Abstract
Background
The association between frailty and cerebral small vessel disease (CSVD) remains controversial due to the use of different methods to assess frailty, including physical frailty phenotype and frailty scores containing measures of cognition. A frailty index based on laboratory tests (FI-Lab), which assesses frailty by the combination of routine laboratory measures and several vital signs, is independent of cognition and function status. We aimed to evaluate the association of FI-Lab with CSVD.
Methods
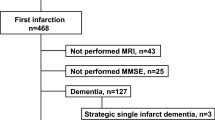
An observational study was carried out in a hospitalized cohort of older patients with minor ischemic stroke or TIA. The FI-Lab was constructed by 20 routine laboratory tests, plus systolic blood pressure, diastolic blood pressure, and pulse pressure. Manifestations of CSVD including white matter hyperintensity (WMH), silent lacunar infarcts, microbleed, enlarged perivascular spaces (EPVS), as well as deep brain atrophy, were measured on magnetic resonance imaging (MRI). An ordinal score system constructed by WMH, EPVS, silent lacunar infarcts, and microbleed was used to reflect the total burden of CSVD. The associations between FI-lab and CSVD were examined by logistic regression analysis and ordinal regression.
Results
A total of 398 patients were recruited from January 2016 to December 2018. The mean FI-Lab value was 0.26 ± 0.11. The prevalence of extensive periventricular WMH, extensive deep WMH, extensive basal ganglia EPVS, extensive centrum semiovale EPVS, silent lacunar infarcts, and deep microbleed was 26.1, 66.6, 68.6, 80.7, 32.9, and 6.5%, respectively. A higher FI-Lab value was associated with increased risks of extensive deep WMH (OR = 1.622; 95% CI, 1.253 ~ 2.100), extensive basal ganglia EPVS (OR = 1.535; 95% CI, 1.187 ~ 1.985), extensive centrum semiovale EPVS (OR = 1.584; 95% CI, 1.167 ~ 2.151), silent lacunar infarcts (OR = 1.273; 95% CI, 1.007 ~ 1.608), and higher total burden of CSVD. These associations remained after the adjustment of potential confounding factors.
Conclusion
This study demonstrated that a higher FI-Lab score might be associated with the presence of WMH, EPVS, silent lacunar infarcts, as well as severe total CSVD burden in older patients with minor stroke or TIA. The FI-Lab provides a basis for the prediction of CSVD.



Similar content being viewed by others
References
Wardlaw JM, Smith C, Dichgans M (2019) Small vessel disease: mechanisms and clinical implications. Lancet Neurol 18:684–696. https://doi.org/10.1016/s1474-4422(19)30079-1
Wardlaw JM, Smith EE, Biessels GJ et al (2013) Neuroimaging standards for research into small vessel disease and its contribution to ageing and neurodegeneration. Lancet Neurol 12:822–838. https://doi.org/10.1016/S1474-4422(13)70124-8
Lee J-H, Oh E, Oh MS et al (2014) Highly variable blood pressure as a predictor of poor cognitive outcome in patients with acute lacunar infarction. Cogn Behav Neurol 27:198. https://doi.org/10.1097/WNN.0000000000000040
Kesav P, Menon D, Vysakha KV et al (2020) Differential distribution of cerebral microbleeds in subtypes of acute ischemic minor stroke and TIA as well as its association with vascular risk factors. Neurol India 68:1139–1143. https://doi.org/10.4103/0028-3886.299147
van Dijk EJ, Prins ND, Vrooman HA et al (2008) Progression of cerebral small vessel disease in relation to risk factors and cognitive consequences: Rotterdam scan study. Stroke 39:2712–2719. https://doi.org/10.1161/STROKEAHA.107.513176
Litak J, Mazurek M, Kulesza B et al (2020) Cerebral small vessel disease. Int J Mol Sci. https://doi.org/10.3390/ijms21249729
Ter Telgte A, van Leijsen EMC, Wiegertjes K et al (2018) Cerebral small vessel disease: from a focal to a global perspective. Nat Rev Neurol 14:387–398. https://doi.org/10.1038/s41582-018-0014-y
