Abstract
Background
Drug transporters and drug-metabolizing enzymes have been linked to drug-induced hepatotoxicity. Solute carrier organic anion transporter family member 1B1 (SLCO1B1), cytochrome P450 2E1 (CYP2E1), and UDP glucuronosyltransferase 1A1 (UGT1A1) were selected as candidate genes to explore their association with susceptibility to anti-tuberculosis drug-induced hepatotoxicity (ATDH).
Methods
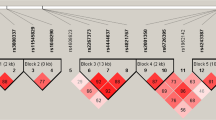
Thirty-four tag single nucleotide polymorphisms (tagSNPs) in SLCO1B1, CYP2E1, and UGT1A1 with 10-kb expansion up- and down-stream were genotyped in 461 patients with ATDH and 466 patients without ATDH in a prospective 1:1 matched case–control study. The frequencies and distributions of genotypes and haplotypes were compared between the groups using three genetic models (dominant, recessive, and additive) to identify associations with susceptibility to ATDH.
Results
Patients with the rs4149034 G/A, rs1564370 G/C, and rs2900478 T/A genotypes of SLCO1B1 had a significantly lower risk of ATDH, while those carrying the rs2417957 T/T and rs4149063 T/T genotypes had an increased risk. The rs4148323 A/A genotype of UGT1A1 was found to significantly reduce the risk of ATDH. Haplotype analysis showed the TGTG, TTTC, and GTTC haplotypes of SLCO1B1 were associated with an increased ATDH risk, whereas the GACC haplotype was related to a reduced risk. The ATG haplotype of UGT1A1 reduced the risk of ATDH. Moreover, treatment outcomes in tuberculosis patients were further affected by genetic variants of SLCO1B1.
Conclusions
Genetic polymorphisms of SLCO1B1 and UGT1A1 were found to be associated with susceptibility to ATDH. Molecular identification of susceptibility genes provides a theoretical foundation for predicting the likelihood of ATDH and predicting treatment outcomes in tuberculosis patients.



Similar content being viewed by others
References
World Health Organization. Global tuberculosis report 2016. (WHO/HTM/TB/2016.13).
Sun Q, Zhang Q, Gu J, et al. Prevalence, risk factors, management, and treatment outcomes of first-line antituberculous drug-induced liver injury: a prospective cohort study. Pharmacoepidemiol Drug Saf. 2016;25:908–17.
Medina-Caliz I, Robles-Diaz M, Garcia-Muñoz B, Spanish DILI registry, et al. Definition and risk factors for chronicity following acute idiosyncratic drug-induced liver injury. J Hepatol. 2016;65(3):532–42.
Chen M, Suzuki A, Borlak J, Andrade RJ, Lucena MI. Drug-induced liver injury: interactions between drug properties and host factors. J Hepatol. 2015;63(2):503–14.
Sharma SK, Balamurugan A, Saha PK, Pandey RM, Mehra NK. Evaluation of clinical and immunogenetic risk factors for the development of hepatotoxicity during antituberculosis treatment. Am J Respir Crit Care Med. 2002;166:916–9.
Shakya R, Rao BS, Shrestha B. Incidence of hepatotoxicity due to antitubercular medicines and assessment of risk factors. Ann Pharmacother. 2004;38:1074–9.
Breen RA, Miller RF, Gorsuch T, et al. Adverse events and treatment interruption in tuberculosis patients with and without HIV co-infection. Thorax. 2006;61:791–4.
Yee D, Valiquette C, Pelletier M, Parisien I, Rocher I, Menzies D. Incidence of serious side effects from first-line antituberculosis drugs among patients treated for active tuberculosis. Am J Respir Crit Care Med. 2003;167:1472–7.
Kim SH, Kim SH, Lee JH, et al. Polymorphisms in drug transporter genes (ABCB1, SLCO1B1 and ABCC2) and hepatitis induced by antituberculosis drugs. Tuberculosis (Edinb). 2012;92(1):100–4.
Chen R, Wang J, Tang S, et al. Association of polymorphisms in drug transporter genes (SLCO1B1 and SLC10A1) and anti-tuberculosis drug-induced hepatotoxicity in a Chinese cohort. Tuberculosis (Edinb). 2015;95(1):68–74.
Guaoua S, Ratbi I, Laarabi FZ, et al. Distribution of allelic and genotypic frequencies of NAT2 and CYP2E1 variants in Moroccan population. BMC Genet. 2014;15:156.
Sharma SK, Jha BK, Sharma A, et al. Genetic polymorphisms of CYP2E1 and GSTM1 loci and susceptibility to anti-tuberculosis drug-induced hepatotoxicity. Int J Tuberc Lung Dis. 2014;18(5):588–93.
Tang SW, Lv XZ, Zhang Y, et al. Cytochrome P450 2E1 gene polymorphisms/haplotypes and anti-tuberculosis drug-induced hepatitis in a Chinese cohort. PLoS One. 2013;8(2):e57526.
