Abstract
Background and Objective
The relationship between hyperuricemia and mortality in patients with acute coronary syndrome (ACS) is considerably controversial. Additionally, the strategy of dual antiplatelet therapy (DAPT) has not been evaluated in patients with ACS with hyperuricemia. This study aims to evaluate the impact of hyperuricemia on the prognosis of ACS and explore the efficacy of ticagrelor compared with clopidogrel in patients with hyperuricemia.
Methods
The study enrolled 4319 patients divided into hyperuricemia (HUA, n = 1060) and normouricemia (NUA, n = 3259) groups. The inverse probability of treatment weighting (IPTW)-adjusted Cox regression analysis was used to evaluate the impact of ticagrelor versus clopidogrel on all-cause and cardiovascular mortality.
Results
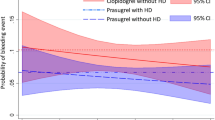
Hyperuricemia significantly increased the risk of all-cause death compared with patients with NUA at 7 days [adjusted hazard ratio (HR): 4.292, 95% confidence interval (CI) 1.727–10.67]; P = 0.002), 14 days (adjusted HR: 2.871, 95% CI 1.326–6.219; P = 0.0074), 30 days (adjusted HR: 2.168, 95% CI 1.056–4.453; P = 0.035), 3 months (adjusted HR: 2.018, 95% CI 1.152–3.533; P = 0.0144) and 1 year (adjusted HR: 1.702, 95% CI 1.137–2.548; P = 0.009). No significant difference was found between ticagrelor and clopidogrel in 1-year all-cause mortality [7.0% versus 5.5%, adjusted HR: 1.114 (95% CI 0.609–2.037), P = 0.725] among patients with concomitant hyperuricemia.
Conclusion
Hyperuricemia was independently related to an increased risk of all-cause and cardiovascular death in patients with ACS undergoing PCI. At 1-year follow-up, there were no significant differences between ticagrelor and clopidogrel concerning all-cause and cardiovascular death in patients with hyperuricemia.




Similar content being viewed by others
References
Bergmark BA, Mathenge N, Merlini PA, Lawrence-Wright MB, Giugliano RP. Acute coronary syndromes. Lancet. 2022;399(10332):1347–58. https://doi.org/10.1016/S0140-6736(21)02391-6.
Bhatt DL, Lopes RD, Harrington RA. Diagnosis and treatment of acute coronary syndromes: a review. JAMA. 2022;327(7):662–75. https://doi.org/10.1001/jama.2022.0358.
Virdis A, Masi S, Casiglia E, Tikhonoff V, Cicero A, Ungar A, et al. Identification of the uric acid thresholds predicting an increased total and cardiovascular mortality over 20 years. Hypertension. 2020;75(2):302–8. https://doi.org/10.1161/HYPERTENSIONAHA.119.13643.
Rodrigues BS, Alves M, Duarte GS, Costa J, Pinto FJ, Caldeira D. The impact of influenza vaccination in patients with cardiovascular disease: an overview of systematic reviews. Trends Cardiovasc Med. 2021;31(5):315–20. https://doi.org/10.1016/j.tcm.2020.06.003.
Zhang M, Zhu X, Wu J, Huang Z, Zhao Z, Zhang X, et al. Prevalence of hyperuricemia among chinese adults: findings from two nationally representative cross-sectional surveys in 2015–16 and 2018–19. Front Immunol. 2021;12: 791983. https://doi.org/10.3389/fimmu.2021.791983.
Gaubert M, Bardin T, Cohen-Solal A, Diévart F, Fauvel JP, Guieu R, et al. Hyperuricemia and hypertension, coronary artery disease, kidney disease: from concept to practice. Int J Mol Sci. 2020. https://doi.org/10.3390/ijms21114066.
Huang H, Huang B, Li Y, Huang Y, Li J, Yao H, et al. Uric acid and risk of heart failure: a systematic review and meta-analysis. Eur J Heart Fail. 2014;16(1):15–24. https://doi.org/10.1093/eurjhf/hft132.
Cheong E, Ryu S, Lee JY, Lee SH, Sung JW, Cho DS, et al. Association between serum uric acid and cardiovascular mortality and all-cause mortality: a cohort study. J Hypertens. 2017;35(Suppl 1):S3-09. https://doi.org/10.1097/HJH.0000000000001330.
Landolfo M, Borghi C. Hyperuricaemia and vascular risk: the debate continues. Curr Opin Cardiol. 2019;34(4):399–405. https://doi.org/10.1097/HCO.0000000000000626.
