Abstract
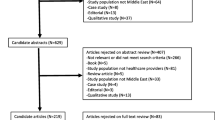
Individuals who provide services for people living with HIV (PLWH) face numerous work-related challenges, including psychosocial and structural factors affecting the quality of care that they provide. Little is known about the factors that relate to burnout among service providers for PLWH. The current study seeks to examine the factors associated with burnout and the role of resilience and coping in the context of burnout. Via convenience sampling, data was collected from 28 professionals (e.g., peer counselors, HIV testers, case managers/case workers, group facilitators, or social workers) serving PLWH in the USA. Participants completed quantitative measures on sociodemographics, organizational factors, discrimination, trauma, depression, and burnout. A sub-sample of 19 participants provided in-depth qualitative data via semi-structured interviews on burnout, coping, and resilience as a buffer against the effects of burnout. Thematic content analysis revealed themes on the factors related to burnout (e.g., discrimination, limited financial and housing resources, and COVID-19), rejuvenating factors, coping with burnout, and intervention strategies. Additionally, Pearson’s product moment correlations revealed significant associations between mental health variables such as depressive and posttraumatic stress disorder symptomology with (a) discrimination and microaggressions and (b) burnout. The current study highlights challenges to providing HIV care, including structural barriers and discrimination that are doubly impactful to the professionals in this sample who share identities with the PLWH whom they serve. These findings may inform the development of an intervention targeting burnout among individuals providing services to PLWH and motivate change to remove structural barriers and improve quality of care for PLWH.

Similar content being viewed by others
Data Availability
Data supporting the findings of this study are unavailable due to ongoing work. Please contact the corresponding author [SD] with queries.
References
World Health Organization. World Health Organization. World Health Organization; 2020 [cited 2020 Jun 17]. Global Health Observatory (GHO) Data. http://www.who.int/gho/hiv/en/.
Centers for Disease Control and Prevention. Estimated HIV incidence and prevalence in the United States, 2014–2018. HIV Surveill Suppl Rep. 2020 May [cited 2020 Jul 14];25(1). Retrieved July 7, 2023, from http://www.cdc.gov/hiv/library/reports/hiv-surveillance.html.
Newman CE, de Wit JBF, Crooks L, Reynolds RH, Canavan PG, Kidd MR. Challenges of providing HIV care in general practice. Aust J Prim Health. 2015;21(2):164–8.
Centers for Disease Control and Prevention. Retention in Care | Treatment, Care, and Prevention for People with HIV | Clinicians | HIV | CDC. 2019 [cited 2020 Jun 1]. Retrieved July 7, 2023, from https://www.cdc.gov/hiv/clinicians/treatment/care-retention.html.
Bonney LE, Del Rio C. Challenges facing the US HIV/AIDS medical care system. Future HIV Ther. 2008;2(2):99–104.
Dombrowski JC, Simoni JM, Katz DA, Golden MR. Barriers to HIV care and treatment among participants in a public health HIV care relinkage program. AIDS Patient Care STDs. 2015;29(5):279–87.
Krawczyk CS, Funkhouser E, Kilby JM, Vermund SH. Delayed access to HIV diagnosis and care: special concerns for the Southern United States. AIDS Care. 2006;18(sup1):35–44.
Stevens PE, Keigher SM. Systemic barriers to health care access for U.S. women with HIV: the role of cost and insurance. Int J Health Serv. 2009;39(2):225–43.
Grant JM, Motter LA, Tanis J. Injustice at every turn: a report of the National Transgender Discrimination Survey. 2011 [cited 2020 Jun 9]. Retrieved July 7, 2023, from http://dataspace.princeton.edu/jspui/handle/88435/dsp014j03d232p.
Meyers T, Moultrie H, Naidoo K, Cotton M, Eley B, Sherman G. Challenges to pediatric HIV care and treatment in South Africa. J Infect Dis. 2007;196(Supplement_3):S474-81.
Machtinger E, Wilson T, Haberer J, Weis D. Psychological trauma and PTSD in HIV-positive women: a meta-analysis. - PubMed - NCBI. AIDS Behav. 2012;16(8):2091–100.
Pence BW. The impact of mental health and traumatic life experiences on antiretroviral treatment outcomes for people living with HIV/AIDS. J Antimicrob Chemother. 2009;63(4):636–40.
Denning P, DiNenno E. Economically disadvantaged. 2018 [cited 2020 Jun 9]. Retrieved July 7, 2023, from https://www.cdc.gov/hiv/group/poverty.html.
