Abstract
Purpose
We aimed to perform a longitudinal assessment of the quality of life of cervical cancer survivors comparing statistical significance with minimal clinically important difference.
Methods
We conducted a prospective cohort study on the quality of life of 106 cervical cancer survivors between August 1, 2016 and January 31, 2019. The self-reported measures included the FACT-Cx v.4.0 and the WHOQOL-BREF questionnaires.
Results
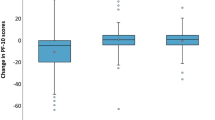
We found no statistically significant changes in the quality of life (p > 0.05), except for a significant worsening in the group that underwent primary surgery and adjuvant radiation therapy and chemotherapy (p = 0.041). However, we observed minimal clinically important differences for all questionnaires regarding the total score (7.81 vs. 23.83 vs. 11.5 vs. 15.5 vs. 26.87 SDs), “physical” (7.28 vs. 4.75 vs. 5.13 vs. 3.79 vs. 4.95 SDs), “functional” (7.87 vs. 4.84 vs. 3.21 vs. 6.93 vs. 12.02 SDs), “emotional” (4.12 vs. 2.34 vs. 1 vs. 1 vs. 3.54 SDs; except for the comparison between the questionnaires at 12–24 months and 24–60 months after the end of the therapy), and “additional concerns” (8.59 vs. 11.13 vs. 8.19 vs. 6.93 vs. 5.66 SDs; except for the comparison between the questionnaires at 0–6 months and 12–24 months after the end of the therapy) domains of the FACT-Cx. The quality of life of long-term cervical cancer survivors was moderate-optimal regarding WHOQOL-BREF questionnaire scores (minimum “psychological healtha”: 48 ± 14.04; maximum “environmentd” 67.46 ± 20.40).
Conclusions
The quality of life of long-term cervical cancer survivors was moderate-optimal. No significant changes in the quality of life were found. However, considering minimal clinically important differences, there was an improvement of the quality of life throughout the follow-up.


Similar content being viewed by others
Data Availability
The data that support the findings of this study are available from the corresponding author upon reasonable request. The data are not publicly available due to the fact that their containing information could compromise the privacy of research participants.
Code Availability
Not applicable.
References
Vistad I, Fosså SD, Dahl AA. A critical review of patient-rated quality of life studies of long-term survivors of cervical cancer. Gynecol Oncol. 2006;102(3):563–72. https://doi.org/10.1016/j.ygyno.2006.03.050.
Cella D, Huang HQ, Monk BJ, Wenzel L, Benda J, McMeekin DS, et al. Health-related quality of life outcomes associated with four cisplatin-based doublet chemotherapy regimens for stage IVB recurrent or persistent cervical cancer: a gynecologic oncology group study. Gynecol Oncol. 2010;119(3):531–7. https://doi.org/10.1016/j.ygyno.2010.08.020.
Fadhilla HN, Mudigdo A, Rahardjo SS. Effect of age and socio economic status on the quality of life of patients with cervical cancer undertaking chemotherapy at Dr. Moewardi Hospital Surakarta. J Epidemiol Public Health. 2017;02(01):11–9.
Jensen PT, Groenvold M, Klee MC, Thranov I, Petersen MA, Machin D. Early-stage cervical carcinoma, radical hysterectomy, and sexual function. Cancer. 2003;100(1):97–106. https://doi.org/10.1002/cncr.11877.
Afiyanti Y, Wardani IY, Martha E. The quality of life of women with cervical cancer in Indonesia: a cross-sectional study. Nurse Med J Nurs. 2019;9(2):128. https://doi.org/10.14710/nmjn.v9i2.26014.
Greimel ER, Winter R, Kapp KS, Haas J. Quality of life and sexual functioning after cervical cancer treatment: a long-term follow-up study. Psychooncology. 2009;18(5):476–82. https://doi.org/10.1002/pon.1426.
Pasek M, Urbański K, Suchocka L. Quality of life in advanced cervical cancer patients subjected to radiotherapy — a WHOQOL BREF questionnaire study. Psycho-Oncologie. 2013;7(2):107–12. https://doi.org/10.1007/s11839-013-0413-7.