Kamran H, Jneid H, Kayani WT, Virani SS, Levine GN, Nambi V, et al. Oral antiplatelet therapy after acute coronary syndrome: a review. JAMA. 2021;325(15):1545–55. https://doi.org/10.1001/jama.2021.0716.
Sibbing D, Aradi D, Alexopoulos D, Ten BJ, Bhatt DL, Bonello L, et al. Updated expert consensus statement on platelet function and genetic testing for guiding P2Y12 receptor inhibitor treatment in percutaneous coronary intervention. JACC Cardiovasc Interv. 2019;12(16):1521–37. https://doi.org/10.1016/j.jcin.2019.03.034.
Tantry US, Navarese EP, Myat A, Gurbel PA. Selection of P2Y12 inhibitor in percutaneous coronary intervention and/or acute coronary syndrome. Prog Cardiovasc Dis. 2018;60(4–5):460–70. https://doi.org/10.1016/j.pcad.2018.01.003.
Kohli P, Wallentin L, Reyes E, Horrow J, Husted S, Angiolillo DJ, et al. Reduction in first and recurrent cardiovascular events with ticagrelor compared with clopidogrel in the PLATO study. Circulation. 2013;127(6):673–80. https://doi.org/10.1161/CIRCULATIONAHA.112.124248.
Rodriguez F, Mahaffey KW. Management of patients with NSTE-ACS: a comparison of the recent AHA/ACC and ESC guidelines. J Am Coll Cardiol. 2016;68(3):313–21. https://doi.org/10.1016/j.jacc.2016.03.599.
Nie S, Chen K, Guo C, Pei Q, Zou C, Yao L, et al. Effect of CYP4F2 Polymorphisms on ticagrelor pharmacokinetics in healthy chinese volunteers. Front Pharmacol. 2021;12: 797278. https://doi.org/10.3389/fphar.2021.797278.
Butler K, Teng R. Evaluation and characterization of the effects of ticagrelor on serum and urinary uric acid in healthy volunteers. Clin Pharmacol Ther. 2012;91(2):264–71. https://doi.org/10.1038/clpt.2011.223.
Liu S, Wu X, Lopez AD, Wang L, Cai Y, Page A, et al. An integrated national mortality surveillance system for death registration and mortality surveillance. China Bull World Health Organ. 2016;94(1):46–57. https://doi.org/10.2471/BLT.15.153148.
Cole SR, Hernán MA. Constructing inverse probability weights for marginal structural models. Am J Epidemiol. 2008;168(6):656–64. https://doi.org/10.1093/aje/kwn164.
Culleton BF, Larson MG, Kannel WB, Levy D. Serum uric acid and risk for cardiovascular disease and death: the Framingham Heart Study. Ann Intern Med. 1999;131(1):7–13. https://doi.org/10.7326/0003-4819-131-1-199907060-00003.
Nieto FJ, Iribarren C, Gross MD, Comstock GW, Cutler RG. Uric acid and serum antioxidant capacity: a reaction to atherosclerosis? Atherosclerosis. 2000;148(1):131–9. https://doi.org/10.1016/s0021-9150(99)00214-2.
Panero F, Gruden G, Perotto M, Fornengo P, Barutta F, Greco E, et al. Uric acid is not an independent predictor of cardiovascular mortality in type 2 diabetes: a population-based study. Atherosclerosis. 2012;221(1):183–8. https://doi.org/10.1016/j.atherosclerosis.2011.11.042.
Pagidipati NJ, Hess CN, Clare RM, Akerblom A, Tricoci P, Wojdyla D, et al. An examination of the relationship between serum uric acid level, a clinical history of gout, and cardiovascular outcomes among patients with acute coronary syndrome. Am Heart J. 2017;187:53–61. https://doi.org/10.1016/j.ahj.2017.02.023.
Chen C, Dong J, Lv Q, Liu X, Zhang Q, Du X. Effect of asymptomatic hyperuricemia on mortality of elderly patients after elective percutaneous coronary intervention. Front Cardiovasc Med. 2022;9: 800414. https://doi.org/10.3389/fcvm.2022.800414.
Ye Z, Lu H, Long M, Li L. Baseline serum uric acid levels are associated with all-cause mortality in acute coronary syndrome patients after percutaneous coronary intervention. Dis Markers. 2018;2018:9731374. https://doi.org/10.1155/2018/9731374.