Riley ED, Gandhi M, Bradley Hare C, Cohen J, Hwang SW. Poverty, unstable housing, and HIV infection among women living in the United States. Curr HIV/AIDS Rep. 2007;4(4):181–6.
Aidala AA, Wilson MG, Shubert V, Gogolishvili D, Globerman J, Rueda S, et al. Housing status, medical care, and health outcomes among people living with HIV/AIDS: a systematic review. Am J Public Health. 2016;106(1):e1-23.
Ha PN, Chuc NTK, Hien HT, Larsson M, Pharris A. HIV-related stigma: impact on healthcare workers in Vietnam. Glob Public Health. 2013;8(Suppl 1):S61-74.
Makhado L, Davhana-Maselesele M. Knowledge and psychosocial wellbeing of nurses caring for people living with HIV/AIDS (PLWH). Health SA Gesondheid. 2016;21:1–10.
Moradi G, Mohraz M, Gouya MM, Dejman M, Alinaghi SS, Rahmani K, et al. Problems of providing services to people affected by HIV/AIDS: service providers and recipients perspectives. East Mediterr Health J Rev Sante Mediterr Orient Al-Majallah Al-Sihhiyah Li-Sharq Al-Mutawassit. 2015;21(1):20–8.
Maslach C, Jackson S, Leiter M. The Maslach burnout inventory manual (4th ed). 1997; Mountain View, CA: CPP, Inc.
Mala R, Santhosh K, Anshul A, Aarthy R. Ethics in human resource management: potential for burnout among healthcare workers in ART and community care centres | Indian Journal of Medical Ethics. Indian J Med Ethics. 2010 [cited 2020 May 25];7(3). Retrieved July 7, 2023, from http://ijme.in/articles/ethics-in-human-resource-management-potential-for-burnout-among-healthcare-workers-in-art-and-community-care-centres/?galley=html.
O’Connor K, Neff DM, Pitman S. Burnout in mental health professionals: a systematic review and meta-analysis of prevalence and determinants. Eur Psychiatry. 2018;53:74–99.
Paris M Jr, Hoge MA. Burnout in the mental health workforce: a review. J Behav Health Serv Res. 2010;37(4):519–28.
Bhembe LQ, Tsai FJ. Occupational stress and burnout among health care workers caring for people living with HIV in Eswatini. J Assoc Nurses AIDS Care JANAC. 2019;30(6):639–47.
Hussein S. Work engagement, burnout and personal accomplishments among social workers: a comparison between those working in children and adults’ services in England. Adm Policy Ment Health Ment Health Serv Res. 2018;45(6):911–23.
Tantchou J. Poor working conditions, HIV/AIDS and burnout: a study in Cameroon. Anthropol Action [Internet]. 2014 [cited 2019 Dec 1];21(3). Retrieved July 7, 2023, from http://berghahnjournals.com/view/journals/aia/21/3/aia210305.xml.
Ntshwarang PN, Malinga-Musamba T. Social workers working with HIV and aids in health care settings: a case study of Botswana. Practice. 2012;24(5):287–98.
Shelton RC, Golin CE, Smith SR, Eng E, Kaplan A. Role of the HIV/AIDS case manager: analysis of a case management adherence training and coordination program in North Carolina. AIDS Patient Care STDs. 2006;20(3):193–204.
Rios-Ellis B, Becker D, Espinoza L, Nguyen-Rodriguez S, Diaz G, Carricchi A, et al. Evaluation of a community health worker intervention to reduce HIV/AIDS stigma and increase HIV testing among underserved Latinos in the Southwestern US. Public Health Rep Wash DC 1974. 2015;130(5):458–67.
Spach D. HIV in racial and ethnic minority polpulations. 2020 [cited 2020 Jun 6]. Retrieved July 7, 2023, from https://www.hiv.uw.edu/go/key-populations/minority-populations/core-concept/all.
Koutsimani P, Montgomery A, Georganta K. The relationship between burnout, depression, and anxiety: a systematic review and meta-analysis. Front Psychol. 2019;10:284. https://doi.org/10.3389/fpsyg.2019.00284/full.
Cohen M, Fabri M, Cai X, Shi Q, Hoover D, Binagwaho A, et al. Prevalence and predictors of posttraumatic stress disorder and depression in HIV-infected and at-risk Rwandan women | Journal of Women’s Health. J Womens Health. 2009;18(11):1783–91.
Tan G, Teo I, Srivastava D, Smith D, Smith SL, Williams W, et al. Improving access to care for women veterans suffering from chronic pain and depression associated with trauma. Pain Med. 2013;14(7):1010–20.
