar 13 PMID: 32179002)
Kamel HK, Duthie EH (2002) The underuse of therapy in the secondary prevention of hip fractures. Drugs Aging. 19(1):1–10. https://doi.org/10.2165/00002512-200219010-00001
LeBoff MS, Kohlmeier L, Hurwitz S, Franklin J, Wright J, Glowacki J (1999) Occult vitamin D deficiency in postmenopausal US women with acute hip fracture. JAMA. 281(16):1505–1511. https://doi.org/10.1001/jama.281.16.1505
Kamel HK (2004) Underutilization of calcium and vitamin D supplements in an academic long-term care facility. J Am Med Dir Assoc 5(2):98–100. https://doi.org/10.1097/01.jam.0000110649.22467.b4
Lorentzon M, Nilsson AG, Johansson H, Kanis JA, Mellström D, Sundh D (2019) Extensive undertreatment of osteoporosis in older Swedish women. Osteoporos Int 30(6):1297–1305. https://doi.org/10.1007/s00198-019-04872-4 (Epub2019 Feb 25. PMID: 30805678; PMCID: PMC6546648)
Solomon DH, Johnston SS, Boytsov NN, McMorrow D, Lane JM, Krohn KD (2014) Osteoporosis medication use after hip fracture in U.S. patients between 2002 and 2011. J Bone Miner Res. 29(9):1929–1937. https://doi.org/10.1002/jbmr.2202
Fuggle NR, Cooper C, Harvey NC, Al-Daghri N, Brandi ML, Bruyere O, Cano A, Dennison EM, Diez-Perez A, Kaufman JM, Palacios S, Prieto-Alhambra D, Rozenberg S, Thomas T, Tremollieres F, Rizzoli R, Kanis JA, Reginster JY (2020) Assessment of cardiovascular safety of anti-osteoporosis drugs. Drugs 80(15):1537–1552. https://doi.org/10.1007/s40265-020-01364-2 (PMID:32725307; PMCID:PMC7536167)
Khan M, Cheung AM, Khan AA (2017) Drug-related adverse events of osteoporosis therapy. Endocrinol Metab Clin North Am 46(1):181–192. https://doi.org/10.1016/j.ecl.2016.09.009 (Epub 2016 Nov 25 PMID: 28131131)
Skjødt MK, Frost M, Abrahamsen B (2019) Side effects of drugs for osteoporosis and metastatic bone disease. Br J Clin Pharmacol 85(6):1063–1071. https://doi.org/10.1111/bcp.13759 (Epub 2018 Oct 17. PMID: 30192026; PMCID: PMC6533454)
Khosla S, Hofbauer LC (2017) Osteoporosis treatment: recent developments and ongoing challenges. Lancet Diabetes Endocrinol. 5(11):898–907. https://doi.org/10.1016/S2213-8587(17)30188-2 (Epub 2017 Jul 7. PMID: 28689769; PMCID: PMC5798872)
Albert SG, Reddy S (2017) Clinical evaluation of cost efficacy of drugs for treatment of osteoporosis: a meta-analysis. Endocr Pract 23(7):841–856. https://doi.org/10.4158/EP161678.RA (Epub 2017 Apr 27 PMID: 28448754)
Dodson TB (2015) The frequency of medication-related osteonecrosis of the jaw and its associated risk factors. Oral Maxillofac Surg Clin North Am 27(4):509–516. https://doi.org/10.1016/j.coms.2015.06.003 (Epub 2015 Sep 9 PMID: 26362367)
Cherubini A, Oristrell J, Pla X et al (2011) The persistent exclusion of older patients from ongoing clinical trials regarding heart failure. Arch Intern Med. 171(6):550–556. https://doi.org/10.1001/archinternmed.2011.31
Cherubini A, Del Signore S, Ouslander J, Semla T, Michel JP (2010) Fighting against age discrimination in clinical trials. J Am Geriatr Soc. 58(9):1791–1796. https://doi.org/10.1111/j.1532-5415.2010.03032.x.
