Abstract
Purpose of Review
Complex nocturnal movements and behaviors are the manifestation of numerous disorders encountered in clinical practice, which are challenging to diagnose due to overlapping clinical manifestations and limitations of the clinical history. We review the three most common causes of complex nocturnal behaviors, disorders of arousal (DOAs) from non-rapid eye movement (NREM) sleep, REM sleep behavior disorder (RBD), and sleep hypermotor epilepsy (SHE), and their overlapping manifestations that can stump clinicians.
Recent Findings
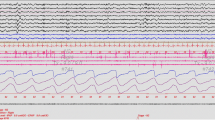
Correlation of semiology with electrical signals (electro-clinical correlation) is key to the diagnosis. Emerging science is demonstrating a shared pathophysiology of SHE and DOAs and RBD as a precursor of neurodegenerative disorders, underscoring the importance of diagnostic accuracy in the sleep and EEG laboratory.
Summary
The evaluation of complex nocturnal movements and behaviors requires a detailed clinical history taken from the patient and observers, video recordings, and in most cases, EEG/PSG confirmation.




Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Chiosa V, Ciolac D, Groppa S, Koirala N, Pintea B, Vataman A, et al. Large-scale network architecture and associated structural cortico-subcortical abnormalities in patients with sleep/awake-related seizures. Sleep. 2019;42(4):zsz006.
•• Tinuper P, Bisulli F, Cross JH, Hesdorffer D, Kahane P, Nobili L, et al. Definition and diagnostic criteria of sleep-related hypermotor epilepsy. Neurology. 2016;86(19):1834–42. This study described the consensus that modified the term nocturnal frontal lobe epilepsy (NFLE) to sleep hypermotor epilepsy (SHE).
Derry CP, Davey M, Johns M, Kron K, Glencross D, Marini C, et al. Distinguishing sleep disorders from seizures: diagnosing bumps in the night. Arch Neurol. 2006;63(5):705–9.
Menghi V, Bisulli F, Tinuper P, Nobili L. Sleep-related hypermotor epilepsy: prevalence, impact and management strategies. Nat Sci Sleep. 2018;10:317–26.
•• Gibbs SA, Proserpio P, Francione S, Mai R, Cardinale F, Sartori I, et al. Clinical features of sleep-related hypermotor epilepsy in relation to the seizure-onset zone: a review of 135 surgically treated cases. Epilepsia. 2019;60(4):707–17. This study shows that the presence of certain semiology patterns (SP) and nonmotor manifestations provide localizing value in patients with SHE.
Licchetta L, Bisulli F, Vignatelli L, Zenesini C, Di Vito L, Mostacci B, et al. Sleep-related hypermotor epilepsy: long-term outcome in a large cohort. Neurology. 2017;88(1):70–7.
Gibbs SA, Proserpio P, Terzaghi M, Pigorini A, Sarasso S, Lo Russo G, et al. Sleep-related epileptic behaviors and non-REM-related parasomnias: insights from stereo-EEG. Sleep Med Rev. 2016;25:4–20.
Nobili L, Cardinale F, Magliola U, Cicolin A, Didato G, Bramerio M, et al. Taylor’s focal cortical dysplasia increases the risk of sleep-related epilepsy. Epilepsia. 2009;50(12):2599–604.
Provini F, Plazzi G, Tinuper P, Vandi S, Lugaresi E, Montagna P. Nocturnal frontal lobe epilepsy. A clinical and polygraphic overview of 100 consecutive cases. Brain. 1999;122(Pt 6):1017–31.
Mostacci B, Troisi S, Bisulli F, Zenesini C, Licchetta L, Provini F, et al. Seizure worsening in pregnancy in women with sleep-related hypermotor epilepsy (SHE): a historical cohort study. Seizure. 2021;91:258–62.
Lugaresi E, Cirignotta F. Hypnogenic paroxysmal dystonia: epileptic seizure or a new syndrome? Sleep. 1981;4(2):129–38.
Wan H, Wang X, Chen Y, Jiang B, Chen Y, Hu W, et al. Sleep-related hypermotor epilepsy: etiology, electro-clinical features, and therapeutic strategies. Nat Sci Sleep. 2021;13:2065–84.
