Abstract
Background
Early non-response is a well-established prognostic marker but evidence-based and consistent recommendations to manage it are limited. The aim of this systematic review and meta-analysis was to generate evidence-based strategies for the management of schizophrenia patients with early non-response to 2 weeks of antipsychotic treatment.
Methods
We conducted a systematic review and meta-analysis of randomized trials comparing antipsychotic dose escalation, switch, augmentation and continuation in individuals with study-defined early antipsychotic treatment non-response. Eligibility criteria were (1) clinical trials of primary psychosis treating for at least 2 weeks with antipsychotic monotherapy with study-defined operationalized criteria for early non-response; and (2) randomization to at least two of the following treatment strategies: dose escalation, switch, augmentation, or treatment continuation. Information sources were Pubmed, PsycINFO, and EMBASE, and risk of bias was assessed using Jadad scores. Results were synthesized using random-effects meta-analysis, comparing each intervention with treatment continuation for total symptom change as the primary outcome, generating standardized mean differences (SMDs) and 95% confidence intervals (CIs). Studies meeting the selection criteria but providing insufficient data for a meta-analysis were presented separately.
Results
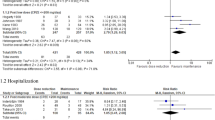
We screened 454 records by 1 August 2022, of which 12 individual datasets met the inclusion criteria, representing 947 research participants. Of those studies, five provided data to include in the meta-analysis (four with early non-response at 2 weeks, one at 3 weeks). Early non-response was defined within a timeline of 2 weeks in eight datasets, with the remaining datasets ranging between 3 and 4 weeks. The rates of early non-response ranged between 72.0 and 24.1%, and the endpoint ranged within 4–24 weeks post randomization. Quality was good (i.e., Jadad score of ≥3) in 8 of the 12 datasets. Overall, three studies compared antipsychotic switch versus continuation and two compared antipsychotic switch versus augmentation, in both cases without significant pooled between-group differences for total symptom severity (n = 149, SMD 0.18, 95% CI −0.14 to 0.5). Individually, two relatively large studies for antipsychotic switch versus continuation found small advantages for switching antipsychotics for total symptom severity (n = 149, SMD −0.49, 95% CI −1.05 to −0.06). One relatively large study found an advantage for dose escalation, although this finding has not been replicated and was not included in the meta-analysis. None of the alternatives included antipsychotic switch to clozapine.
Conclusions
Despite robust accuracy of early antipsychotic non-response predicting ultimate response, the evidence for treatment strategies that should be used for early non-response after 2–3 weeks is limited. While meta-analytic findings were non-significant, some individual studies suggest advantages of antipsychotic switch or dose escalation. Therefore, any conclusions should be interpreted carefully, given the insufficient high-quality evidence.



Similar content being viewed by others
References
Charlson FJ, Ferrari AJ, Santomauro DF, et al. Global epidemiology and burden of Schizophrenia: findings from the global burden of disease study 2016. Schizophr Bull. 2018;44(6):1195–203. https://doi.org/10.1093/schbul/sby058.
Kahn RS, Sommer IE, Murray RM, et al. Schizophrenia. Nat Rev Dis Primer. 2015;2:15067. https://doi.org/10.1038/nrdp.2015.67.
McCutcheon RA, Pillinger T, Efthimiou O, et al. Reappraising the variability of effects of antipsychotic medication in schizophrenia: a meta-analysis. World Psychiatry. 2022;21(2):287–94. https://doi.org/10.1002/wps.20977.
Winkelbeiner S, Leucht S, Kane JM, Homan P. Evaluation of differences in individual treatment response in schizophrenia spectrum disorders: a meta-analysis. JAMA Psychiat. 2019;76(10):1063–73. https://doi.org/10.1001/jamapsychiatry.2019.1530.
Sarpal DK, Argyelan M, Robinson DG, et al. Baseline striatal functional connectivity as a predictor of response to antipsychotic drug treatment. Am J Psychiatry. 2016;173(1):69–77. https://doi.org/10.1176/appi.ajp.2015.14121571.
Li A, Zalesky A, Yue W, et al. A neuroimaging biomarker for striatal dysfunction in schizophrenia. Nat Med. 2020;26(4):558–65. https://doi.org/10.1038/s41591-020-0793-8.
Samara MT, Leucht C, Leeflang MM, et al. Early improvement as a predictor of later response to antipsychotics in schizophrenia: a diagnostic test review. Am J Psychiatry. 2015;172(7):617–29. https://doi.org/10.1176/appi.ajp.2015.14101329.