Mandrekar S, Dueck A. Future directions in QOL research. Curr Probl Cancer. 2005;29(6):343–51. https://doi.org/10.1016/j.currproblcancer.2005.09.009.
Osoba D. A taxonomy of the uses of health-related quality-of-life instruments in cancer care and the clinical meaningfulness of the results. Med Care. 2002;40(Supplement):III31–8.
Castillo-Ávila IY, Canencia-Padilla J, Zurbarán-Lamadrid M, Pertuz-Cantillo D, Montes-Padilla M, Jiménez-Chacón E. Calidad de vida en mujeres con cáncer cérvico-uterino, Cartagena (Colombia), 2012. Rev Colomb Obstet Ginecol. 2015;66(1):22. https://doi.org/10.18597/rcog.4.
Sánchez R, Villamizar L, Ortiz N. Validación de la escala FACT-Cx en Colombia usando el modelo de teoría de respuesta al ítem. Revista Colombiana de Cancerología. 2011;15(1):13–21. https://doi.org/10.1016/s0123-9015(11)70076-2.
Cella D, Hernandez L, Bonomi AE, Corona M, Vaquero M, Shiomoto G, et al. Spanish language translation and initial validation of the functional assessment of cancer therapy quality-of-life instrument. Med Care. 1998;36(9):1407–18. https://doi.org/10.1097/00005650-199809000-00012.
Benítez-Borrego S, Guàrdia-Olmos J, Urzúa-Morales A. Factorial structural analysis of the Spanish version of WHOQOL-BREF: an exploratory structural equation model study. Qual Life Res. 2014;23(8):2205–12. https://doi.org/10.1007/s11136-014-0663-2.
Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Hillsdale: L. Erlbaum Associates; 1988.
Machin D, Campbell MJ, Tan S-B, Tan S-H, Tan S. Sample Size Tables for Clinical Studies. Somerset: Wiley; 2011.
Cella DF, Tulsky DS, Gray G, Sarafian B, Linn E, Bonomi A, et al. The functional assessment of cancer therapy scale: development and validation of the general measure. J Clin Oncol. 1993;11(3):570–9. https://doi.org/10.1200/jco.1993.11.3.570.
Yost KJ, Eton DT, García SF, Cella D. Minimally important differences were estimated for six patient-reported outcomes measurement information system-cancer scales in advanced-stage cancer patients. J Clin Epidemiol. 2011;64(5):507–16. https://doi.org/10.1016/j.jclinepi.2010.11.018.
Norman GR, Sloan JA, Wyrwich KW. Interpretation of changes in health-related quality of life. Med Care. 2003;41(5):582–92. https://doi.org/10.1097/01.mlr.0000062554.74615.4c.
Pauler DK, McCoy S, Moinpour C. Pattern mixture models for longitudinal quality of life studies in advanced stage disease. Stat Med. 2003;22(5):795–809. https://doi.org/10.1002/sim.1397.
EPIDAT - Consellería de Sanidade - Servizo Galego de Saúde [Internet]. 2023. www.sergas.es. https://www.sergas.es/Saude-publica/EPIDAT
Le Borgne G, Mercier M, Woronoff A-S, Guizard A-V, Abeilard E, Caravati-Jouvenceaux A, et al. Quality of life in long-term cervical cancer survivors: a population-based study. Gynecol Oncol. 2013;129(1):222–8. https://doi.org/10.1016/j.ygyno.2012.12.033.
Greenwald HP, McCorkle R, Baumgartner K, Gotay C, Neale AV. Quality of life and disparities among long-term cervical cancer survivors. J Cancer Surviv. 2014;8(3):419–26. https://doi.org/10.1007/s11764-014-0352-8.
Kim M-K, Sim JA, Yun YH, Bae D-S, Nam JH, Park CT, et al. Health-related quality of life and sociodemographic characteristics as prognostic indicators of long-term survival in disease-free cervical cancer survivors. Int J Gynecol Cancer. 2016;26(4):743–9. https://doi.org/10.1097/igc.0000000000000665.
Corney RH, Everett H, Howells A, Crowther ME. Psychosocial adjustment following major gynaecological surgery for carcinoma of the cervix and vulva. J Psychosom Res. 1992;36(6):561–8. https://doi.org/10.1016/0022-3999(92)90041-y.