Palmer K, Villani ER, Vetrano DL, Cherubini A, Cruz-Jentoft AJ, Curtin D, Denkinger M, Gutiérrez-Valencia M, Guðmundsson A, Knol W, Mak DV, O’Mahony D, Pazan F, Petrovic M, Rajkumar C, Topinkova E, Trevisan C, van der Cammen TJM, van Marum RJ, Wehling M, Ziere G, Bernabei R, Onder G, European Geriatric Medicine Society Pharmacology special interest group (2019) Association of polypharmacy and hyperpolypharmacy with frailty states: a systematic review and meta-analysis. Eur Geriatr Med 10(1):9–36. https://doi.org/10.1007/s41999-018-0124-5 (Epub 2018 Nov 7. PMID: 32720270)
Gutiérrez-Valencia M, Martínez-Velilla N, Vilches-Moraga A (2019) Polypharmacy in older people: time to take action. Eur Geriatr Med 10(1):1–3. https://doi.org/10.1007/s41999-018-0140-5 (Epub 2018 Nov 30 PMID: 32720284)
Tinetti ME, Bogardus ST, Agostini JV (2004) Potential pitfalls of disease-specific guidelines for patients with multiple conditions. N Engl J Med. 351(27):2870–2874. https://doi.org/10.1056/NEJMsb042458
Marengoni A, Onder G (2015) Guidelines, polypharmacy, and drug-drug interactions in patients with multimorbidity. BMJ 11(350):h1059. https://doi.org/10.1136/bmj.h1059 (PMID: 25761379)
Cadogan CA, Ryan C, Hughes CM (2016) Appropriate polypharmacy and medicine safety: when many is not too many. Drug Saf 39(2):109–116. https://doi.org/10.1007/s40264-015-0378-5 (PMID:26692396;PMCID:PMC4735229)
Kuijpers MAJ, Van Marum RJ, Egberts ACG, Jansen PAF (2008) Relationship between polypharmacy and underprescribing. Br J Clin Pharmacol 65(1):130–133. https://doi.org/10.1111/j.1365-2125.2007.02961.x
Winkelmayer WC, Fischer MA, Schneeweiss S, Wang PS, Levin R, Avorn J (2005) Underuse of ACE inhibitors and angiotensin II receptor blockers in elderly patients with diabetes. Am J Kidney Dis. 46(6):1080–1087. https://doi.org/10.1053/j.ajkd.2005.08.018
Cherubini A, Ruggiero C, Dell’Aquila G et al (2012) Underrecognition and undertreatment of dementia in italian nursing homes. J Am Med Dir Assoc. 13(8):759.e7-13. https://doi.org/10.1016/j.jamda.2012.05.015
Holmes HM, Hayley DC, Alexander GC, Sachs GA (2006) Reconsidering medication appropriateness for patients late in life. Arch Intern Med 166(6):605–609. https://doi.org/10.1001/archinte.166.6.605 (PMID: 16567597)
Kulik A, Desai NR, Shrank WH et al (2013) Full prescription coverage versus usual prescription coverage after coronary artery bypass graft surgery: analysis from the post-myocardial infarction free rx event and economic evaluation (FREEE) randomized trial. Circulation. 128(11 Suppl 1):S219-S225. https://doi.org/10.1161/CIRCULATIONAHA.112.000337
Gallagher PF, O’Connor MN, O’Mahony D (2011) Prevention of potentially inappropriate prescribing for elderly patients: a randomized controlled trial using STOPP/START criteria. Clin Pharmacol Ther 89(6):845–854. https://doi.org/10.1038/clpt.2011.44 (Epub 2011 Apr 20 PMID: 21508941)
San-José A, Agustí A, Vidal X, Barbé J, Torres OH, Ramírez-Duque N, García J, Fernández-Moyano A, López-Soto A, Formiga F (2014) Potentially Inappropriate Prescribing in Older Patients in Spain (PIPOPS) Investigators’ project. An inter-rater reliability study of the prescribing indicated medications quality indicators of the Assessing Care Of Vulnerable Elders (ACOVE) 3 criteria as a potentially inappropriate prescribing tool. Arch Gerontol Geriatr 58(3):460–464. https://doi.org/10.1016/j.archger.2013.12.006 (Epub 2014 Jan 2. PMID: 24438879)
Curtin D, Gallagher PF, O’Mahony D (2019) Explicit criteria as clinical tools to minimize inappropriate medication use and its consequences. Ther Adv Drug Saf 13(10):2042098619829431. https://doi.org/10.1177/2042098619829431 (PMID:30800270;PMCID:PMC6378636)
Rabenberg A, Schulte T, Hildebrandt H, Wehling M (2019) The FORTA (Fit fOR The Aged)-EPI (Epidemiological) algorithm: application of an information technology tool for the epidemiological assessment of drug treatment in older people. Drugs Aging 36(10):969–978. https://doi.org/10.1007/s40266-019-00703-7 (PMID: 31435913)
