Abstract
Background
Frailty has been suggested as a possible risk factor for postoperative delirium (POD). However, results of previous studies were not consistent. We performed a meta-analysis of cohort study to evaluate the above association.
Methods
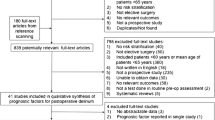
Relevant studies were obtained via systematic search of PubMed, Embase, SCOPUS, and Web of Science databases. Only studies with multivariate analysis were included. A random-effect model incorporating the potential heterogeneity was used to combine the results.
Results
Fifteen cohort studies including 3250 adult patients who underwent surgery were included, and the prevalence of frailty was 27.1% (880/3250) before surgeries. Overall, POD occurred in 513 patients (15.8%). Pooled results showed that frailty was associated with a higher risk of POD (adjusted odds ratio [OR]: 3.23, 95% confidence interval [CI]: 2.56–4.07, P < 0.001) without significant heterogeneity (P for Cochrane’s Q test = 0.25, I2 = 18%). Subgroup analyses showed a more remarkable association between frailty and POD in prospective cohort studies (OR: 3.64, 95% CI: 2.95–4.49, P < 0.001) than that in retrospective cohort studies (OR: 2.32, 95% CI: 1.60–3.35, P < 0.001; P for subgroup difference = 0.04). Moreover, the association was not affected by country of the study, age group of the patient, elective or emergency surgeries, cardiac and non-cardiac surgeries, evaluation instruments for frailty, diagnostic methods for POD, or quality score of the study (P for subgroup difference all > 0.05).
Conclusions
Frailty may be associated with a higher risk of POD in adult population.



Similar content being viewed by others
References
Rawle MJ, McCue L, Sampson EL et al (2021) Anticholinergic burden does not influence delirium subtype or the delirium-mortality association in hospitalized older adults: results from a prospective cohort study. Drugs Aging. https://doi.org/10.1007/s40266-020-00827-1
Dahlstrom EB, Han JH, Healy H et al (2020) Delirium prevention and treatment in the emergency department (ED): a systematic review protocol. BMJ Open 10:e037915. https://doi.org/10.1136/bmjopen-2020-037915
Oliveira JESL, Berning MJ, Stanich JA et al (2020) Risk factors for delirium among older adults in the emergency department: a systematic review protocol. BMJ Open 10:e039175. https://doi.org/10.1136/bmjopen-2020-039175
Abad-Gurumeta A, Casans-Frances R, Gomez-Rios MA (2020) Postoperative neurocognitive disorders: unknowns to solve and work to do. Minerva Anestesiol 86:908–909. https://doi.org/10.23736/S0375-9393.20.14796-5
Duning T, Ilting-Reuke K, Beckhuis M et al (2020) Postoperative delirium - treatment and prevention. Curr Opin Anaesthesiol. https://doi.org/10.1097/ACO.0000000000000939
Jin Z, Hu J, Ma D (2020) Postoperative delirium: perioperative assessment, risk reduction, and management. Br J Anaesth 125:492–504
Olotu C (2020) Postoperative neurocognitive disorders. Curr Opin Anaesthesiol 33:101–108. https://doi.org/10.1097/ACO.0000000000000812
Pagad S, Somagutta MR, May V et al (2020) Delirium in cardiac intensive care unit. Cureus 12:e10096. https://doi.org/10.7759/cureus.10096
Aitken SJ, Blyth FM, Naganathan V (2017) Incidence, prognostic factors and impact of postoperative delirium after major vascular surgery: a meta-analysis and systematic review. Vasc Med 22:387–397. https://doi.org/10.1177/1358863X17721639
Bai J, Liang Y, Zhang P et al (2020) Association between postoperative delirium and mortality in elderly patients undergoing hip fractures surgery: a meta-analysis. Osteoporos Int 31:317–326. https://doi.org/10.1007/s00198-019-05172-7
Shi Z, Mei X, Li C et al (2019) Postoperative delirium is associated with long-term decline in activities of daily living. Anesthesiology 131:492–500. https://doi.org/10.1097/ALN.0000000000002849
Park EA, Kim MY (2019) Postoperative delirium is associated with negative outcomes and long-term mortality in elderly Koreans: a retrospective observational study. Medicina (Kaunas) 55. https://doi.org/10.3390/medicina55100618
Chaiwat O, Chanidnuan M, Pancharoen W et al (2019) Postoperative delirium in critically ill surgical patients: incidence, risk factors, and predictive scores. BMC Anesthesiol 19:39. https://doi.org/10.1186/s12871-019-0694-x
McIsaac DI, MacDonald DB, Aucoin SD (2020) Frailty for perioperative clinicians: a narrative review. Anesth Analg 130:1450–1460. https://doi.org/10.1213/ANE.0000000000004602