Saito T, Kawamura Y, Tanabe Y et al (2014) Cerebral microbleeds and asymptomatic cerebral infarctions in patients with atrial fibrillation. J Stroke Cerebrovasc Dis 23:1616–1622. https://doi.org/10.1016/j.jstrokecerebrovasdis.2014.01.005
Ma T, Cai J, Zhu YS et al (2018) Association between a frailty index based on common laboratory tests and QTc prolongation in older adults: the Rugao longevity and ageing study. Clin Interv Aging 13:797–804. https://doi.org/10.2147/CIA.S149791
Howlett SE, Rockwood MR, Mitnitski A et al (2014) Standard laboratory tests to identify older adults at increased risk of death. BMC Med 12:171. https://doi.org/10.1186/s12916-014-0171-9
Moroni F, Ammirati E, Rocca MA et al (2018) Cardiovascular disease and brain health: focus on white matter hyperintensities. Int J Cardiol Heart Vasc 19:63–69. https://doi.org/10.1016/j.ijcha.2018.04.006
Fazekas F, Kleinert R, Offenbacher H et al (1993) Pathologic correlates of incidental MRI white matter signal hyperintensities. Neurology 43:1683–1689. https://doi.org/10.1212/wnl.43.9.1683
Greenberg SM, Vernooij MW, Cordonnier C et al (2009) Cerebral microbleeds: a guide to detection and interpretation. Lancet Neurol 8:165–174. https://doi.org/10.1016/S1474-4422(09)70013-4
Staals J, Makin SD, Doubal FN et al (2014) Stroke subtype, vascular risk factors, and total MRI brain small-vessel disease burden. Neurology 83:1228–1234. https://doi.org/10.1212/WNL.0000000000000837
Sato S, Delcourt C, Heeley E et al (2016) Significance of cerebral small-vessel disease in acute intracerebral hemorrhage. Stroke 47:701–707. https://doi.org/10.1161/STROKEAHA.115.012147
Rockwood K, Mitnitski A (2011) Frailty defined by deficit accumulation and geriatric medicine defined by frailty. Clin Geriatr Med 27:17–26. https://doi.org/10.1016/j.cger.2010.08.008
Yang Y, Lee LC (2010) Dynamics and heterogeneity in the process of human frailty and aging: evidence from the US older adult population. J Gerontol B Psychol Sci Soc Sci 65B:246–255. https://doi.org/10.1093/geronb/gbp102
Moon SY, de Souto Barreto P, Rolland Y et al (2018) Prospective associations between white matter hyperintensities and lower extremity function. Neurology 90:e1291–e1297. https://doi.org/10.1212/WNL.0000000000005289
Jordan LC, DeBaun MR (2018) Cerebral hemodynamic assessment and neuroimaging across the lifespan in sickle cell disease. J Cereb Blood Flow Metab 38:1438–1448. https://doi.org/10.1177/0271678X17701763
Anandh KR, Sujatha CM, Ramakrishnan S (2014) Atrophy analysis of corpus callosum in Alzheimer brain MR images using anisotropic diffusion filtering and level sets. Annu Int Conf IEEE Eng Med Biol Soc 2014:1945–1948. https://doi.org/10.1109/EMBC.2014.6943993
Solfrizzi V, Scafato E, Frisardi V et al (2013) Frailty syndrome and the risk of vascular dementia: the Italian longitudinal study on aging. Alzheimers Dement 9:113–122. https://doi.org/10.1016/j.jalz.2011.09.223
Ma Y, Song A, Viswanathan A et al (2020) Blood pressure variability and cerebral small vessel disease: a systematic review and meta-analysis of population-based cohorts. Stroke 51:82–89. https://doi.org/10.1161/STROKEAHA.119.026739
Kant IMJ, de Bresser J, van Montfort SJT et al (2017) MRI markers of neurodegenerative and neurovascular changes in relation to postoperative delirium and postoperative cognitive decline. Am J Geriatr Psychiatry 25:1048–1061. https://doi.org/10.1016/j.jagp.2017.06.016
Caplan LR (1995) Binswanger’s disease–revisited. Neurology 45:626–633. https://doi.org/10.1212/wnl.45.4.626
Buchman AS, Yu L, Wilson RS et al (2014) Brain pathology contributes to simultaneous change in physical frailty and cognition in old age. J Gerontol A Biol Sci Med Sci 69:1536–1544. https://doi.org/10.1093/gerona/glu117
Siejka TP, Srikanth VK, Hubbard RE et al (2018) Frailty and cerebral small vessel disease: a cross-sectional analysis of the Tasmanian study of cognition and gait (TASCOG). J Gerontol A Biol Sci Med Sci 73:255–260. https://doi.org/10.1093/gerona/glx145
