Abstract
Introduction
Sodium–glucose cotransporter 2 (SGLT2) inhibitors are a relatively new class of antihyperglycemic agents, with the potential to inhibit breast cancer development. However, the association between SGLT2 inhibitors and risk of breast cancer in human studies is unclear.
Objective
The aim of our study is to use a large national claims database to assess the association between SGLT2 inhibitor use and risk of breast cancer.
Methods
We considered a study population of 158,483 adult women with type 2 diabetes who newly initiated SGLT2 inhibitors or dipeptidyl peptidase 4 (DPP4) inhibitors using Optum’s deidentified Clinformatics Data Mart Database between 1 January 2013 and 31 March 2022. The association between SGLT2 inhibitor use and risk of breast cancer was examined using Cox proportional hazard models stratified by age in the overall sample and in a subsample based on propensity score and medication initiation time matching. The effect of medication use duration was explored.
Results
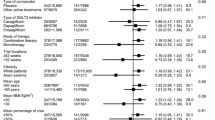
With an average follow-up of 2.2 years, 2154 breast cancer cases were identified. There was no significant association between SGLT2 inhibitor use and the risk of breast cancer in overall sample (HR = 0.96; 95% CI 0.87, 1.06), in women younger than 51 years old (HR = 0.88; 95% CI 0.59, 1.32), or in women aged 51 years or older (HR = 0.95; 95% CI 0.86, 1.04). The results remained nonsignificant using matching, medication use duration, and sensitivity analyses.
Conclusion
Our findings suggest SGLT2 inhibitors use was not associated with breast cancer risk compared with DPP4 inhibitors use. Studies with longer follow-up and better adjustments are needed to confirm the finding.

Similar content being viewed by others
References
Sung H, Ferlay J, Siegel RL, et al. Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71:209–49. https://doi.org/10.3322/caac.21660.
Economopoulou P, Dimitriadis G, Psyrri A. Beyond BRCA: new hereditary breast cancer susceptibility genes. Cancer Treat Rev. 2015;41:1–8. https://doi.org/10.1016/j.ctrv.2014.10.008.
Tomic D, Shaw JE, Magliano DJ. The burden and risks of emerging complications of diabetes mellitus. Nat Rev Endocrinol. 2022;18:525–39. https://doi.org/10.1038/s41574-022-00690-7.
Khan MAB, Hashim MJ, King JK, et al. Epidemiology of type 2 diabetes—global burden of disease and forecasted trends. J Epidemiol Glob Health. 2020;10:107–11. https://doi.org/10.2991/jegh.k.191028.001.
Tang H, Dai Q, Shi W, et al. SGLT2 inhibitors and risk of cancer in type 2 diabetes: a systematic review and meta-analysis of randomised controlled trials. Diabetologia. 2017;60:1862–72. https://doi.org/10.1007/s00125-017-4370-8.
Boyle P, Boniol M, Koechlin A, et al. Diabetes and breast cancer risk: a meta-analysis. Br J Cancer. 2012;107:1608–17. https://doi.org/10.1038/bjc.2012.414.
Warburg O, Wind F, Negelein E. The metabolism of tumors in the body. J Gen Physiol. 1927;8:519–30.
Lupsa BC, Inzucchi SE. Use of SGLT2 inhibitors in type 2 diabetes: weighing the risks and benefits. Diabetologia. 2018;61:2118–25. https://doi.org/10.1007/s00125-018-4663-6.
Pharmacologic Approaches to Glycemic Treatment: Standards of Medical Care in Diabetes—2022 | Diabetes Care | American Diabetes Association. https://diabetesjournals.org/care/article/45/Supplement_1/S125/138908/9-Pharmacologic-Approaches-to-Glycemic-Treatment. Accessed 24 Jan 2023
Fonseca-Correa JI, Correa-Rotter R. Sodium-glucose cotransporter 2 inhibitors mechanisms of action: a review. Front Med. 2021;8: 777861. https://doi.org/10.3389/fmed.2021.777861.
Lambers Heerspink HJ, de Zeeuw D, Wie L, et al. Dapagliflozin a glucose-regulating drug with diuretic properties in subjects with type 2 diabetes. Diabetes Obes Metab. 2013;15:853–62. https://doi.org/10.1111/dom.12127.
