Abstract
Background and Objective
Adherence to and persistence with inhaled long-acting bronchodilators (ILAB), is commonly considered to be a relevant driver of perceived health-related quality of life (HRQoL) in chronic obstructive pulmonary disease (COPD), but the topic is rarely studied with real-world data. Using survey and health insurance claims data, this study investigates the effect of adherence to and persistence with ILAB on EQ-5D-5L visual analog scale (VAS) in ILAB users who were enrolled in the German disease management programs (DMP) for COPD.
Methods
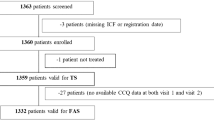
Included ILAB users were aged ≥ 18 years, continuously insured with AOK Bavaria and enrolled in the DMP for COPD. Adherence to ILAB [proportion of days covered (PDC); PDC ≥ 80%], and persistence (days of uninterrupted ILAB therapy) were assessed in the year preceding the study’s HRQoL questionnaire. In a cross-sectional design we applied quasi-Poisson models with log link function and subgroup analyses. The robustness of results was analyzed with comprehensive sensitivity analyses.
Results
Patients with PDC ≥ 80% had 2.96% higher VAS scores than patients with lower PDCs. From all analyses, patients with GOLD stage III had the highest effects from PDC ≥ 80% (5.33% increased VAS). Patients without heart failure profited significantly more from PDC ≥ 80% (+ 4.34% vs − 2.88%) and from an additional persistent day (+ 0.01% vs – 0.01%) than patients with heart failure.
Conclusions
Overall, ILAB users significantly profited from PDC ≥ 80%, but not from continuous PDC or persistent days. In secondary subgroup analyses, patients with GOLD stage III and patients without heart failure particularly profited from PDC ≥ 80%. Only patients without heart failure particularly profited from more persistent days. Because identified effects were small and often not robust, advancing adherence and persistence alone may not improve the German DMP for COPD substantially.


Similar content being viewed by others
References
GOLD. Global strategy for the diagnosis, management, and prevention of COPD. https://goldcopd.org/gold-reports/. Accessed 01 Mar 2021.
Cramer JA, Roy A, Burrell A, Fairchild CJ, Fuldeore MJ, Ollendorf DA, et al. Medication compliance and persistence: terminology and definitions. Value Health. 2008;11(1):44–7.
G-BA. DMP-Anforderungen-Richtlinie. https://www.g-ba.de/richtlinien/83/. Accessed 01 Mar 2021.
G-BA. Disease-Management-Programme. https://www.g-ba.de/themen/disease-management-programme/. Accessed 01 Mar 2021.
Achelrod D, Welte T, Schreyogg J, Stargardt T. Costs and outcomes of the German disease management programme (DMP) for chronic obstructive pulmonary disease (COPD)-A large population-based cohort study. Health Policy (Amsterdam, Netherlands). 2016;120(9):1029–39.
Mehring M, Donnachie E, Fexer J, Hofmann F, Schneider A. Disease management programs for patients with COPD in Germany: a longitudinal evaluation of routinely collected patient records. Respir Care. 2014;59(7):1123–32.
Martin LR, Williams SL, Haskard KB, Dimatteo MR. The challenge of patient adherence. Ther Clin Risk Manag. 2005;1(3):189–99.
van Boven JF, Chavannes NH, van der Molen T, Rutten-van Mölken MP, Postma MJ, Vegter S. Clinical and economic impact of non-adherence in COPD: a systematic review. Respir Med. 2014;108(1):103–13.
Sehl J, O’Doherty J, O’Connor R, O’Sullivan B, O’Regan A. Adherence to COPD management guidelines in general practice? A review of the literature. Irish J Med Sci (1971-). 2018;187(2):403–7.
Mueller S, Wilke T, Bechtel B, Punekar YS, Mitzner K, Virchow JC. Non-persistence and non-adherence to long-acting COPD medication therapy: a retrospective cohort study based on a large German claims dataset. Respir Med. 2017;122:1–11.
George M. Adherence in asthma and COPD: new strategies for an old problem. Respir Care. 2018;63(6):818–31.
Agh T, Domotor P, Bartfai Z, Inotai A, Fujsz E, Meszaros A. Relationship between medication adherence and health-related quality of life in subjects with COPD: a systematic review. Respir Care. 2015;60(2):297–303.
