Abstract
Objective
Given increasing patient populations, general practitioner (GP) workforce constraints and increasing demand for health services in New Zealand (NZ), the development and provision of pharmacist prescribing services may need to increase to improve people’s access to medicines. A discrete choice experiment (DCE) was utilised to determine community pharmacist preferences for prescribing services in primary care in NZ, and to understand how these factors could improve the provision of pharmacist prescribing services.
Methods
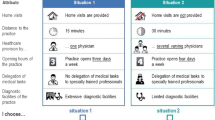
A D-efficient design generated 30 labelled choice questions in three blocks of ten, and three alternatives per choice question. The online DCE was emailed to practising community pharmacists in NZ. The DCE included two attributes with five levels (prescribing model, educational requirements) and three attributes with three levels (location, professional fee, change in income). A mixed multinomial logit model was used to estimate preferences.
Results
A total of 264 respondents completed the survey with 2640 observations for analyses. This DCE found pharmacists preferred pharmacy services with the following characteristics: ability to prescribe using minor ailments and independent prescribing models relative to the pharmacist-only medicines prescribing model; prescribing education by accredited learning modules relative to PGDipClinPharm + PGCertPharmPres; remuneration via a professional fee; and pharmacist prescribing services located in community pharmacies rather than in GP practices.
Conclusions
Prescribing policy could incorporate these pharmacist preferences to help develop accessible and effective pharmacist prescribing services that not only improve access to medicines, but also address inequity of access to medicines in NZ. These DCE results are encouraging as they signal that the community pharmacists also see themselves and their pharmacies as part of the prescribing team in primary care in NZ.

Similar content being viewed by others
References
Cope LC, Abuzour AS, Tully MP. Nonmedical prescribing: where are we now? Ther Adv Drug Saf. 2016;7(4):165–72.
Weeks G, George J, Maclure K, Stewart D. Non-medical prescribing versus medical prescribing for acute and chronic disease management in primary and secondary care. Cochrane Database Syst Rev. 2016;11(11):CD01127. https://doi.org/10.1002/14651858.CD011227.pub2.
Carswell S, Donovan E, Pimm F. Equitable access to medicines via primary healthcare –a review of the literature. PHARMAC. 2018. https://www.pharmac.govt.nz/assets/equitable-access-to-medicines-literature-review.pdf. Accessed 10 Apr 2020.
i5 Health. Non-Medical Prescribing (NMP) An Economic Evaluation. NHS Health Education North West. December 2015. https://www.i5health.com/NMP/NMPEconomicEvaluation.pdf. Accessed 5 Oct 2018.
Latter S, Blenkinsopp A, Smith A, Chapman S, Tinelli M, Gerard K et al. Evaluation of nurse and pharmacist independent prescribing. University of Southampton; Keele University, Department of Health Policy. October 2010
Raghunandan R, Tordoff J, Smith A. Non-medical prescribing in New Zealand: an overview of prescribing rights, service delivery models and training. Ther Adv Drug Saf. 2017;8(11):349–60. https://doi.org/10.1177/2042098617723312.
Nursing Council of New Zealand. The Nursing Council of New Zealand Annual Report 2018. https://www.nursingcouncil.org.nz/Public/Publications/Annual_report/NCNZ/publications-section/Annual_reports.aspx?hkey=8e07d135-7e88-4024-9a2e-4d55e2900eef. Accessed 1 Oct 2019.
Pharmacy Council of New Zealand. Workforce Demographic Report 2018. https://www.pharmacycouncil.org.nz/news-and-publications/workforce-demographics/. Accessed 1 Oct 2019.
Metcalfe S, Beyene K, Urlich J, Jones R, Proffitt C, Harrison J, et al. Te Wero tonu-the challenge continues: Maori access to medicines 2006/07-2012/13 update. NZ Med J. 2018;131(1485):27–47.
Lancsar E, Louviere J. Conducting discrete choice experiments to inform healthcare decision making. PharmacoEconomics. 2008;26(8):661–77. https://doi.org/10.2165/00019053-200826080-00004.
Hensher DA, Rose JM, Greene WH. Applied choice analysis. 2nd ed. Cambridge: Cambridge University Press; 2015.
Rose JM, Bliemer MCJ. Constructing efficient stated choice experimental designs. Transp Rev. 2009;29(5):587–617. https://doi.org/10.1080/01441640902827623.
Johnson FR, Lancsar E, Marshall D, Kilambi V, Muhlbacher A, Regier DA, et al. Constructing experimental designs for discrete-choice experiments: report of the ISPOR Conjoint Analysis Experimental Design Good Research Practices Task Force. Value Health. 2013;16(1):3–13. https://doi.org/10.1016/j.jval.2012.08.2223.