Bhatia MS, Munjal S. Prevalence of depression in people living with HIV/AIDS undergoing ART and factors associated with it. J Clin Diagn Res JCDR. 2014;8(10):WC01-4.
O’Cleirigh C, Magidson JF, Skeer MR, Mayer KH, Safren SA. Prevalence of psychiatric and substance abuse symptomatology among HIV-infected gay and bisexual men in HIV primary care. Psychosomatics. 2015;56(5):470–8.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders (5th ed). Arlington, VA: Author; 2013. https://doi.org/10.1176/appi.books.9780890425596.
van der Merwe A, Hunt X. Secondary trauma among trauma researchers: lessons from the field. Psychol Trauma Theory Res Pract Policy. 2019;11(1):10–8.
Mall S, Sorsdahl K, Swartz L, Joska J. “I understand just a little…” perspectives of HIV/AIDS service providers in South Africa of providing mental health care for people living with HIV/AIDS. AIDS Care. 2012;24(3):319–23.
Benevides-Pereira AMT, Das-Neves-Alves R. A study on burnout syndrome in healthcare providers to people living with HIV. AIDS Care. 2007;19(4):565–71.
Ginossar T, Oetzel J, Hill R, Avila M, Archiopoli A, Wilcox B. HIV health-care providers’ burnout: can organizational culture make a difference? AIDS Care. 2014;26(12):1605–8.
Nie Z, Jin Y, He L, Chen Y, Ren X, Yu J, et al. Correlation of burnout with social support in hospital nurses. Int J Clin Exp Med. 2015;8(10):19144–9.
Shoptaw S, Stein JA, Rawson RA. Burnout in substance abuse counselors: impact of environment, attitudes, and clients with HIV. J Subst Abuse Treat. 2000;19(2):117–26.
Raviola G, Machoki M, Mwaikambo E, Good MJD. HIV, disease plague, demoralization and “burnout”: resident experience of the medical profession in Nairobi. Kenya Cult Med Psychiatry. 2002;26(1):55–86.
Schuster RC, McMahon DE, Young SL. A comprehensive review of the barriers and promoters health workers experience in delivering prevention of vertical transmission of HIV services in sub-Saharan Africa. AIDS Care. 2016;28(6):778–94.
Peltzer K, Matseke G, Louw J. Secondary trauma and job burnout and associated factors among HIV lay counsellors in Nkangala district, South Africa. Br J Guid Couns. 2013;42(4):410–22. https://doi.org/10.1080/03069885.2013.835788.
Rowan D, Lynch S, Randall E, Johnson H. Deconstructing burnout in HIV service providers. J HIVAIDS Soc Serv. 2015;14(1):58–73.
Sales JM, Piper K, Riddick C, Getachew B, Colasanti J, Kalokhe A. Low provider and staff self-care in a large safety-net HIV clinic in the Southern United States: implications for the adoption of trauma-informed care. SAGE Open Med. 2019;7:2050312119871417.
Stockton R, Tebatso P, Morran DK, Yebei P, Chang SH, Voils-Levenda A. A survey of HIV/AIDS counselors in Botswana: satisfaction with training and supervision, self-perceived effectiveness and reactions to counseling HIV-positive clients. J HIVAIDS Soc Serv. 2012;11(4):424–46.
Molina Y, Dirkes J, Ramirez-Valles J. Burnout in HIV/AIDS volunteers: a socio-cultural analysis among Latino gay, bisexual men, and transgender people. Nonprofit Volunt Sect Q. 2017;46(6):1231–49.
Wells EM. Examining perceived racial microaggressions and burnout in helping profession graduate students of color. 2009 Aug [cited 2020 Jul 22]. Retrieved July 7, 2023, from http://athenaeum.libs.uga.edu/handle/10724/25971.
Roomaney R, Steenkamp J, Kagee A. Predictors of burnout among HIV nurses in the Western Cape. Curationis. 2017;40(1):1–9.
Robinson A. Guest opinion: HIV response fails black GBTs. The Bay Area Reporter. 2018 [cited 2020 Jul 22]. Retrieved July 7, 2023, from https://www.ebar.com/news/news//268807.
Kim MH, Mazenga AC, Simon K, Yu X, Ahmed S, Nyasulu P, et al. Burnout and self-reported suboptimal patient care amongst health care workers providing HIV care in Malawi. PLoS ONE. 2018;13(2):e0192983.
Salvagioni DAJ, Melanda FN, Mesas AE, González AD, Gabani FL, de Andrade SM. Physical, psychological and occupational consequences of job burnout: a systematic review of prospective studies. PLoS ONE. 2017 [cited 2020 May 31];12(10). Retrieved July 7, 2023, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5627926/.