• Proserpio P, Loddo G, Zubler F, Ferini-Strambi L, Licchetta L, Bisulli F, et al. Polysomnographic features differentiating disorder of arousals from sleep-related hypermotor epilepsy. Sleep. 2019;42(12):zsz166. This article highlights that the value of sleep stage and relative time of occurrence of minor and major motor manifestations in relation to sleep onset for discriminating DOA and SHE episodes.
Rheims S, Ryvlin P, Scherer C, Minotti L, Hoffmann D, Guenot M, et al. Analysis of clinical patterns and underlying epileptogenic zones of hypermotor seizures. Epilepsia. 2008;49(12):2030–40.
Bisulli F, Licchetta L, Tinuper P. Sleep related hyper motor epilepsy (SHE): a unique syndrome with heterogeneous genetic etiologies. Sleep Science and Practice. 2019;3(1):3.
Wu T, Avidan AY, Engel J. Sleep and epilepsy, clinical spectrum and updated review. Sleep Med Clin. 2021;16(2):389–408.
Chassoux F, Landré E, Mellerio C, Turak B, Mann MW, Daumas-Duport C, et al. Type II focal cortical dysplasia: electroclinical phenotype and surgical outcome related to imaging. Epilepsia. 2012;53(2):349–58.
Steinlein OK, Mulley JC, Propping P, Wallace RH, Phillips HA, Sutherland GR, et al. A missense mutation in the neuronal nicotinic acetylcholine receptor alpha 4 subunit is associated with autosomal dominant nocturnal frontal lobe epilepsy. Nat Genet. 1995;11(2):201–3.
Halász P, Szűcs A. Sleep and epilepsy link by plasticity. Front Neurol. 2020;11:911.
Heron SE, Smith KR, Bahlo M, Nobili L, Kahana E, Licchetta L, et al. Missense mutations in the sodium-gated potassium channel gene KCNT1 cause severe autosomal dominant nocturnal frontal lobe epilepsy. Nat Genet. 2012;44(11):1188–90.
Dibbens LM, de Vries B, Donatello S, Heron SE, Hodgson BL, Chintawar S, et al. Mutations in DEPDC5 cause familial focal epilepsy with variable foci. Nat Genet. 2013;45(5):546–51.
Weckhuysen S, Marsan E, Lambrecq V, Marchal C, Morin-Brureau M, An-Gourfinkel I, et al. Involvement of GATOR complex genes in familial focal epilepsies and focal cortical dysplasia. Epilepsia. 2016;57(6):994–1003.
Gibbs SA, Proserpio P, Francione S, Mai R, Cossu M, Tassi L, et al. Seizure duration and latency of hypermotor manifestations distinguish frontal from extrafrontal onset in sleep-related hypermotor epilepsy. Epilepsia. 2018;59(9):e130–4.
Kumar J, Solaiman A, Mahakkanukrauh P, Mohamed R, Das S. Sleep related epilepsy and pharmacotherapy: an insight. Front Pharmacol. 2018;27(9):1088.
Asioli GM, Rossi S, Bisulli F, Licchetta L, Tinuper P, Provini F. Therapy in sleep-related hypermotor epilepsy (SHE). Curr Treat Options Neurol. 2020;22(1):1.
Oldani A, Manconi M, Zucconi M, Martinelli C, Ferini-Strambi L. Topiramate treatment for nocturnal frontal lobe epilepsy. Seizure. 2006;15(8):649–52.
Lim SN, Cheng MY, Hsieh HY, Chiang HI, Wu T. Treatment of pharmacoresistant sleep-related hypermotor epilepsy (SHE) with the selective AMPA receptor antagonist perampanel. Sleep Med. 2021;81:382–6.
Nobili L, Francione S, Mai R, Cardinale F, Castana L, Tassi L, et al. Surgical treatment of drug-resistant nocturnal frontal lobe epilepsy. Brain. 2007;130(Pt 2):561–73.
Nobili L, Sartori I, Terzaghi M, Stefano F, Mai R, Tassi L, et al. Relationship of epileptic discharges to arousal instability and periodic leg movements in a case of nocturnal frontal lobe epilepsy: a stereo-EEG study. Sleep. 2006;29(5):701–4.
Losurdo A, Proserpio P, Cardinale F, Gozzo F, Tassi L, Mai R, et al. Drug-resistant focal sleep related epilepsy: results and predictors of surgical outcome. Epilepsy Res. 2014;108(5):953–62.