Hauber AB, Gonzalez JM, Groothuis-Oudshoorn CG, Prior T, Marshall DA, Cunningham C, et al. Statistical methods for the analysis of discrete choice experiments: a Report of the ISPOR Conjoint Analysis Good Research Practices Task Force. Value Health. 2016;19(4):300–15. https://doi.org/10.1016/j.jval.2016.04.004.
Famiyeh IM, McCarthy L. Pharmacist prescribing: A scoping review about the views and experiences of patients and the public. Res Soc Admin Pharm RSAP. 2017;13(1):1–16. https://doi.org/10.1016/j.sapharm.2016.01.002.
Whitty JA, Kendall E, Sav A, Kelly F, McMillan SS, King MA, et al. Preferences for the delivery of community pharmacy services to help manage chronic conditions. Res Soc Admin Pharm RSAP. 2015;11(2):197–21515. https://doi.org/10.1016/j.sapharm.2014.06.007.
Grindrod KA, Marra CA, Colley L, Tsuyuki RT, Lynd LD. Pharmacists' preferences for providing patient-centered services: a discrete choice experiment to guide health policy. Ann Pharmacother. 2010;44(10):1554–64. https://doi.org/10.1345/aph.1P228.
Munger MA, Walsh M, Godin J, Feehan M. Pharmacist’s demand for optimal primary care service delivery in a community pharmacy: the OPTiPharm study. Ann Pharmacother. 2017;51(12):1069–76. https://doi.org/10.1177/1060028017722795.
Vass C, Gray E, Payne K. Discrete choice experiments of pharmacy services: a systematic review. Int J Clin Pharm. 2016;38(3):620–30. https://doi.org/10.1007/s11096-015-0221-1.
Naik-Panvelkar P, Armour C, Saini B. Discrete choice experiments in pharmacy: a review of the literature. Int J Pharm Pract. 2013;21(1):3–19. https://doi.org/10.1111/ijpp.12002.
Bliemer MCJ, Rose JM, Beck M, editors. Generating partial choice set designs for stated choice experiments. Annual Meeting of the International Association on Travel Behaviour Research 2018; Santa Barbara CA, USA.
ChoiceMetrics. Ngene V1.1.2. www.choice-metrics.com. Accessed 1 Aug 2017
Bliemer MCJ, Rose JM. Construction of experimental designs for mixed logit models allowing for correlation across choice observations. Transp Res Part B Methodol. 2010;44(6):720–34. https://doi.org/10.1016/j.trb.2009.12.004.
ChoiceMetrics. Ngene v1.1.2 User Manual & Reference Guide. Sydney, Australia: 2014.
R Core Team. A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing. https://www.R-project.org/. Accessed 18 Sept 2019.
Econometric Software. NLOGIT Version 6. Castle Hill, NSW, Australia. https://www.limdep.com/products/nlogit/. Accessed 19 Apr 2018.
van de Pol JM, Koster ES, Hövels AM, Bouvy ML. How community pharmacists prioritize cognitive pharmaceutical services. Res in Soc Admin Pharm. 2019;15(9):1088–94. https://doi.org/10.1016/j.sapharm.2018.09.012.
Scott A, Bond C, Inch J, Grant A. Preferences of community pharmacists for extended roles in primary care. PharmacoEconomics. 2007;25(9):783–92. https://doi.org/10.2165/00019053-200725090-00006.
Inch J, Bond CM, Lee AJ, Scott A, Grant AM. Scottish community pharmacists' current involvement in and attitudes towards ‘extended service’ provision: a national survey. Int J Pharm Pract. 2005;13(4):289–301. https://doi.org/10.1211/ijpp.13.4.0008.
Lo C, Tran Y, Anderson K, Craig A, Middleton J. Functional priorities in persons with spinal cord injury: using discrete choice experiments to determine preferences. J Neurotrauma. 2016;33(21):1958–68. https://doi.org/10.1089/neu.2016.4423.
Muhlbacher A, Johnson FR. Choice experiments to quantify preferences for health and healthcare: state of the practice. Appl Health Econ Health Policy. 2016;14(3):253–66. https://doi.org/10.1007/s40258-016-0232-7.
Robinson J. The trials and triumphs of pharmacist independent prescribers. Pharm J. 2018. https://doi.org/10.1211/PJ.2018.20204489.