Ng CS, Hasnat A, Al Maruf A, et al. N-Acetyltransferase 2 (NAT2) genotype as a risk factor for development of drug-induced liver injury relating to antituberculosis drug treatment in a mixed-ethnicity patient group. Eur J Clin Pharmacol. 2014;70(9):1079–86.
Singla N, Gupta D, Birbian N, Singh J. Association of NAT2, GST and CYP2E1 polymorphisms and anti-tuberculosis drug-induced hepatotoxicity. Tuberculosis (Edinb). 2014;94(3):293–8.
Daly AK. Drug-induced liver injury: past, present and future. Pharmacogenomics. 2010;11(5):607–11.
Zhang K, Qin ZS, Liu JS, Chen T, Waterman MS, Sun F. Haplotype block partitioning and tag SNP selection using genotype data and their applications to association studies. Genome Res. 2004;14:908e16.
Abboud G, Kaplowitz N. Drug-induced liver injury. Drug Saf. 2007;30:277–94.
Aithal GP, Watkins PB, Andrade RJ, et al. Case definition and phenotype standardization in drug-induced liver injury. Clin Pharmacol Ther. 2011;89:806–15.
Danan G, Benichou C. Causality assessment of adverse reactions to drugs. a novel method based on the conclusions of international consensus meetings: application to drug-induced liver injuries. J Clin Epidemiol. 1993;46:1323–30.
Hennig S, Naiker S, Reddy T, et al. Effect of SLCO1B1 polymorphisms on rifabutin phamacokinetics in African HIV-infected patients with tuberculosis. Antimicrob Agents Chemothor. 2015;60(1):617–20.
Weiner M, Peloquin C, Burman W, et al. Effects of tuberculosis, race, and human gene SLCO1B1 polymorphisms on rifampin concentrations. Antimicrob Agents Chemother. 2010;54(10):4192–200.
Bins S, Lenting A, El Bouazzaoui S, et al. Polymorphisms in SLCO1B1 and UGT1A1 are associated with sorafenib-induced toxicity. Pharmacogenomics. 2016;17(14):1483–90.
Tostmann A, Boeree MJ, Aarnoutse RE, de Lange WC, van der Ven AJ, Dekhuijzen R. Antituberculosis drug-induced hepatotoxicity: concise up-to-date review. Gastroenterol Hepatol. 2008;232:192–202.
Bose PD, Sarma MP, Medhi S, Das BC, Husain SA, Kar P. Role of polymorphic N-acetyl transferase2 and cytochrome P4502E1 gene in antituberculosis treatment-induced hepatitis. J Gastroenterol Hepatol. 2011;26:312–8.
Sheng YJ, Wu G, He HY, Chen W, Zou YS, Li Q, Zhong L, Huang YM, Deng CL. The association between CYP2E1 polymorphisms and hepatotoxicity due to anti-tuberculosis drugs: a meta-analysis. Infect Genet Evolut. 2014;24:34–40.
Kim JY, Cheong HS, Park BL, Kim LH, Namgoong S, Kim JO, Kim HD, Kim YH, Chung MW, Han SY, Shin HD. Comprehensive variant screening of the UGT gene family. Yonsei Med J. 2014;55(1):232–9.
Gagné JF, Montminy V, Belanger P, Journault K, Gaucher G, Guillemette C. Common human UGT1A polymorphisms and the altered metabolism of irinotecan active metabolite 7-ethyl-10-hydroxycamptothecin (SN-38). Mol Pharmacol. 2002;62(3):608–17.
Chang JC, Liu EH, Lee CN, et al. UGT1A1 polymorphisms associated with risk of induced liver disorders by anti-tuberculosis medication. Int J Tuberc Lung Dis. 2012;16(3):376–8.
Chen R, Wang J, Tang SW, et al. CYP7A1, BAAT and UGT1A1 polymorphisms and susceptibility to anti-tuberculosis drug-induced hepatotoxicity. Int J Tuberc Lung Dis. 2016;20(6):812–8.
Acknowledgements
We specially acknowledge the technical assistance from Genesky Biotechnologies Inc. Shanghai, China. We also thank Medjaden Bioscience Limited for assisting in the preparation of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was supported by the National Nature Science Foundation of China (no. 81400006), the Shanghai Pujiang Program (no. 16PJD041), and the National Science and Technology Major Program (no. 2014ZX09507008).
Conflict of interest
The authors declare no conflict of interest.
Ethics approval
The present study was approved by the Ethics Committees of both Tongji University School of Medicine and Shanghai Pulmonary Hospital.
Informed consent
Written informed consent was received from patients.
Rights and permissions
About this article
Cite this article
Sun, Q., Liu, Hp., Zheng, Rj. et al. Genetic Polymorphisms of SLCO1B1, CYP2E1 and UGT1A1 and Susceptibility to Anti-Tuberculosis Drug-Induced Hepatotoxicity: A Chinese Population-Based Prospective Case–Control Study. Clin Drug Investig 37, 1125–1136 (2017). https://doi.org/10.1007/s40261-017-0572-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40261-017-0572-6