Stojanović M, Vuković M, Jovanović M, Dimitrijević S, Radenković M (2020) GheOP<sup>3</sup> S tool and START/STOPP criteria version 2 for screening of potentially inappropriate medications and omissions in nursing home residents. J Eval Clin Pract 26(1):158–164. https://doi.org/10.1111/jep.13107 (Epub 2019 Feb 5 PMID: 30722098)
Forsetlund L, Eike MC, Gjerberg E, Vist GE (2011) Effect of interventions to reduce potentially inappropriate use of drugs in nursing homes: a systematic review of randomised controlled trials. BMC Geriatr. 11:16. https://doi.org/10.1186/1471-2318-11-16
Alldred DP, Kennedy MC, Hughes C, Chen TF, Miller P (2016) Interventions to optimise prescribing for older people in care homes. Cochrane Database Syst Rev. 2(2):CD009095.https://doi.org/10.1002/14651858.CD009095.pub3
Wehling M, Burkhardt H, Kuhn-Thiel A, Pazan F, Throm C, Weiss C, Frohnhofen H (2016) VALFORTA: a randomised trial to validate the FORTA (Fit fOR The Aged) classification. Age Ageing 45(2):262–267. https://doi.org/10.1093/ageing/afv200 (Epub 2016 Jan 18 PMID: 26786346)
Lee J, Alshehri S, Kutbi H, Martin J (2015) Optimizing pharmacotherapy in elderly patients: the role of pharmacists. Integr Pharm Res Pract. 4:101–111. https://doi.org/10.2147/IPRP.S70404.
Kim J, Tofade TS, Peckman H (2009) Caring for the elderly in an inpatient setting: managing insomnia and polypharmacy. J Pharm Pract. 22(5):494–506. https://doi.org/10.1177/0897190008330199
Gillespie U, Alassaad A, Hammarlund-Udenaes M et al (2013) Effects of pharmacists’ interventions on appropriateness of prescribing and evaluation of the instruments’ (MAI, STOPP and STARTs’) ability to predict hospitalization-analyses from a randomized controlled trial. PLoS One. 8(5):e62401. https://doi.org/10.1371/journal.pone.0062401
Spinewine A, Swine C, Dhillon S, Lambert P, Nachega JB, Wilmotte L, Tulkens PM (2007) Effect of a collaborative approach on the quality of prescribing for geriatric inpatients: a randomized, controlled trial. J Am Geriatr Soc 55(5):658–665. https://doi.org/10.1111/j.1532-5415.2007.01132.x (PMID: 17493184)
Crotty M, Whitehead C, Rowett D, Halbert J, Weller D, Finucane P, Esterman A (2004) An outreach intervention to implement evidence based practice in residential care: a randomized controlled trial [ISRCTN67855475]. BMC Health Serv Res 4(1):6. https://doi.org/10.1186/1472-6963-4-6
Tulner LR, Van Campen JPCM, Frankfort SV et al (2010) Changes in under-treatment after comprehensive geriatric assessment: an observational study. Drugs Aging. 27(10):831–843. https://doi.org/10.2165/11539330-000000000-00000
Lea SC, Watts KL, Davis NA et al (2017) The potential clinical benefits of medicines optimisation through comprehensive geriatric assessment, carried out by secondary care geriatricians, in a general practice care setting in North Staffordshire, UK: A feasibility study. BMJ Open. 7(9):e015278. https://doi.org/10.1136/bmjopen-2016-015278
Romskaug R, Skovlund E, Straand J, Molden E, Kersten H, Pitkala KH, Lundqvist C, Wyller TB (2020) Effect of clinical geriatric assessments and collaborative medication reviews by geriatrician and family physician for improving health-related quality of life in home-dwelling older patients receiving polypharmacy: a cluster randomized clinical trial. JAMA Intern Med 180(2):181–189. https://doi.org/10.1001/jamainternmed.2019.5096
Strauven G, Anrys P, Vandael E et al (2019) Cluster-controlled trial of an intervention to improve prescribing in nursing homes study. J Am Med Dir Assoc. 20(11):1404–1411. https://doi.org/10.1016/j.jamda.2019.06.006
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Ethical approval
No ethical approval was requested for this study since it was a review of published literature.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lombardi, F., Paoletti, L., Carrieri, B. et al. Underprescription of medications in older adults: causes, consequences and solutions—a narrative review. Eur Geriatr Med 12, 453–462 (2021). https://doi.org/10.1007/s41999-021-00471-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41999-021-00471-x