Pearman T. Quality of life and psychosocial adjustment in gynecologic cancer survivors. Health Qual Life Outcomes. 2003;1(1):33. https://doi.org/10.1186/1477-7525-1-33.
Greimel E, Thiel I, Peintinger F, Cegnar I, Pongratz E. Prospective assessment of quality of life of female cancer patients. Gynecol Oncol. 2002;85(1):140–7. https://doi.org/10.1006/gyno.2002.6586.
Barker CL, Routledge JA, Farnell DJJ, Swindell R, Davidson SE. The impact of radiotherapy late effects on quality of life in gynaecological cancer patients. Br J Cancer. 2009;100(10):1558–65. https://doi.org/10.1038/sj.bjc.6605050.
Ljuca D, Marosevic G. Quality of life in patients with cervical cancer FIGO IIb stage after concomitant chemoradiotherapy. Radiol Oncol. 2009. https://doi.org/10.2478/v10019-009-0025-9.
Kumar S, Rana ML, Verma K, Singh N, Sharma AK, Maria AK, et al. PrediQt-Cx: post treatment health related quality of life prediction model for cervical cancer patients. PLoS ONE. 2014;9(2):e89851. https://doi.org/10.2478/v10019-009-0025-9.
Ferrandina G, Mantegna G, Petrillo M, Fuoco G, Venditti L, Terzano S, et al. Quality of life and emotional distress in early stage and locally advanced cervical cancer patients: a prospective, longitudinal study. Gynecol Oncol. 2012;124(3):389–94. https://doi.org/10.1016/j.ygyno.2011.09.041.
Dahiya N, Acharya AS, Bachani D, Sharma D, Gupta S, Haresh K, Rath G. Quality of life of patients with advanced cervical cancer before and after chemoradiotherapy. Asian Pac J Cancer Prev. 2016;17(7):3095–9.
Matulonis UA, Huang HQ, Filiaci VL, Randall M, DiSilvestro PA, Moxley KM, et al. Patient reported outcomes for cisplatin and radiation followed by carboplatin/paclitaxel versus carboplatin/paclitaxel for locally advanced endometrial carcinoma: an NRG oncology study. Gynecol Oncol. 2022;164(2):428–36. https://doi.org/10.1016/j.ygyno.2021.11.021.
Hopwood P, Stephens RJ, Machin D. Approaches to the analysis of quality of life data: experiences gained from a medical research council lung cancer working party palliative chemotherapy trial. Qual Life Res. 1994;3(5):339–52. https://doi.org/10.1007/bf00451726.
Hu X, Jing M, Zhang M, Yang P, Yan X. Responsiveness and minimal clinically important difference of the EQ-5D-5L in cervical intraepithelial neoplasia: a longitudinal study. Health Qual Life Outcomes. 2020. https://doi.org/10.1186/s12955-020-01578-8.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
All authors met the authorship criteria. JCG: investigation, conceptualization, methodology, writing—original draft preparation, visualization, writing-reviewing and editing. LR-P: methodology, software, data curation, formal analysis, validation, writing—reviewing and editing, and supervision. MCRR: supervision. FMM: resources and supervision. IRJ: resources and supervision. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no competing interests to report.
Ethical Approval
The research project was approved by the Research Ethics Committee of our institution, according to the requirements of Spanish Law 14/2007 of July 3 on biomedical research and the 1964 Declaration of Helsinki.
Informed Consent
The research assistant obtained a written informed consent from each subject before each interview to participate and publish her data; participants were assured that they could stop the study process at any time and were assured that nonparticipation would have no consequences for their follow-up care or therapy. There was no refund for the participants.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
M. Carmen Rubio Rodríguez: Chief of Department; Francisco Márquez Maraver: Chief of Advanced Gynecological Surgery Unit for Women in INSEGO, Vithas-Nisa Aljarafe Hospital.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Cea García, J., Ríos-Pena, L., Rubio Rodríguez, M.C. et al. Longitudinal Assessment of the Quality of Life of Cervical Cancer Survivors from a Tertiary Hospital in Seville, Spain: Does Statistical Significance Equate to Clinical Relevance?. Indian J Gynecol Oncolog 22, 24 (2024). https://doi.org/10.1007/s40944-023-00793-7
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40944-023-00793-7