Lauretani F, Longobucco Y, Ferrari Pellegrini F et al (2020) Comprehensive model for physical and cognitive frailty: current organization and unmet needs. Front Psychol 11:569629. https://doi.org/10.3389/fpsyg.2020.569629
Kojima G, Aoyama R, Taniguchi Y (2020) Associations between pet ownership and frailty: a systematic review. Geriatrics (Basel) 5. https://doi.org/10.3390/geriatrics5040089
Hewston P, Grenier A, Burke E et al (2020) Frailty and life-space mobility: implications for clinical practice and research. Occup Ther Health Care 1–9. https://doi.org/10.1080/07380577.2020.1846235
Sioutas G, Tsoulfas G (2020) Frailty assessment and postoperative outcomes among patients undergoing general surgery. Surgeon 18:e55–e66
Leung JM, Tsai TL, Sands LP (2011) Brief report: preoperative frailty in older surgical patients is associated with early postoperative delirium. Anesth Analg 112:1199–1201. https://doi.org/10.1213/ANE.0b013e31820c7c06
Jung P, Pereira MA, Hiebert B et al (2015) The impact of frailty on postoperative delirium in cardiac surgery patients. J Thorac Cardiovasc Surg 149:869–875 e861–862. https://doi.org/10.1016/j.jtcvs.2014.10.118
Brown CH, Max L, La Flam A et al (2016) The association between preoperative frailty and postoperative delirium after cardiac surgery. Anesth Analg 123:430-435. https://doi.org/10.1213/ANE.0000000000001271
Haugen CE, Mountford A, Warsame F et al (2018) Incidence, risk factors, and sequelae of post-kidney transplant delirium. J Am Soc Nephrol 29:1752–1759. https://doi.org/10.1681/ASN.2018010064
Nomura Y, Nakano M, Bush B et al (2019) Observational study examining the association of baseline frailty and postcardiac surgery delirium and cognitive change. Anesth Analg 129:507–514. https://doi.org/10.1213/ANE.0000000000003967
Saravana-Bawan B, Warkentin LM, Rucker D et al (2019) Incidence and predictors of postoperative delirium in the older acute care surgery population: a prospective study. Can J Surg 62:33–38. https://doi.org/10.1503/cjs.016817
Chen Y, Qin J (2020) Modified frailty index independently predicts postoperative delirium and delayed neurocognitive recovery after elective total joint arthroplasty. J Arthroplasty. https://doi.org/10.1016/j.arth.2020.07.074
Itagaki A, Sakurada K, Matsuhama M et al (2020) Impact of frailty and mild cognitive impairment on delirium after cardiac surgery in older patients. J Cardiol 76:147–153. https://doi.org/10.1016/j.jjcc.2020.02.007
Mahanna-Gabrielli E, Zhang K, Sieber FE et al (2020) Frailty is associated with postoperative delirium but not with postoperative cognitive decline in older noncardiac surgery patients. Anesth Analg 130:1516–1523. https://doi.org/10.1213/ANE.0000000000004773
Roopsawang I, Thompson H, Zaslavsky O et al (2020) Predicting hospital outcomes with the reported Edmonton frail scale-Thai version in orthopaedic older patients. J Clin Nurs 29:4708–4719. https://doi.org/10.1111/jocn.15512
Saljuqi AT, Hanna K, Asmar S et al (2020) Prospective evaluation of delirium in geriatric patients undergoing emergency general surgery. J Am Coll Surg 230:758–765. https://doi.org/10.1016/j.jamcollsurg.2020.01.029
Susano MJ, Grasfield RH, Friese M et al (2020) Brief preoperative screening for frailty and cognitive impairment predicts delirium after spine surgery. Anesthesiology 133:1184–1191. https://doi.org/10.1097/ALN.0000000000003523
Thillainadesan J, Mudge AM, Aitken SJ et al (2020) The prognostic performance of frailty for delirium and functional decline in vascular surgery patients. J Am Geriatr Soc. https://doi.org/10.1111/jgs.16907
Dasgupta M, Rolfson DB, Stolee P et al (2009) Frailty is associated with postoperative complications in older adults with medical problems. Arch Gerontol Geriatr 48:78–83. https://doi.org/10.1016/j.archger.2007.10.007
Pol RA, van Leeuwen BL, Visser L et al (2011) Standardised frailty indicator as predictor for postoperative delirium after vascular surgery: a prospective cohort study. Eur J Vasc Endovasc Surg 42:824–830. https://doi.org/10.1016/j.ejvs.2011.07.006
Schenning KJ, Deiner SG (2015) Postoperative delirium in the geriatric patient. Anesthesiol Clin 33:505–516. https://doi.org/10.1016/j.anclin.2015.05.007
Stroup DF, Berlin JA, Morton SC et al (2000) Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis of observational studies in epidemiology (MOOSE) group. JAMA 283:2008–2012