Lee T-M, Chang N-C, Lin S-Z. Dapagliflozin, a selective SGLT2 Inhibitor, attenuated cardiac fibrosis by regulating the macrophage polarization via STAT3 signaling in infarcted rat hearts. Free Radic Biol Med. 2017;104:298–310. https://doi.org/10.1016/j.freeradbiomed.2017.01.035.
Komatsu S, Nomiyama T, Numata T, et al. SGLT2 inhibitor ipragliflozin attenuates breast cancer cell proliferation. Endocrine J. 2020;67:99–106. https://doi.org/10.1507/endocrj.EJ19-0428.
Komatsu S, Nomiyama T, Numata T, et al. SGLT2 Inhibitor ipragliflozin induces breast cancer apoptosis via membrane hyperpolarization and mitochondria dysfunction. Diabetes. 2018;67:255-OR. https://doi.org/10.2337/db18-255-OR.
Ware K, Smith T, Brown D-V, et al. The effect of sodium glucose transporter 2 inhibitors on proliferation and growth factor signaling pathways in triple negative breast cancer. FASEB J. 2019;33:647.48. https://doi.org/10.1096/fasebj.2019.33.1_supplement.647.48.
Nasiri AR, Rodrigues MR, Li Z, et al. SGLT2 inhibition slows tumor growth in mice by reversing hyperinsulinemia. Cancer Metab. 2019;7:10. https://doi.org/10.1186/s40170-019-0203-1.
Zhou J, Zhu J, Yu S-J, et al. Sodium-glucose co-transporter-2 (SGLT-2) inhibition reduces glucose uptake to induce breast cancer cell growth arrest through AMPK/mTOR pathway. Biomed Pharmacother. 2020;132: 110821. https://doi.org/10.1016/j.biopha.2020.110821.
Benedetti R, Benincasa G, Glass K, et al. Effects of novel SGLT2 inhibitors on cancer incidence in hyperglycemic patients: a meta-analysis of randomized clinical trials. Pharmacol Res. 2022;175: 106039. https://doi.org/10.1016/j.phrs.2021.106039.
Jones D. Diabetes field cautiously upbeat despite possible setback for leading SGLT2 inhibitor. Nat Rev Drug Discov. 2011;10:645–6. https://doi.org/10.1038/nrd3546.
Marilly E, Cottin J, Cabrera N, et al. SGLT2 inhibitors in type 2 diabetes: a systematic review and meta-analysis of cardiovascular outcome trials balancing their risks and benefits. Diabetologia. 2022;65:2000–10. https://doi.org/10.1007/s00125-022-05773-8.
Dadey DYA, Rodrigues A, Haider G, et al. Impact of socio-economic factors on radiation treatment after resection of metastatic brain tumors: trends from a private insurance database. J Neurooncol. 2022;158:445–51. https://doi.org/10.1007/s11060-022-04031-6.
Clinformatics® Data Mart. https://cdn-aem.optum.com/content/dam/optum4/resources/pdf/clinformatics-data-mart.pdf. Accessed 26 Jan 2023.
Suissa K, Schneeweiss S, Lin KJ, et al. Validation of obesity-related diagnosis codes in claims data. Diabetes Obes Metab. 2021;23:2623–31. https://doi.org/10.1111/dom.14512.
Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43:1130–9. https://doi.org/10.1097/01.mlr.0000182534.19832.83.
NCI Comorbidity Index Overview. https://healthcaredelivery.cancer.gov/seermedicare/considerations/comorbidity.html. Accessed 25 Aug 2023
Segal Z, Kalifa D, Radinsky K, et al. Machine learning algorithm for early detection of end-stage renal disease. BMC Nephrol. 2020;21:518. https://doi.org/10.1186/s12882-020-02093-0.
Box-Steffensmeier JM, Jones BS. Event history modeling: a guide for social scientists. Cambridge: Cambridge University Press; 2004.
Surakasula A, Nagarjunapu GC, Raghavaiah KV. A comparative study of pre- and post-menopausal breast cancer: risk factors, presentation, characteristics and management. J Res Pharm Pract. 2014;3:12–8. https://doi.org/10.4103/2279-042X.132704.