Groeschel S, Chong WK, Surtees R et al (2006) Virchow-Robin spaces on magnetic resonance images: normative data, their dilatation, and a review of the literature. Neuroradiology 48:745–754. https://doi.org/10.1007/s00234-006-0112-1
Low A, Mak E, Rowe JB et al (2019) Inflammation and cerebral small vessel disease: a systematic review. Ageing Res Rev 53:100916. https://doi.org/10.1016/j.arr.2019.100916
Chung CP, Chou KH, Chen WT et al (2016) Cerebral microbleeds are associated with physical frailty: a community-based study. Neurobiol Aging 44:143–150. https://doi.org/10.1016/j.neurobiolaging.2016.04.025
Del Brutto OH, Mera RM, Ha JE et al (2016) Oily fish consumption is inversely correlated with cerebral microbleeds in community-dwelling older adults: results from the Atahualpa project. Aging Clin Exp Res 28:737–743. https://doi.org/10.1007/s40520-015-0473-6
Gregoire SM, Brown MM, Kallis C et al (2010) MRI detection of new microbleeds in patients with ischemic stroke: five-year cohort follow-up study. Stroke 41:184–186. https://doi.org/10.1161/STROKEAHA.109.568469
Lee SH, Lee ST, Kim BJ et al (2011) Dynamic temporal change of cerebral microbleeds: long-term follow-up MRI study. PLoS ONE 6:e25930. https://doi.org/10.1371/journal.pone.0025930
Klarenbeek P, van Oostenbrugge RJ, Rouhl RP et al (2013) Higher ambulatory blood pressure relates to new cerebral microbleeds: 2-year follow-up study in lacunar stroke patients. Stroke 44:978–983. https://doi.org/10.1161/STROKEAHA.111.676619
Xu X, Hilal S, Collinson SL et al (2015) Association of magnetic resonance imaging markers of cerebrovascular disease burden and cognition. Stroke 46:2808–2814. https://doi.org/10.1161/STROKEAHA.115.010700
Vinters HV (1987) Cerebral amyloid angiopathy. A critical review. Stroke 18:311–324. https://doi.org/10.1161/01.str.18.2.311
Iadecola C (2017) The neurovascular unit coming of age: a journey through neurovascular coupling in health and disease. Neuron 96:17–42. https://doi.org/10.1016/j.neuron.2017.07.030
Zhao J, Qu W, Zhou X et al (2021) Sleep quality mediates the association between cerebral small vessel disease burden and frailty: a community-based study. Front Aging Neurosci 13:751369. https://doi.org/10.3389/fnagi.2021.751369
Acknowledgements
This work was supported by the National Natural Science Foundation of China (Grant No. 81771286).
Funding
Foundation for Innovative Research Groups of the National Natural Science Foundation of China, No. 81771286, Xiaowei Lu.
Author information
Authors and Affiliations
Contributions
(I) Conception and design: XL; (II) Administrative support: XL; (III) Provision of study materials or patients: MD, YC, GC; (IV) Collection and assembly of data: MD, YC, QW; (V) Data analysis and interpretation: XL, GC, JZ, YZ; (VI) Manuscript writing: XL, JZ, MD; (VII) Final approval of manuscript: all authors.
Corresponding author
Ethics declarations
Conflict of interest
All the authors declare that there is no conflict of interest.
Ethical statement
The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted by the Declaration of Helsinki (as revised in 2013). This study protocol was approved by the Ethical Committee of the First Affiliated Hospital with Nanjing Medical University, and informed consent was obtained from all participants before the study.
Informed consent
Informed consent was obtained from all participants or their guardians before the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Dou, M., Cen, Y., Zhong, J. et al. Association between frailty index based on routine laboratory tests and risk of cerebral small vessel disease in elderly patients: a hospital-based observational study. Aging Clin Exp Res 34, 2683–2692 (2022). https://doi.org/10.1007/s40520-022-02207-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-022-02207-8