Sateia MJ. International classification of sleep disorders-third edition: highlights and modifications. Chest. 2014;146(5):1387–94.
Ohayon MM, Guilleminault C, Priest RG. Night terrors, sleepwalking, and confusional arousals in the general population: their frequency and relationship to other sleep and mental disorders. J Clin Psychiatry. 1999;60(4):268–76 (quiz 277).
Guilleminault C, Palombini L, Pelayo R, Chervin RD. Sleepwalking and sleep terrors in prepubertal children: what triggers them? Pediatrics. 2003;111(1):e17-25.
Idir Y, Oudiette D, Arnulf I. Sleepwalking, sleep terrors, sexsomnia and other disorders of arousal: the old and the new. J Sleep Res. 2022;6: e13596.
Schenck CH, Milner DM, Hurwitz TD, Bundlie SR, Mahowald MW. A polysomnographic and clinical report on sleep-related injury in 100 adult patients. Am J Psychiatry. 1989;146(9):1166–73.
•• International Classification of Sleep Disorders. Third edition. Darien, IL: American Academy of Sleep Medicine; 2014. The ICSD-3 is the authoritative clinical text for the classification of sleep disorders.
Castelnovo A, Lopez R, Proserpio P, Nobili L, Dauvilliers Y. NREM sleep parasomnias as disorders of sleep-state dissociation. Nat Rev Neurol. 2018;14(8):470–81.
Irfan M, Schenck CH, Howell MJ. NonREM disorders of arousal and related parasomnias: an updated review. Neurotherapeutics. 2021;18(1):124–39.
Bjorvatn B, Grønli J, Pallesen S. Prevalence of different parasomnias in the general population. Sleep Med. 2010;11(10):1031–4.
Ohayon MM, Priest RG, Zulley J, Smirne S. The place of confusional arousals in sleep and mental disorders: findings in a general population sample of 13,057 subjects. J Nerv Ment Dis. 2000;188(6):340–8.
Leung AKC, Leung AAM, Wong AHC, Hon KL. Sleep terrors: an updated review. Curr Pediatr Rev. 2020;16(3):176–82.
Stallman HM, Kohler M. Prevalence of sleepwalking: a systematic review and meta-analysis. PLoS ONE. 2016;11(11): e0164769.
Crisp AH. The sleepwalking/night terrors syndrome in adults. Postgrad Med J. 1996;72(852):599–604.
Winkelman JW, Wipper B, Purks J, Mei L, Schoerning L. Topiramate reduces nocturnal eating in sleep-related eating disorder. Sleep. 2020;43(9):zsaa060.
Inoue Y. Sleep-related eating disorder and its associated conditions. Psychiatry Clin Neurosci. 2015;69(6):309–20.
Loddo G, Sessagesimi E, Mignani F, Cirignotta F, Mondini S, Licchetta L, et al. Specific motor patterns of arousal disorders in adults: a video-polysomnographic analysis of 184 episodes. Sleep Med. 2018;41:102–9.
Kales A, Soldatos CR, Bixler EO, Ladda RL, Charney DS, Weber G, et al. Hereditary factors in sleepwalking and night terrors. Br J Psychiatry. 1980;137:111–8.
•• Petit D, Pennestri MH, Paquet J, Desautels A, Zadra A, Vitaro F, et al. Childhood sleepwalking and sleep terrors: a longitudinal study of prevalence and familial aggregation. JAMA Pediatr. 2015;169(7):653–8. This study highlights the strong familial aggregation of childhood SW and ST.
Kalantari N, McDuff P, Pilon M, Desautels A, Montplaisir JY, Zadra A. Self-reported developmental changes in the frequency and characteristics of somnambulistic and sleep terror episodes in chronic sleepwalkers. Sleep Med. 2022;89:147–55.
Stallman HM, Kohler M, White J. Medication induced sleepwalking: a systematic review. Sleep Med Rev. 2018;37:105–13.
FULL PRESCRIBING INFORMATION: CONTENTS* WARNING: CENTRAL NERVOUS SYSTEM (CNS) DEPRESSION and ABUSE AND MISUSE. Jazz Pharmaceuticals, Inc; 2021.
Rodriguez CL, Foldvary-Schaefer N. Clinical neurophysiology of NREM parasomnias. Handb Clin Neurol. 2019;161:397–410.