Biglia N, Peano E, Sgandurra P, et al. Body mass index (BMI) and breast cancer: impact on tumor histopatologic features, cancer subtypes and recurrence rate in pre and postmenopausal women. Gynecol Endocrinol. 2013;29:263–7. https://doi.org/10.3109/09513590.2012.736559.
Chollet-Hinton L, Anders CK, Tse C-K, et al. Breast cancer biologic and etiologic heterogeneity by young age and menopausal status in the Carolina Breast Cancer Study: a case-control study. Breast Cancer Res. 2016;18:79. https://doi.org/10.1186/s13058-016-0736-y.
Hicks B, Kaye JA, Azoulay L, et al. The application of lag times in cancer pharmacoepidemiology: a narrative review. Ann Epidemiol. 2023;84:25–32. https://doi.org/10.1016/j.annepidem.2023.05.004.
Austin PC. Optimal caliper widths for propensity-score matching when estimating differences in means and differences in proportions in observational studies. Pharm Stat. 2011;10:150–61. https://doi.org/10.1002/pst.433.
Bergstralh EJ, Kosanke JL, Jacobsen SJ. Software for optimal matching in observational studies. Epidemiology. 1996;7:331–2.
Lin DY, Wei LJ. The robust inference for the Cox proportional hazards model. J Am Stat Assoc. 1989;84:1074–8. https://doi.org/10.1080/01621459.1989.10478874.
Austin PC. The performance of different propensity score methods for estimating marginal hazard ratios. Stat Med. 2013;32:2837–49. https://doi.org/10.1002/sim.5705.
Zou H-T, Yang G-H, Cai Y-J, et al. Are high- or low-dose SGLT2 inhibitors associated with cardiovascular and respiratory adverse events? A meta-analysis. J Cardiovasc Pharmacol. 2022;79:655. https://doi.org/10.1097/FJC.0000000000001222.
McMurray JJV, Solomon SD, Inzucchi SE, et al. Dapagliflozin in patients with heart failure and reduced ejection fraction. N Engl J Med. 2019;381:1995–2008. https://doi.org/10.1056/NEJMoa1911303.
Suissa M, Yin H, Yu OHY, et al. Sodium–glucose cotransporter 2 inhibitors and the short-term risk of breast cancer among women with type 2 diabetes. Diabetes Care. 2020;44:e9–11. https://doi.org/10.2337/dc20-1073.
Dicembrini I, Nreu B, Montereggi C, et al. Risk of cancer in patients treated with dipeptidyl peptidase-4 inhibitors: an extensive meta-analysis of randomized controlled trials. Acta Diabetol. 2020;57:689–96. https://doi.org/10.1007/s00592-020-01479-8.
Tilinca MC, Tiuca RA, Tilea I, Varga A. The SGLT-2 inhibitors in personalized therapy of diabetes mellitus patients. J Pers Med. 2021;11:1249. https://doi.org/10.3390/jpm11121249.
Salvatore T, Galiero R, Caturano A, et al. An overview of the cardiorenal protective mechanisms of SGLT2 inhibitors. Int J Mol Sci. 2022;23:3651. https://doi.org/10.3390/ijms23073651.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Not applicable.
Conflicts of Interest
The authors declare that there are no competing interests.
Availability of Data and Material
The data supporting this study's findings are not publicly available due to reasons of sensitivity but can be accessed from Optum on reasonable request. Optum service website: https://www.optum.com/business/insights/life-sciences/page.hub.contact-lifesciences.html.
Ethics Approval
This study was approved by the Indiana University institutional review board (protocol number: 21486).
Consent for Participate
Consent was waived by the institutional review board due to the utilization of deidentified data.
Consent for Publication
Not applicable.
Code Availability
Available on reasonable request from the corresponding author.
Author Contributions
FW, JL, and MH contributed to the design of the study. FW performed the analysis. The first draft of the manuscript was written by FW and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wang, F., Hendryx, M., Liu, N. et al. SGLT2 Inhibitor Use and Risk of Breast Cancer Among Adult Women with Type 2 Diabetes. Drug Saf 47, 125–133 (2024). https://doi.org/10.1007/s40264-023-01373-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40264-023-01373-6