Zhao G, Huang L, Song M, Song Y. Baseline serum uric acid level as a predictor of cardiovascular disease related mortality and all-cause mortality: a meta-analysis of prospective studies. Atherosclerosis. 2013;231(1):61–8. https://doi.org/10.1016/j.atherosclerosis.2013.08.023.
Li B, Chen L, Hu X, Tan T, Yang J, Bao W, Rong S. Association of serum uric acid with all-cause and cardiovascular mortality in diabetes. Diabetes Care. 2023;46(2):425–33. https://doi.org/10.2337/dc22-1339.
Gherghina ME, Peride I, Tiglis M, Neagu TP, Niculae A, Checherita IA. Uric acid and oxidative stress-relationship with cardiovascular, metabolic, and renal impairment. Int J Mol Sci. 2022. https://doi.org/10.3390/ijms23063188.
Han Y, Claessen BE, Chen SL, Chunguang Q, Zhou Y, Xu Y, et al. Ticagrelor with or without aspirin in chinese patients undergoing percutaneous coronary intervention: a TWILIGHT China substudy. Circ Cardiovasc Interv. 2022;15(4): e9495. https://doi.org/10.1161/CIRCINTERVENTIONS.120.009495.
Kim BK, Hong SJ, Cho YH, Yun KH, Kim YH, Suh Y, et al. Effect of ticagrelor monotherapy vs ticagrelor with aspirin on major bleeding and cardiovascular events in patients with acute coronary syndrome: the TICO Randomized Clinical Trial. JAMA. 2020;323(23):2407–16. https://doi.org/10.1001/jama.2020.7580.
Lee S, Wadowski PP, Hoberstorfer T, Weikert C, Pultar J, Kopp CW, et al. Decreased platelet inhibition by thienopyridines in hyperuricemia. Cardiovasc Drugs Ther. 2021;35(1):51–60. https://doi.org/10.1007/s10557-020-07058-x.
Goto S, Huang CH, Park SJ, Emanuelsson H, Kimura T. Ticagrelor vs. clopidogrel in Japanese, Korean and Taiwanese patients with acute coronary syndrome—randomized, double-blind, phase III PHILO study. Circ J. 2015;79(11):2452–60. https://doi.org/10.1253/circj.CJ-15-0112.
Bryant CE, Rajai A, Webb NJA, Hogg RJ. Effects of losartan and enalapril on serum uric acid and GFR in children with proteinuria. Pediatr Nephrol. 2021;36(10):3211–9. https://doi.org/10.1007/s00467-021-05045-4.
Ferreira JP, Zannad F, Kiernan MS, Konstam MA. High- versus low-dose losartan and uric acid: an analysis from HEAAL. J Cardiol. 2023;82(1):57–61. https://doi.org/10.1016/j.jjcc.2023.04.005.
Suijk DLS, van Baar MJB, van Bommel EJM, Iqbal Z, Krebber MM, Vallon V, Touw D, Hoorn EJ, Nieuwdorp M, Kramer MMH, Joles JA, Bjornstad P, van Raalte DH. SGLT2 Inhibition and uric acid excretion in patients with type 2 diabetes and normal kidney function. Clin J Am Soc Nephrol. 2022;17(5):663–71. https://doi.org/10.2215/CJN.11480821.
Acknowledgements
We gratefully thank all the participants in the study.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Funding
No financial support was obtained from any individual, institutions, agencies, drug industries, or organizations.
Completing Interests
The authors have no relevant financial or nonfinancial interests to disclose.
Availability of Data and Material
The datasets used and/or analyzed during this study are available from the corresponding author on reasonable request.
Author Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Shanshan Nie, Yuhang Zhao, Zeying Feng, Yu Cao, and Guoping Yang. Data analysis was performed by Fangfang Ding, Zeying Feng, and Liying Gong. All authors commented on previous versions of the manuscript. The first draft of the manuscript was written by Shanshan Nie, and all authors read and edited the manuscript. All authors read and approved the final manuscript.
Ethics Approval
This is an observational study. The Medical Ethics Committee of the Third Xiangya Hospital has confirmed that no ethical approval and informed consent are required (code number: R18030).
Code Availability
Not applicable.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Nie, S., Zhao, Y., Feng, Z. et al. Effect of Ticagrelor versus Clopidogrel on All-Cause and Cardiovascular Mortality in Acute Coronary Syndrome Patients with Hyperuricemia. Clin Drug Investig 44, 163–174 (2024). https://doi.org/10.1007/s40261-024-01342-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40261-024-01342-6