Milligan S, Kennedy G. To what degree? Alternative micro-credentialing in a digital age. In: James R, French S, Kelly P, editors. Visions for Australian tertiary education Melbourne: Melbourne Centre for the Study of Higher Education. Parkville: The University of Melbourne; 2017. p. 41–54.
Elliot R, Clayton J, Iwata J. Exploring the use of micro-credentialing and digital badges in learning environments to encourage motivation to learn and achieve. In: Hegarty B, McDonald J, Loke S-K, editors. ASCILITE rhetoric and reality: critical perspectives on educational technology, Dunedin, New Zealand; 2014. p. 703–7.
Makowsky MJ, Guirguis LM, Hughes CA, Sadowski CA, Yuksel N. Factors influencing pharmacists' adoption of prescribing: qualitative application of the diffusion of innovations theory. Implement Sci. 2013;8:109. https://doi.org/10.1186/1748-5908-8-109.
Law MR, Ma T, Fisher J, Sketris IS. Independent pharmacist prescribing in Canada. Can Pharm J Revue Pharm Can. 2012;145(1):17–23.e1. https://doi.org/10.3821/1913-701x-145.1.17.
Paudyal V, Watson MC, Sach T, Porteous T, Bond CM, Wright DJ, et al. Are pharmacy-based minor ailment schemes a substitute for other service providers? A systematic review. Br J Gen Pract. 2013;63(612):e472–e481481. https://doi.org/10.3399/bjgp13X669194.
PricewaterhouseCoopers. The value of community pharmacy—summary report PSNC.September 2016. https://psnc.org.uk/wp-content/uploads/2016/09/The-value-of-community-pharmacy-summary-report.pdf. Accessed 20 Oct 2019.
Mansell K, Bootsman N, Kuntz A, Taylor J. Evaluating pharmacist prescribing for minor ailments. Int J Pharm Pract. 2015;23(2):95–101. https://doi.org/10.1111/ijpp.12128.
Rosenthal M, Austin Z, Tsuyuki RT. Are pharmacists the ultimate barrier to pharmacy practice change? Can Pharm J Revue Pharm Can. 2010;143(1):37–42. https://doi.org/10.3821/1913-701x-143.1.37.
Al Hamarneh YN, Johnston K, Marra CA, Tsuyuki RT. Pharmacist prescribing and care improves cardiovascular risk, but is it cost-effective? A cost-effectiveness analysis of the R(x)EACH study. Can Pharm J (Ott). 2019;152(4):257–66. https://doi.org/10.1177/1715163519851822.
Beahm NP, Smyth DJ, Tsuyuki RT. Outcomes of Urinary Tract Infection Management by Pharmacists (RxOUTMAP): a study of pharmacist prescribing and care in patients with uncomplicated urinary tract infections in the community. Can Pharm J Revue Pharm Can. 2018;151(5):305–14. https://doi.org/10.1177/1715163518781175.
Pharmacy Council of New Zealand. Pharmacy Council takes “right touch” regulatory approach for prescriber qualification. 24 July 2019. https://www.pharmacycouncil.org.nz/dnn_uploads/Media%2520Release%2520Pharmacist%2520prescriber%2520July%25202019.pdf?ver=2019-07-24-035706-667. Accessed 30 July 2019.
Acknowledgements
The authors would like to acknowledge and thank Professor Michiel Bliemer (MSc, PhD), who provided experiment design advice. We thank the pharmacists who participated in the study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This research was supported by a PhD scholarship from the University of Otago, New Zealand.
Conflict of interest
The authors declare no competing interests.
Ethics approval
This study was approved by the University of Otago Human Ethics Committee (reference D17/403).
Consent to participate:
All participants were provided with participant information when they entered the online survey and consented to participate in the study.
Consent to publish
All participants were provided with participant information when they entered the online survey and consented to publication of the results of this study.
Availability of data and material (data transparency)
The data sets generated and analysed during this study are not publicly available due to constraints imposed in the Ethics process, but are available from the corresponding author on reasonable request subject to approval.
Code availability (software or custom code)
Not applicable.
Author contributions
RR designed the DCE (with advice from Prof. Michiel Bliemer) and carried out data collection. RR performed the analyses with supervision from KH; AS, CM and JT supervised the project, providing overall direction and planning. All authors contributed to the final manuscript by providing critical feedback and helping shape the research, analysis and writing of the manuscript.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Raghunandan, R., Howard, K., Marra, C.A. et al. Identifying Community Pharmacist Preferences For Prescribing Services in Primary Care in New Zealand: A Discrete Choice Experiment. Appl Health Econ Health Policy 19, 253–266 (2021). https://doi.org/10.1007/s40258-020-00615-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40258-020-00615-3