Abstract
Background and aims
The Healthy Aging Index (HAI) is useful in capturing the health status of multiple organ systems in older adults. Previous studies have mainly focused on the association of HAI with mortality and disability. We constructed a modified HAI (mHAI) to examine its association with mobility limitations and falls in a community-based sampling of older Chinese adults.
Methods
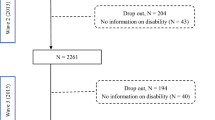
We investigated 399 community-dwelling older adults aged 80 years or older, and constructed the mHAI with five non-invasive tests (systolic blood pressure, the Montreal Cognitive Assessment test, glucose concentrations, cystatin C levels, and self-reported respiratory problems).
Results
The mean mHAI score for the participants in our study was 3.6. After multivariate adjustment, per unit increase in mHAI score was associated with self-reported difficulty in stooping, kneeling, or crouching (odds ratio [OR] = 1.16, 95% confidence interval [CI] 1.00–1.34), and walking 400 m (OR = 1.21, 95% CI 1.03–1.42). Per unit increase in mHAI score was also associated with poor balance (OR = 1.29, 95% CI 1.07–1.55), lower extremity strength limitation (OR = 1.30, 95% CI 1.10–1.52), low handgrip strength (OR = 1.25, 95% CI 1.08–1.46), and slow gait speed (OR = 1.21, 95% CI 1.02–1.42). The association between mHAI and falls was also significant (per unit of mHAI OR = 1.21, 95% CI 1.04–1.40).
Conclusion
The mHAI can be used as a simple assessment tool to determine mobility status in older adults and identify those at high risk for falls.

Similar content being viewed by others
References
Cesari M, Onder G, Russo A et al (2006) Comorbidity and physical function: results from the aging and longevity study in the Sirente geographic area (ilSIRENTE study). Gerontology 52:24–32
Charlson M, Szatrowski TP, Peterson J et al (1994) Validation of a combined comorbidity index. J Clin Epidemiol 47:1245–1251
Condon J, You J, McDonnell J (2012) Performance of comorbidity indices in measuring outcomes after acute myocardial infarction in Australian indigenous and non-indigenous patients. Intern Med J 42:165–173
Michel JP, Graf C, Ecarnot F (2019) Individual healthy aging indices, measurements and scores. Aging Clin Exp Res 31:1719–1725
Charlson ME, Pompei P, Ales KL et al (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40:373–383
Deyo RA, Cherkin DC, Ciol MA (1992) Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol 45:613–619
Romano PS, Roos LL, Jollis JG (1993) Adapting a clinical comorbidity index for use with ICD-9-CM administrative data: differing perspectives. J Clin Epidemiol 46:1075–1090
Newman AB, Boudreau RM, Naydeck BL et al (2008) A physiologic index of comorbidity: relationship to mortality and disability. J Gerontol A Biol Sci Med Sci 63:603–609
Sanders JL, Boudreau RM, Penninx BW et al (2012) Association of a Modified Physiologic Index with mortality and incident disability: the Health, Aging, and Body Composition study. J Gerontol A Biol Sci Med Sci 67:1439–1446
Wu C, Smit E, Sanders JL et al (2017) A modified healthy aging index and its association with mortality: the National Health and Nutrition Examination Survey, 1999–2002. J Gerontol A Biol Sci Med Sci 72:1437–1444
Committee of Cardio-Cerebro-Vascular Diseases of Gerontological Society of China (2017) Chinese College of Cardiovascular Physicians of Chinese Medical Doctor Association. Chinese expert consensus on the diagnosis and treatment of hypertension in the elderly. Zhonghua Nei Ke Za Zhi 56:885–893
Tan JP, Li N, Gao J et al (2015) Optimal cutoff scores for dementia and mild cognitive impairment of the Montreal Cognitive Assessment among elderly and oldest-old Chinese population. J Alzheimers Dis 43:1403–1412
Guralnik JM, Simonsick EM, Ferrucci L et al (1994) A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol 49:M85–94
Beauchet O, Dubost V, Revel Delhom C et al (2011) French Society of Geriatrics and Gerontology. How to manage recurrent falls in clinical practice: Guidelines of the French Society of Geriatrics and Gerontology. J Nutr Health Aging 15:79–84
Rosso AL, Sanders JL, Arnold AM et al (2015) Multisystem physiologic impairments and changes in gait speed of older adults. J Gerontol A Biol Sci Med Sci 70:317–322
Loprinzi PD, Addoh O, Joyner C (2016) Multimorbidity, mortality, and physical activity. Chronic Illn 12:272–280
MacKinnon HJ, Wilkinson TJ, Clarke AL et al (2018) The association of physical function and physical activity with all-cause mortality and adverse clinical outcomes in nondialysis chronic kidney disease: a systematic review. Ther Adv Chronic Dis 9:209–226
Landi F, Calvani R, Tosato M et al (2016) Impact of physical function impairment and multimorbidity on mortality among community-living older persons with sarcopaenia: results from the ilSIRENTE prospective cohort study. BMJ Open 6:e008281
Tinetti ME, Williams CS (1997) Falls, injuries due to falls, and the risk of admission to a nursing home. N Engl J Med 337:1279–1284
Olij BF, Panneman MJM, van Beeck EF et al (2019) Fall-related healthcare use and mortality among older adults in the Netherlands, 1997–2016. Exp Gerontol 120:95–100
Galet C, Zhou Y, Eyck PT et al (2018) Fall injuries, associated deaths, and 30-day readmission for subsequent falls are increasing in the elderly US population: a query of the WHO mortality database and National Readmission Database from 2010 to 2014. Clin Epidemiol 10:1627–1637
Oh J, Choi CK, Kim SA et al (2019) Association of falls and fear of falling with mortality in Korean adults: the Dong-gu study. Chonnam Med J 55:104–108
Sri-On J, Tirrell GP, Bean JF et al (2017) Revisit, subsequent hospitalization, recurrent fall, and death within 6 months after a fall among elderly emergency department patients. Ann Emerg Med 70:516–521.e2
Makino K, Makizako H, Doi T et al (2018) Impact of fear of falling and fall history on disability incidence among older adults: Prospective cohort study. Int J Geriatr Psychiatry 33:658–662
Acknowledgments
We acknowledge all participants involved in the present study.
Funding
Opening Foundation of National Clinical Research Center for Geriatric Diseases (NCRCG-PLAGH-2018008, NCRCG-PLAGH-2018010). Military Healthcare Fund (19BJZ34) and Military medicine fund for youth scholars of the Chinese PLA General Hospital (QNC19054).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The ethics committee of the Chinese PLA General Hospital approved this study, which complies with the current laws of China (Ethic number: S2018-102-01).
Informed consent
Written informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Li, K., Xu, W., Hu, B. et al. The modified Healthy Aging Index is associated with mobility limitations and falls in a community-based sample of oldest old. Aging Clin Exp Res 33, 555–562 (2021). https://doi.org/10.1007/s40520-020-01560-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-020-01560-w