Higgins J, Green S (2011) Cochrane handbook for systematic reviews of interventions version 5.1.0. The Cochrane Collaboration www.cochranehandbook.org
Wells GA, Shea B, O'Connell D et al (2010) The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp
Higgins JP, Thompson SG (2002) Quantifying heterogeneity in a meta-analysis. Stat Med 21:1539–1558. https://doi.org/10.1002/sim.1186
Patsopoulos NA, Evangelou E, Ioannidis JP (2008) Sensitivity of between-study heterogeneity in meta-analysis: proposed metrics and empirical evaluation. Int J Epidemiol 37:1148–1157. https://doi.org/10.1093/ije/dyn065
Egger M, Davey Smith G, Schneider M et al (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315:629–634
Persico I, Cesari M, Morandi A et al (2018) Frailty and delirium in older adults: a systematic review and meta-analysis of the literature. J Am Geriatr Soc 66:2022–2030. https://doi.org/10.1111/jgs.15503
Tjeertes EKM, van Fessem JMK, Mattace-Raso FUS et al (2020) Influence of frailty on outcome in older patients undergoing non-cardiac surgery—a systematic review and meta-analysis. Aging Dis 11:1276–1290. https://doi.org/10.14336/AD.2019.1024
Janssen TL, Alberts AR, Hooft L et al (2019) Prevention of postoperative delirium in elderly patients planned for elective surgery: systematic review and meta-analysis. Clin Interv Aging 14:1095–1117. https://doi.org/10.2147/CIA.S201323
Hempenius L, Slaets JP, van Asselt D et al (2013) Outcomes of a geriatric liaison intervention to prevent the development of postoperative delirium in frail elderly cancer patients: report on a multicentre, randomized, controlled trial. PLoS ONE 8:e64834. https://doi.org/10.1371/journal.pone.0064834
Fabricio DM, Chagas MHN, Diniz BS (2020) Frailty and cognitive decline. Transl Res 221:58–64. https://doi.org/10.1016/j.trsl.2020.01.002
Daiello LA, Racine AM, Gou RY et al (2019) Postoperative delirium and postoperative cognitive dysfunction: overlap and divergence. Anesthesiology 131:477–491. https://doi.org/10.1097/ALN.0000000000002729
Wilson D, Jackson T, Sapey E et al (2017) Frailty and sarcopenia: the potential role of an aged immune system. Ageing Res Rev 36:1–10. https://doi.org/10.1016/j.arr.2017.01.006
Calvani R, Marini F, Cesari M et al (2017) Biomarkers for physical frailty and sarcopenia. Aging Clin Exp Res 29:29–34. https://doi.org/10.1007/s40520-016-0708-1
Mosk CA, van Vugt JLA, de Jonge H et al (2018) Low skeletal muscle mass as a risk factor for postoperative delirium in elderly patients undergoing colorectal cancer surgery. Clin Interv Aging 13:2097–2106. https://doi.org/10.2147/CIA.S175945
Makiguchi T, Yamaguchi T, Nakamura H et al (2020) Impact of skeletal muscle mass on postoperative delirium in patients undergoing free flap repair after oral cancer resection. J Plast Surg Hand Surg 54:161–166. https://doi.org/10.1080/2000656X.2020.1724545
Aucoin SD, Hao M, Sohi R et al (2020) Accuracy and feasibility of clinically applied frailty instruments before surgery: a systematic review and meta-analysis. Anesthesiology 133:78–95. https://doi.org/10.1097/ALN.0000000000003257
Borozdina A, Qeva E, Cinicola M et al (2018) Perioperative cognitive evaluation. Curr Opin Anaesthesiol 31:756–761. https://doi.org/10.1097/ACO.0000000000000658
Patel V, Champaneria R, Dretzke J et al (2018) Effect of regional versus general anaesthesia on postoperative delirium in elderly patients undergoing surgery for hip fracture: a systematic review. BMJ Open 8:e020757. https://doi.org/10.1136/bmjopen-2017-020757
Papadopoulos G, Pouangare M, Papathanakos G et al (2014) The effect of ondansetron on postoperative delirium and cognitive function in aged orthopedic patients. Minerva Anestesiol 80:444–451
Author information
Authors and Affiliations
Contributions
DF and JY designed the study; DF and XT performed literature search, study identification, and data extraction; DF, MZ and LC performed statistics; DF drafted the manuscript; JY critically reviewed the manuscript. All authors approved the submission.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Statement of human and animal rights
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
For this type of study, no informed consent is required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Fu, D., Tan, X., Zhang, M. et al. Association between frailty and postoperative delirium: a meta-analysis of cohort study. Aging Clin Exp Res 34, 25–37 (2022). https://doi.org/10.1007/s40520-021-01828-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-021-01828-9