Leucht S, Kane JM, Kissling W, Hamann J, Etschel E, Engel RR. What does the PANSS mean? Schizophr Res. 2005;79(2–3):231–8. https://doi.org/10.1016/j.schres.2005.04.008.
Remington G, Addington D, Honer W, Ismail Z, Raedler T, Teehan M. Guidelines for the pharmacotherapy of schizophrenia in adults. Can J Psychiatry. 2017;62(9):604–16. https://doi.org/10.1177/0706743717720448.
Keepers GA, Fochtmann LJ, Anzia JM, et al. The American psychiatric association practice guideline for the treatment of patients with schizophrenia. Am J Psychiatry. 2020;177(9):868–72. https://doi.org/10.1176/appi.ajp.2020.177901.
Hasan A, Falkai P, Wobrock T, et al. World Federation of Societies of Biological Psychiatry (WFSBP) Guidelines for Biological Treatment of Schizophrenia, part 1: update 2012 on the acute treatment of schizophrenia and the management of treatment resistance. World J Biol Psychiatry. 2012;13(5):318–78. https://doi.org/10.3109/15622975.2012.696143.
Buckley PF, Correll CU. Strategies for dosing and switching antipsychotics for optimal clinical management. J Clin Psychiatry. 2008;69(Suppl 1):4–17.
Kahn RS, van Winter RI, Leucht S, et al. Amisulpride and olanzapine followed by open-label treatment with clozapine in first-episode schizophrenia and schizophreniform disorder (OPTiMiSE): a three-phase switching study. Lancet Psychiatry. 2018;5(10):797–807. https://doi.org/10.1016/S2215-0366(18)30252-9.
Correll CU, Rubio JM, Inczedy-Farkas G, Birnbaum ML, Kane JM, Leucht S. Efficacy of 42 pharmacologic cotreatment strategies added to antipsychotic monotherapy in schizophrenia: systematic overview and quality appraisal of the meta-analytic evidence. JAMA Psychiat. 2017;74(7):675–84. https://doi.org/10.1001/jamapsychiatry.2017.0624.
Galling B, Roldán A, Hagi K, Rietschel L, Walyzada F, Zheng W, et al. Antipsychotic augmentation vs monotherapy in schizophrenia: systematic review, meta-analysis and meta-regression analysis. World Psychiatry. 2017;16(1):77–89.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7): e1000097. https://doi.org/10.1371/journal.pmed.1000097.
Jadad AR, Moore RA, Carroll D, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996;17(1):1–12. https://doi.org/10.1016/0197-2456(95)00134-4.
R Core Team (2020). R: A language and environment for statistical computing. Vienna: R Foundation for Statistical Computing. URL https://www.R-project.org/.
Suzuki T, Uchida H, Watanabe K, et al. How effective is it to sequentially switch among Olanzapine, Quetiapine and Risperidone? A randomized, open-label study of algorithm-based antipsychotic treatment to patients with symptomatic schizophrenia in the real-world clinical setting. Psychopharmacology. 2007;195(2):285–95. https://doi.org/10.1007/s00213-007-0872-2.
Kinon BJ, Kane JM, Johns C, et al. Treatment of neuroleptic-resistant schizophrenic relapse. Psychopharmacol Bull. 1993;29(2):309–14.
Shalev A, Hermesh H, Rothberg J, Munitz H. Poor neuroleptic response in acutely exacerbated schizophrenic patients. Acta Psychiatr Scand. 1993;87(2):86–91. https://doi.org/10.1111/j.1600-0447.1993.tb03335.x.
Kinon BJ, Chen L, Ascher-Svanum H, et al. Early response to antipsychotic drug therapy as a clinical marker of subsequent response in the treatment of schizophrenia. Neuropsychopharmacol. 2010;35(2):581–90. https://doi.org/10.1038/npp.2009.164.
Heres S, Cordes J, Feyerabend S, et al. Changing the antipsychotic in early nonimprovers to amisulpride or olanzapine: randomized, double-blind trial in patients with schizophrenia. Schizophr Bull. 2022;48(6):1273–83. https://doi.org/10.1093/schbul/sbac068.
Loebel A, Silva R, Goldman R, et al. Lurasidone dose escalation in early nonresponding patients with schizophrenia: a randomized placebo-controlled study. J Clin Psychiatry. 2016;77(12):1672–80. https://doi.org/10.4088/JCP.16m10698.
Hatta K, Otachi T, Sudo Y, et al. A comparison between augmentation with olanzapine and increased risperidone dose in acute schizophrenia patients showing early non-response to risperidone. Psychiatry Res. 2012;198(2):194–201. https://doi.org/10.1016/j.psychres.2012.01.006.