Mainieri G, Loddo G, Castelnovo A, Balella G, Cilea R, Mondini S, et al. EEG activation does not differ in simple and complex episodes of disorders of arousal: a spectral analysis study. Nat Sci Sleep. 2022;14:1097–111.
•• Lopez R, Shen Y, Chenini S, Rassu AL, Evangelista E, Barateau L, et al. Diagnostic criteria for disorders of arousal: a video-polysomnographic assessment. Ann Neurol. 2018;83(2):341–51. This study describes that frequent slow/mixed arousals in SWS and complex behaviors during vPSG are strongly associated with DOAs.
Mutti C, Bernabè G, Barozzi N, Ciliento R, Trippi I, Pedrazzi G, et al. Commonalities and differences in NREM parasomnias and sleep-related epilepsy: is there a continuum between the two conditions? Front Neurol. 2020;11: 600026.
Guilleminault C, Kirisoglu C, da Rosa AC, Lopes C, Chan A. Sleepwalking, a disorder of NREM sleep instability. Sleep Med. 2006;7(2):163–70.
Zucconi M, Oldani A, Ferini-Strambi L, Smirne S. Arousal fluctuations in non-rapid eye movement parasomnias: the role of cyclic alternating pattern as a measure of sleep instability. J Clin Neurophysiol. 1995;12(2):147–54.
Kokkinos V, Vulliémoz S, Koupparis AM, Koutroumanidis M, Kostopoulos GK, Lemieux L, et al. A hemodynamic network involving the insula, the cingulate, and the basal forebrain correlates with EEG synchronization phases of sleep instability. Sleep. 2019;42(4):zsy259.
Schenck CH, Bundlie SR, Ettinger MG, Mahowald MW. Chronic behavioral disorders of human REM sleep: a new category of parasomnia. Sleep. 1986;9(2):293–308.
Howell MJ. Rapid eye movement sleep behavior disorder and other rapid eye movement parasomnias. Continuum (Minneap Minn). 2020;26(4):929–45.
Williams SR, Henzler N, Peřinová P, Morrison IA, Ellis JG, Riha RL. Trauma immediately preceding REM-behavior disorder: a valuable prognostic marker? Front Neurol. 2021;12: 710584.
Dauvilliers Y, Schenck CH, Postuma RB, Iranzo A, Luppi PH, Plazzi G, et al. REM sleep behaviour disorder. Nat Rev Dis Primers. 2018;4(1):19.
Antelmi E, Lippolis M, Biscarini F, Tinazzi M, Plazzi G. REM sleep behavior disorder: mimics and variants. Sleep Med Rev. 2021;60: 101515.
Chiaro G, Calandra-Buonaura G, Cecere A, Mignani F, Sambati L, Loddo G, et al. REM sleep behavior disorder, autonomic dysfunction and synuclein-related neurodegeneration: where do we stand? Clin Auton Res. 2018;28(6):519–33.
Högl B, Stefani A. REM sleep behavior disorder (RBD): Update on diagnosis and treatment. Somnologie (Berl). 2017;21(Suppl 1):1–8.
Frauscher B, Gschliesser V, Brandauer E, Ulmer H, Peralta CM, Müller J, et al. Video analysis of motor events in REM sleep behavior disorder. Mov Disord. 2007;22(10):1464–70.
•• Lapierre O, Montplaisir J. Polysomnographic features of REM sleep behavior disorder: development of a scoring method. Neurology. 1992;42(7):1371–4. This study describes a scoring method for RBD.
Berry RB, Quan SF, Abreu AR, Bibbs ML, DelRosso L, Harding SM, Mao M-M, Plante DT, Pressman MR, Troester MR; et al. The AASM manual for the scoring of sleep and associated events: rules, terminology and technical specifications, Version 2.6. Darien,IL, USA: American Academy of Sleep Medicine; 2020.
•• Frauscher B, Iranzo A, Gaig C, Gschliesser V, Guaita M, Raffelseder V, et al. Normative EMG Values during REM Sleep for the Diagnosis of REM Sleep Behavior Disorder. Sleep. 2012;35(6):835–47. This study describes the normative EMG values for RBD.
Zhang Y, Ren R, Yang L, Sanford LD, Tang X. Polysomnographically measured sleep changes in idiopathic REM sleep behavior disorder: a systematic review and meta-analysis. Sleep Med Rev. 2020;54: 101362.