Kirsch F, Schramm A, Schwarzkopf L, Lutter JI, Szentes B, Huber M, et al. Direct and indirect costs of COPD progression and its comorbidities in a structured disease management program: results from the LQ-DMP study. Respir Res. 2019;20(1):1–15.
Kirsch F, Schramm A, Kurz C, Schwarzkopf L, Lutter JI, Huber M, et al. Effect of BMI on health care expenditures stratified by COPD GOLD severity grades: results from the LQ-DMP study. Respir Med. 2020;175:106194.
Huber MB, Kurz C, Kirsch F, Schwarzkopf L, Schramm A, Leidl R. The relationship between body mass index and health-related quality of life in COPD: real-world evidence based on claims and survey data. Respir Res. 2020;21(1):1–10.
Huber MB, Schneider N, Kirsch F, Schwarzkopf L, Schramm A, Leidl R. Long-term weight gain in obese COPD patients participating in a disease management program: a risk factor for reduced health-related quality of life. Respir Res. 2021;22(1):1–9.
Stöber A LJ, Schwarzkopf L, Kirsch F, Schramm A, Vogelmeier C, Leidl R. Impact of clinical changes on health-related quality of life in COPD patients within one year: real world analysis based on claims data. Int J COPD. 2021 (in press).
Euro-Informationen. AOK Bayern. https://www.krankenkassen.de/gesetzliche-krankenkassen/krankenkassen-liste/235-AOK-Bayern.html#kurzportrait. Accessed 26 Feb 2021.
EuroQol. EQ-5D-5L | About. https://euroqol.org/eq-5d-instruments/eq-5d-5l-about/. Accessed 16 Apr 2020.
Vogelmeier C, Buhl R, Burghuber O, Criée C-P, Ewig S, Godnic-Cvar J, et al. Leitlinie zur Diagnostik und Therapie von Patienten mit chronisch obstruktiver Bronchitis und Lungenemphysem (COPD). Pneumologie. 2018;72(04):253–308.
Carls GS, Roebuck MC, Brennan TA, Slezak JA, Matlin OS, Gibson TB. Impact of medication adherence on absenteeism and short-term disability for five chronic diseases. J Occup Environ Med. 2012;54(7):792–805.
Peterson AM, Nau DP, Cramer JA, Benner J, Gwadry-Sridhar F, Nichol M. A checklist for medication compliance and persistence studies using retrospective databases. Value Health. 2007;10(1):3–12.
Lim MT, Ab Rahman N, Teh XR, Chan CL, Thevendran S, Ahmad Hamdi N, et al. Optimal cut-off points for adherence measure among patients with type 2 diabetes in primary care clinics: a retrospective analysis. Therap Adv Chronic Dis. 2021;12:2040622321990264.
Karve S, Cleves MA, Helm M, Hudson TJ, West DS, Martin BC. Good and poor adherence: optimal cut-point for adherence measures using administrative claims data. Curr Med Res Opin. 2009;25(9):2303–10.
Wu JR, Moser DK, De Jong MJ, Rayens MK, Chung ML, Riegel B, et al. Defining an evidence-based cutpoint for medication adherence in heart failure. Am Heart J. 2009;157(2):285–91.
Krack G, Holle R, Kirchberger I, Kuch B, Amann U, Seidl H. Determinants of adherence and effects on health-related quality of life after myocardial infarction: a prospective cohort study. BMC Geriatr. 2018;18(1):136.
Krack G, Zeidler H, Zeidler J. Claims data analysis of tumor necrosis factor inhibitor treatment dosing among patients with rheumatoid arthritis: a systematic review of methods. Drugs-Real World Outcomes. 2016;3(3):265–78.
KVB. Verordnung aktuell—Änderung der Rehabilitations-Richtlinie. www.kvb.de/verordnungen. Accessed 26 Jun 2019.
Zeileis A, Kleiber C, Jackman S. Regression models for count data in R. J Stat Softw. 2008;27(8):1–25.
Grochtdreis T, Dams J, Konig HH, Konnopka A. Health-related quality of life measured with the EQ-5D-5L: estimation of normative index values based on a representative German population sample and value set. Eur J Health Econ. 2019;20(6):933–44.
McCaffrey N, Kaambwa B, Currow DC, Ratcliffe J. Health-related quality of life measured using the EQ-5D-5L: South Australian population norms. Health Qual Life Outcomes. 2016;14(1):133.
Kamangar F. Confounding variables in epidemiologic studies: basics and beyond. Arch Iran Med. 2012;15(8):0.