Hatta K, Otachi T, Fujita K, et al. Antipsychotic switching versus augmentation among early non-responders to risperidone or olanzapine in acute-phase schizophrenia. Schizophr Res. 2014;158(1–3):213–22. https://doi.org/10.1016/j.schres.2014.07.015.
Correll CU, Martin A, Patel C, et al. Systematic literature review of schizophrenia clinical practice guidelines on acute and maintenance management with antipsychotics. NPJ Schizophr. 2022;8(1):5. https://doi.org/10.1038/s41537-021-00192-x.
Howes OD, McCutcheon R, Agid O, et al. Treatment-resistant schizophrenia: treatment response and resistance in psychosis (TRRIP) working group consensus guidelines on diagnosis and terminology. Am J Psychiatry. 2017;174(3):216–29. https://doi.org/10.1176/appi.ajp.2016.16050503.
Correll CU, Citrome L, Haddad PM, et al. The use of long-acting injectable antipsychotics in schizophrenia: evaluating the evidence. J Clin Psychiatry. 2016;77(Suppl 3):1–24. https://doi.org/10.4088/JCP.15032su1.
Lopez LV, Shaikh A, Merson J, Greenberg J, Suckow RF, Kane JM. Accuracy of clinician assessments of medication status in the emergency setting: a comparison of clinician assessment of antipsychotic usage and plasma level determination. J Clin Psychopharmacol. 2017;37(3):310–4. https://doi.org/10.1097/JCP.0000000000000697.
McCutcheon R, Beck K, D’Ambrosio E, et al. Antipsychotic plasma levels in the assessment of poor treatment response in schizophrenia. Acta Psychiatr Scand. 2018;137(1):39–46. https://doi.org/10.1111/acps.12825.
Rubio JM, Schoretsanitis G, John M, et al. Psychosis relapse during treatment with long-acting injectable antipsychotics in individuals with schizophrenia-spectrum disorders: an individual participant data meta-analysis. Lancet Psychiatry. 2020;7(9):749–61. https://doi.org/10.1016/S2215-0366(20)30264-9.
Bak M. Monitoring clozapine adverse effects calls for the integration of protocol and good clinical practice. J Clin Psychiatry. 2012;73(10):1313–4. https://doi.org/10.4088/JCP.12com07964.
Kane JM, Agid O, Baldwin ML, et al. Clinical Guidance on the Identification and Management of Treatment-Resistant Schizophrenia. J Clin Psychiatry. 2019;80(2):18123. https://doi.org/10.4088/JCP.18com12123.
Nielsen J, Nielsen RE, Correll CU. Predictors of clozapine response in patients with treatment-refractory schizophrenia: results from a Danish Register Study. J Clin Psychopharmacol. 2012;32(5):678–83. https://doi.org/10.1097/JCP.0b013e318267b3cd.
Thien K, O’Donoghue B. Delays and barriers to the commencement of clozapine in eligible people with a psychotic disorder: a literature review. Early Interv Psychiatry. 2019;13(1):18–23. https://doi.org/10.1111/eip.12683.
Bachmann CJ, Aagaard L, Bernardo M, et al. International trends in clozapine use: a study in 17 countries. Acta Psychiatr Scand. 2017;136(1):37–51. https://doi.org/10.1111/acps.12742.
Bareis N, Olfson M, Wall M, Stroup TS. Variation in psychotropic medication prescription for adults with schizophrenia in the United States. Psychiatr Serv. 2022;73(5):492–500. https://doi.org/10.1176/appi.ps.202000932.
Potkin SG, Kane JM, Correll CU, et al. The neurobiology of treatment-resistant schizophrenia: paths to antipsychotic resistance and a roadmap for future research. NPJ Schizophr. 2020;6(1):1. https://doi.org/10.1038/s41537-019-0090-z.
Koutsouleris N, Kambeitz-Ilankovic L, Ruhrmann S, et al. Prediction models of functional outcomes for individuals in the clinical high-risk state for psychosis or with recent-onset depression: a multimodal, multisite machine learning analysis. JAMA Psychiat. 2018;75(11):1156. https://doi.org/10.1001/jamapsychiatry.2018.2165.
Gallego JA, Robinson DG, Sevy SM, et al. Time to treatment response in first-episode schizophrenia: should acute treatment trials last several months? J Clin Psychiatry. 2011;72(12):1691–6. https://doi.org/10.4088/JCP.10m06349.
Case M, Stauffer VL, Ascher-Svanum H, et al. The heterogeneity of antipsychotic response in the treatment of schizophrenia. Psychol Med. 2011;41(6):1291–300. https://doi.org/10.1017/S0033291710001893.