Miglis MG, Adler CH, Antelmi E, Arnaldi D, Baldelli L, Boeve BF, et al. Biomarkers of conversion to α-synucleinopathy in isolated rapid-eye-movement sleep behaviour disorder. Lancet Neurol. 2021;20(8):671–84.
Iranzo A, Fernández-Arcos A, Tolosa E, Serradell M, Molinuevo JL, Valldeoriola F, et al. Neurodegenerative disorder risk in idiopathic REM sleep behavior disorder: study in 174 patients. PLoS ONE. 2014;9(2): e89741.
• Postuma RB, Iranzo A, Hu M, Högl B, Boeve BF, Manni R, et al. Risk and predictors of dementia and parkinsonism in idiopathic REM sleep behaviour disorder: a multicentre study. Brain. 2019;142(3):744–59. This multicentre study documents the high phenoconversion rate from iRBD to an overt neurodegenerative syndrome.
Feinstein MA, Sharp RR, Sandness DJ, Feemster JC, Junna M, Kotagal S, et al. Physician and patient determinants of prognostic counseling in idiopathic REM sleep-behavior disorder. Sleep Med. 2019;62:80–5.
Aurora RN, Zak RS, Maganti RK, Auerbach SH, Casey KR, Chowdhuri S, et al. Best practice guide for the treatment of REM sleep behavior disorder (RBD). J Clin Sleep Med. 2010;6(1):85–95.
Li SX, Lam SP, Zhang J, Yu MWM, Chan JWY, Liu Y, et al. A prospective, naturalistic follow-up study of treatment outcomes with clonazepam in rapid eye movement sleep behavior disorder. Sleep Med. 2016;21:114–20.
Kunz D, Stotz S, Bes F. Treatment of isolated REM sleep behavior disorder using melatonin as a chronobiotic. J Pineal Res. 2021;71(2): e12759.
Jun J, Kim R, Byun J, Kim T, Lim J, Sunwoo J, et al. Prolonged–release melatonin in patients with idiopathic REM sleep behavior disorder. Ann Clin Transl Neurol. 2019;6(4):716–22.
Kunz D, Mahlberg R. A two-part, double-blind, placebo-controlled trial of exogenous melatonin in REM sleep behaviour disorder. J Sleep Res. 2010;19(4):591–6.
Besag FMC, Vasey MJ, Lao KSJ, Wong ICK. Adverse events associated with melatonin for the treatment of primary or secondary sleep disorders: a systematic review. CNS Drugs. 2019;33(12):1167–86.
[Internet]. 2022 [cited 21 June 2022]. Available from: https://www.merriam-webster.com/dictionary/stereotypy. In.
Halász P, Kelemen A, Szűcs A. Physiopathogenetic Interrelationship between nocturnal frontal lobe epilepsy and NREM arousal parasomnias. Epilepsy Res Treat. 2012;2012: 312693.
Herman ST, Walczak TS, Bazil CW. Distribution of partial seizures during the sleep–wake cycle: differences by seizure onset site. Neurology. 2001;56(11):1453–9.
Frauscher B, Gotman J. Sleep, oscillations, interictal discharges, and seizures in human focal epilepsy. Neurobiol Dis. 2019;127:545–53.
Bisulli F, Vignatelli L, Naldi I, Pittau F, Provini F, Plazzi G, et al. Diagnostic accuracy of a structured interview for nocturnal frontal lobe epilepsy (SINFLE): a proposal for developing diagnostic criteria. Sleep Med. 2012;13(1):81–7.
Derry CP, Harvey AS, Walker MC, Duncan JS, Berkovic SF. NREM arousal parasomnias and their distinction from nocturnal frontal lobe epilepsy: a video EEG analysis. Sleep. 2009;32(12):1637–44.
Zadra A, Pilon M, Montplaisir J. Polysomnographic diagnosis of sleepwalking: effects of sleep deprivation. Ann Neurol. 2008;63(4):513–9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical collection on Sleep and Neurological Conditions
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Mora-Munoz, L., Alsheikhtaha, Z. & Foldvary-Schaefer, N. Differential Diagnosis of Complex Nocturnal Behaviors. Curr Sleep Medicine Rep 8, 74–85 (2022). https://doi.org/10.1007/s40675-022-00238-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40675-022-00238-1