Quanjer PH, Stanojevic S, Cole TJ, Baur X, Hall GL, Culver BH, et al. Multi-ethnic reference values for spirometry for the 3–95-yr age range: the global lung function 2012 equations. Eur Respir J. 2012;40(6):1324–43.
Schwarzer G, Carpenter JR, Rücker G. Meta-analysis with R. New York: Springer; 2015.
Boland MRS, van Boven JFM, Kruis AL, Chavannes NH, van der Molen T, Goossens LMA, et al. Investigating the association between medication adherence and health-related quality of life in COPD: methodological challenges when using a proxy measure of adherence. Respir Med. 2016;110:34–45.
Bogart M, Stanford RH, Laliberté F, Germain G, Wu JW, Duh MS. Medication adherence and persistence in chronic obstructive pulmonary disease patients receiving triple therapy in a USA commercially insured population. Int J Chron Obstruct Pulmon Dis. 2019;14:343–52.
Corden ZM, Bosley CM, Rees PJ, Cochrane GM. Home nebulized therapy for patients with COPD: patient compliance with treatment and its relation to quality of life. Chest. 1997;112(5):1278–82.
Agh T, Inotai A, Meszaros A. Factors associated with medication adherence in patients with chronic obstructive pulmonary disease. Respiration. 2011;82(4):328–34.
Turner J, Wright E, Mendella L, Anthonisen N. Predictors of patient adherence to long-term home nebulizer therapy for COPD. The IPPB Study Group. Intermittent Positive Pressure Breathing. Chest. 1995;108(2):394–400.
Nolan CM, Longworth L, Lord J, Canavan JL, Jones SE, Kon SS, et al. The EQ-5D-5L health status questionnaire in COPD: validity, responsiveness and minimum important difference. Thorax. 2016;71(6):493–500.
Cook CE. Clinimetrics Corner: the Minimal Clinically Important Change Score (MCID): a necessary pretense. J Man Manip Ther. 2008;16(4):E82–3.
Ariel A, Altraja A, Belevskiy A, Boros PW, Danila E, Fležar M, et al. Inhaled therapies in patients with moderate COPD in clinical practice: current thinking. Int J Chron Obstruct Pulmon Dis. 2017;13:45–56.
Ferguson GT, Pizzichini E, Flezar M, Grönke L, Korducki L. The fixed-dose combination of tiotropium + olodaterol has a rapid onset of action in patients with COPD. Eur Respir J. 2015;46(suppl 59):PA2957.
Mentz RJ, Fiuzat M, Kraft M, Lindenfeld J, O’Connor CM. Bronchodilators in heart failure patients with COPD: is it time for a clinical trial? J Card Fail. 2012;18(5):413–22.
Li G, Taljaard M, Van den Heuvel ER, Levine MA, Cook DJ, Wells GA, et al. An introduction to multiplicity issues in clinical trials: the what, why, when and how. Int J Epidemiol. 2017;46(2):746–55.
Nau DP. Proportion of days covered (PDC) as a preferred method of measuring medication adherence. Springfield: Pharmacy Quality Alliance; 2012.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The project is funded by the Federal Joint Committee (G-BA), Innovation Fund (funding code 01VSF16025).
Competing interests
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
Ethics approval
The ethics committee of the Ludwig Maximilians University, Munich, approved the study (vote no. 17-358).
Consent to participate
Participants provided written informed consent at the time of inclusion in the disease management program.
Consent to publish
Not applicable.
Availability of data and materials
The datasets generated and/or analyzed during the current study are not publicly available and according to the data protection concept approved by the responsible data security officials and the ethics committee.
Code availability
Not applicable.
Author contributions
GK developed the statistical models, analyzed the data, wrote the manuscript, and acted as the corresponding author. FK was responsible for the entire data management of the LQ-DMP study. LS is the study statistician and provided continuous support with regard to methodological questions. RL is principal investigator of the LQ-DMP project and provided advice on content related questions. Supported by AS, LS and RL conceived the study and decided on the research questions to be answered. All coauthors critically commented on earlier manuscript drafts and approved the final version.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Krack, G., Kirsch, F., Schwarzkopf, L. et al. Can Adherence to and Persistence with Inhaled Long-acting Bronchodilators Improve the Quality of Life in Patients with Chronic Obstructive Pulmonary Disease? Results from a German Disease Management Program. Clin Drug Investig 41, 989–998 (2021). https://doi.org/10.1007/s40261-021-01083-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40261-021-01083-w