Ketter TA, Agid O, Kapur S, Loebel A, Siu CO, Romano SJ. Rapid antipsychotic response with ziprasidone predicts subsequent acute manic/mixed episode remission. J Psychiatr Res. 2010;44(1):8–14. https://doi.org/10.1016/j.jpsychires.2009.07.006.
Agid O, Kapur S, Arenovich T, Zipursky RB. Delayed-onset hypothesis of antipsychotic action: a hypothesis tested and rejected. Arch Gen Psychiatry. 2003;60(12):1228–35. https://doi.org/10.1001/archpsyc.60.12.1228.
Schoretsanitis G, Kane JM, Correll CU, et al. Blood levels to optimize antipsychotic treatment in clinical practice: a joint consensus statement of the american society of clinical psychopharmacology and the therapeutic drug monitoring task force of the arbeitsgemeinschaft für neuropsychopharmakologie und pharmakopsychiatrie. J Clin Psychiatry. 2020;81(3):199. https://doi.org/10.4088/JCP.19cs13169.
Woo YS, Park SY, Yoon BH, Choi WS, Wang SM, Bahk WM. Amisulpride augmentation in schizophrenia patients with poor response to olanzapine: a 4-week, randomized, rater-blind, controlled Pilot Study. Clin Psychopharmacol Neurosci. 2022;20(3):567–72. https://doi.org/10.9758/cpn.2022.20.3.567.
Hatta K, Otachi T, Sudo Y, et al. Difference in early prediction of antipsychotic non-response between risperidone and olanzapine in the treatment of acute-phase schizophrenia. Schizophr Res. 2011;128(1–3):127–35. https://doi.org/10.1016/j.schres.2011.02.011.
Loebel A, Citrome L, Correll CU, Xu J, Cucchiaro J, Kane JM. Treatment of early non-response in patients with schizophrenia: assessing the efficacy of antipsychotic dose escalation. BMC Psychiatry. 2015;15:271. https://doi.org/10.1186/s12888-015-0629-0.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Jose M. Rubio was supported in part by grant number K23MH127300. No funding was specifically received for this article.
Author contributions
CUC conceptualized the study; DG and JMR conducted the record search; and JMR conducted the analyses and wrote the first iteration of the manuscript. All co-authors provided meaningful edits to the final version of the manuscript. All authors agree to be accountable for this work.
Conflicts of interest
Jose M. Rubio has been a consultant for Lundbeck, Teva and Janssen, has received research funding from Alkermes, and receives royalties from UpToDate. Daniel Guinart has been a consultant for and/or has received speaker honoraria from Otsuka America Pharmaceuticals, Janssen Pharmaceuticals, Lundbeck and Teva. Christoph U. Correll has been a consultant and/or advisor to, or has received honoraria from, AbbVie, Acadia, Alkermes, Allergan, Angelini, Aristo, Boehringer-Ingelheim, Cardio Diagnostics, Cerevel, CNX Therapeutics, Compass Pathways, Darnitsa, Gedeon Richter, Hikma, Holmusk, IntraCellular Therapies, Janssen/J&J, Karuna, LB Pharma, Lundbeck, MedAvante-ProPhase, MedInCell, Merck, Mindpax, Mitsubishi Tanabe Pharma, Mylan, Neurocrine, Newron, Noven, Otsuka, Pharmabrain, PPD Biotech, Recordati, Relmada, Reviva, Rovi, Seqirus, SK Life Science, Sunovion, Sun Pharma, Supernus, Takeda, Teva, and Viatris; provided expert testimony for Janssen and Otsuka; served on a Data Safety Monitoring Board for Lundbeck, Relmada, Reviva, Rovi, Supernus, and Teva; received grant support from Janssen and Takeda; received royalties from UpToDate; and is a stock option holder of Cardio Diagnostics, Mindpax, LB Pharma and Quantic. John M. Kane has been a consultant for or received honoraria from Alkermes, Forum, Allergan, Genentech, Lundbeck, Intracellular Therapies, Janssen Pharmaceutica, Johnson & Johnson, Merck, Neurocrine, Otsuka, Pierre Fabre, Reviva, Roche, Sunovion, Takeda and Teva; has received grant support from Otsuka Lundbeck and Janssen; and is a shareholder in Vanguard Research, LB PharmaGroup, and LB Pharmaceuticals, Inc.
Availability of data
Not applicable.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Code availability
Not applicable.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Rubio, J.M., Guinart, D., Kane, J.M. et al. Early Non-Response to Antipsychotic Treatment in Schizophrenia: A Systematic Review and Meta-Analysis of Evidence-Based Management Options. CNS Drugs 37, 499–512 (2023). https://doi.org/10.1007/s40263-023-01009-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40263-023-01009-4