Centers for Disease Control and Prevention. HIV surveillance report, 2019. 2021. Report No.: 32. http://www.cdc.gov/hiv/library/reports/hiv-surveillance.html. Accessed 7 Jul 2023.
Gueritault-Chalvin V, Kalichman SC, Demi A, Peterson JL. Work-related stress and occupational burnout in AIDS caregivers: test of a coping model with nurses providing AIDS care. AIDS Care. 2000;12(2):149–61.
Visser M, Mabota P. The emotional wellbeing of lay HIV counselling and testing counsellors. Afr J AIDS Res. 2015;14(2):169–77. https://doi.org/10.2989/16085906.2015.1040812.
Moremi M. Volunteer stress and coping in HIV and AIDS home-based care [Diss.]. University of South Africa; 2012. Retrieved July 7, 2023, from https://pdfs.semanticscholar.org/c02b/3e7ec8698af96de0525cb8227b3d5196c2c7.pdf.
Arrogante O, Aparicio-Zaldivar E. Burnout and health among critical care professionals: the mediational role of resilience. Intensive Crit Care Nurs. 2017;42:110–5.
Chen F, Curran PJ, Bollen KA, Kirby J, Paxton P. An empirical evaluation of the use of fixed cutoff points in RMSEA test statistic in structural equation models. Sociol Methods Res. 2008;36(4):462–94.
Sheykhshabani EH, Karimi R, Beshlideh K. The effect of authentic leadership on burnout with mediating areas of worklife and occupational coping self-efficacy. J Psychol. 2019;23(2):166–80.
Harker R, Pidgeon A, Klaassen F, King S. Exploring resilience and mindfulness as preventative factors for psychological distress burnout and secondary traumatic stress among human service professionals. Work Read Mass. 2016;54(3):631–7.
Fortney L, Luchterhand C, Zakletskaia L, Zgierska A, Rakel D. Abbreviated mindfulness intervention for job satisfaction, quality of life, and compassion in primary care clinicians: a pilot study. Ann Fam Med. 2013;11(5):412–20.
Dyrbye L, Power D, Massie F, Eaker A, Harper W. Factors associated with resilience to and recovery from burnout: a prospective, multi-institutional study of US medical students. Med Educ. 2010;44(10):1016–26. https://doi.org/10.1111/j.1365-2923.2010.03754.x.
Edmonds C, Lockwood GM, Bezjak A, Nyhof-Young J. Alleviating emotional exhaustion in oncology nurses: an evaluation of Wellspring’s “Care for the Professional Caregiver Program.” J Cancer Educ Off J Am Assoc Cancer Educ. 2012;27(1):27–36.
Johnson SM, Naidoo AV. Transpersonal practices as prevention intervention for burnout among HIV/AIDS coordinator teachers. South Afr J Psychol. 2013;43(1):59–70.
Morrison Wylde C, Mahrer NE, Meyer RML, Gold JI. Mindfulness for novice pediatric nurses: smartphone application versus traditional intervention. J Pediatr Nurs. 2017;36:205–12.
Creswell J, Plano CV. Designing and conducting mixed methods research. 2nd ed. Thousand Oaks, California: Sage Publications, Inc; 2011.
Castleberry A. NVivo 10 [software program]. Version 10. QSR International; 2012. Am J Pharm Educ. 2014 [cited 2020 May 26];78(1). Retrieved July 7, 2023, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3930250/.
Spector PE, Jex SM. J Occup Health Psychol. 1998;3(4):356–67.
Williams DR, Yu Y, Jackson JS, Anderson NB. Racial differences in physical and mental health: socio-economic status, stress and discrimination. J Health Psychol. 1997;2(3):335–51.
Torres-Harding SR, Andrade AL Jr, Romero Diaz CE. The Racial Microaggressions Scale (RMAS): a new scale to measure experiences of racial microaggressions in people of color. Cultur Divers Ethnic Minor Psychol. 2012;18(2):153–64.
Nadal KL, Whitman CN, Davis LS, Erazo T, Davidoff KC. Microaggressions toward lesbian, gay, bisexual, transgender, queer, and genderqueer people: a review of the literature. J Sex Res. 2016;53(4–5):488–508.
Eaton LA, Allen A, Maksut JL, Earnshaw V, Watson RJ, Kalichman SC. HIV microaggressions: a novel measure of stigma-related experiences among people living with HIV. J Behav Med. 2020;43(1):34–43.
Weathers FW, Litz BT, Keane TM, Palmieri PA, Marx BP, Schnurr PP. The PTSD Checklist for DSM-5 (PCL-5). 2013 [cited 2018 Dec 21]. Retrieved July 7, 2023, from https://www.ptsd.va.gov/professional/assessment/adult-sr/ptsd-checklist.asp.
Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1(3):385–401.
Campbell-Sills L, Stein MB. Psychometric analysis and refinement of the Connor-davidson Resilience Scale (CD-RISC): validation of a 10-item measure of resilience. J Trauma Stress. 2007;20(6):1019–28.
Zimet G, Dahlem N, Zimet S, Farley G. The multidimensional scale of perceived social support. J Pers Assess. 1988;52(1):30–41.
Carver CS. You want to measure coping but your protocol’s too long: consider the brief COPE. Int J Behav Med. 1997;4(1):92–100.
Schwarzer R, Jerusalem M. General Self-Efficacy Scale (GSE). In: Weinman J, Wright S, Johnston M, Measures in health psychology: a user’s portfolio. Causal and control beliefs. Windsor, England: NFER-NELSON. 1995 [cited 2018 Dec 21]; 35–7. Retrieved July 7, 2023, from http://www.midss.ie/content/general-self-efficacy-scale-gse.
Do AN, Rosenberg ES, Sullivan PS, Beer L, Strine TW, Schulden JD, et al. Excess burden of depression among HIV-infected persons receiving medical care in the united states: data from the medical monitoring project and the behavioral risk factor surveillance system. PLoS ONE. 2014;9(3):e92842.
Woodford MR, Weber G, Nicolazzo Z, Hunt R, Kulick A, Coleman T, et al. Depression and attempted suicide among LGBTQ college students: fostering resilience to the effects of heterosexism and cisgenderism on campus. J Coll Stud Dev. 2018;59(4):421–38.
Dale SK, Nelson CM, Wright IA, Etienne K, Lazarus K, Gardner N et al. Structural equation model of intersectional microaggressions, discrimination, resilience, and mental health among black women with hiv. Health psychology. 2023 May;42(5):299.
Acknowledgements
The co-authors would like to express gratitude to the participants who gave their time and energy to participate in this study—without them, this research study would not exist. Thank you as well to the community stakeholders who played a key role in the recruitment, referrals, and engagement of women. I would also like to thank the Strengthening Health through INovation and Engagement (SHINE) research staff and volunteers who helped to facilitate the collection and analysis of this data. We express gratitude to the first author’s thesis committee—Dr. Deborah Jones-Weiss, Dr. Steven Safren, and Dr. Sannisha Dale (thesis chair and senior author)—who provided support, resources, feedback, and guidance from conceptualization to data analysis and interpretation.
Funding
This research was funded by Dr. Sannisha Dale’s start-up award from the University of Miami. Dr. Sannisha Dale was additionally funded by R56MH121194 and R01MH121194 from the National Institute of Mental Health.
Author information
Authors and Affiliations
Contributions
Rachelle Reid and Sannisha Dale contributed to the study conception and design. Material preparation and data collection were performed by Rachelle Reid. Interview transcription and coding were performed by Rachelle Reid, Aarti Madhu, Stephanie Gonzalez, Hannah Crosby, and Michelle Stjuste. The first draft of the manuscript was written by Rachelle Reid with iterative feedback and edits by Sannisha Dale. Thereafter, all authors commented on versions of the manuscript and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics Approval
This study was performed in accordance with the principles of the Declaration of Helsinki All study procedures and materials were approved by the Institutional review Board at the University of Miami (11/6/2020, No. 20201279).
Consent to Participate
Informed consent was obtained from all individual participants included in the study.
Consent for Publication
Research participants have provided informed consent for the publication of the research findings in a peer-reviewed journal.
Competing Interests
Unrelated to the data in this manuscript, Dr. Dale is a co-investigator on a Merck & Co. funded project on “A Qualitative Study to Explore Biomedical HIV Prevention Preferences, Challenges and Facilitators among Diverse At-Risk Women Living in the United States” and has served as a workgroup consultant on engaging people living with HIV for Gilead Sciences, Inc. All other authors declare that they do not have relevant financial, non-financial interests nor competing interests to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Reid, R., Madhu, A., Gonzalez, S. et al. Burnout Among Service Providers for People Living with HIV: Factors Related to Coping and Resilience. J. Racial and Ethnic Health Disparities (2023). https://doi.org/10.1007/s40615-023-01784-2
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40615-023-01784-2