Abstract
Vascular malformations are inborn errors of vascular morphogenesis and consist of localized networks of abnormal blood and/or lymphatic vessels with weak endothelial cell proliferation. They have historically been managed by surgery and sclerotherapy. Extensive insight into the genetic origin and molecular mechanism of development has been accumulated over the last 20 years. Since the discovery of the first somatic mutations in a vascular anomaly 10 years ago, it is now recognized that they are perhaps all caused by inherited or somatic mutations in genes that hyperactivate two major intracellular signaling pathways: the RAS/MAPK/ERK and/or the phosphatidylinositol 3 kinase (PIK3)/protein kinase B/mammalian target of rapamycin (mTOR) pathway. Several targeted molecular inhibitors of these pathways have been developed, mostly for the treatment of cancers that harbor mutations in the same pathways. The mTOR inhibitor sirolimus is the most studied compound for the treatment of venous, lymphatic, and complex malformations. Disease responses of vascular malformations to sirolimus have now been reported in several studies in terms of clinical changes, quality of life, functional and radiological outcomes, and safety. Other targeted treatment strategies, such as the PIK3CA inhibitor alpelisib for PIK3CA-mutated vascular malformations, are also emerging. Repurposing of cancer drugs has become a major focus in this rapidly evolving field.

Similar content being viewed by others
References
Mulliken JB, Glowacki J. Hemangiomas and vascular malformations in infants and children: a classification based on endothelial characteristics. Plast Reconstr Surg. 1982;69(3):412–22.
Wassef M, Blei F, Adams D, Alomari A, Baselga E, Berenstein A, ISSVA Board, and Scientific Committee, et al. Vascular anomalies classification: recommendations from the International Society for the Study of Vascular Anomalies. Pediatrics. 2015;136(1):e203–e214214.
International Society for the Study of Vascular Anomalies. Classification of vascular anomalies. 2018. Available from: https://issva.org/classification. Accessed 20 Nov 2019.
Boon LM, Ballieuzx F, Vikkula M. Vascular malformations. In: Kang S, Amagai M, Bruckner AL, Enk AH, Margolis DJ, McMichael AJ, et al., editors. Fitzpatrick’s dermatology. 9th ed. New York: McGraw-Hill Education/Medical; 2019. p. 2636–2638.
Boon LM, Vikkula M. Vascular malformations. In: Hoeger P, Kinsler V, Yan A, Harper J, Oranje A, et al., editors. Harper’s textbook of pediatric dermatology. Wiley: New York; 2019. p. 1399–1424.
Ricci KW. Advances in the medical management of vascular anomalies. Semin Intervent Radiol. 2017;34(3):239–49.
Revencu N, Boon LM, Vikkula M. Capillary malformation/arteriovenous malformation. In: Pyeritz RE, Korf BR, Grody WW, editors. Emery and Rimoin’s principles and practice of medical genetics and genomics. 7th ed. San Diego: Academic Press; 2019. p. 261–266.
Rodriguez-Laguna L, Agra N, Ibañez K, Oliva-Molina G, Gordo G, Khurana N, et al. Somatic activating mutations in PIK3CA cause generalized lymphatic anomaly. J Exp Med. 2019;216(2):407–18.
Brouillard P, Limaye N, Boon LM, Vikkula M. Disorders of the venous system. In: Pyeritz RE, Korf BR, Grody WW, editors. Emery and Rimoin’s principles and practice of medical genetics and genomics. 7th ed. San Diego: Academic Press; 2019. p. 251–260.
Sadick M, Wüller-Wille R, Wildgruber M, Wohlgemuth WA. Vascular anomalies (part I): classification and diagnostics of vascular anomalies. Rofo. 2018;190(9):825–35.
Brouillard P, Vikkula M. Vascular malformations: localized defects in vascular morphogenesis. Clin Genet. 2003;63(5):340–51.
Limaye N, Uebelhoer M, Tuominen M, Wirkkala R, Mulliken JB, Eklund L, et al. Somatic mutations in angiopoietin receptor gene TEK cause solitary and multiple sporadic venous malformations. Nat Genet. 2009;41(1):118–24.
Vikkula M, Boon LM, Carraway KL 3rd, Calvert JT, Diamonti AJ, Goumnerov B, et al. Vascular dysmorphogenesis caused by an activating mutation in the receptor tyrosine kinase TIE2. Cell. 1996;87(7):1181–90.
Nguyen HL, Boon LM, Vikkula M. Vascular anomalies caused by abnormal signaling within endothelial cells: targets for novel therapies. Semin Intervent Radiol. 2017;34(3):233–8.
Seront E, Van Damme A, Boon LM, Vikkula M. Rapamycin and treatment of venous malformations. Curr Opin Hematol. 2019;26(3):185–92.
Soblet J, Kangas J, Nätynki M, Mendola A, Helaers R, Uebelhoer M, et al. Blue rubber bleb nevus (BRBN) syndrome is caused by somatic TEK (TIE2) mutations. J Invest Dermatol. 2017;137(1):207–16.
Wouters V, Limaye N, Uebelhoer M, Irrthum A, Boon LM, Mulliken JB, et al. Hereditary cutaneomucosal venous malformations are caused by TIE2 mutations with widely variable hyper-phosphorylating effects. Eur J Hum Genet. 2010;18(4):414–20.
Soblet J, Limaye N, Uebelhoer M, Boon LM, Vikkula M. Variable somatic TIE2 mutations in half of sporadic venous malformations. Mol Syndromol. 2013;4(4):179–83.
Limaye N, Kangas J, Mendola A, Godfraind C, Schlögel MJ, Helaers R, et al. Somatic activating PIK3CA mutations cause venous malformation. Am J Hum Genet. 2015;97(6):914–21.
Nätynki M, Kangas J, Miinalainen I, Sormunen R, Pietilä R, Soblet J, et al. Common and specific effects of TIE2 mutations causing venous malformations. Hum Mol Genet. 2015;24(22):6374–89.
Karakas B, Bachman KE, Park BH. Mutation of the PIK3CA oncogene in human cancers. Br J Cancer. 2006;94(4):455–9.
Castillo SD, Tzouanacou E, Zaw-Thin M, Berenjeno IM, Parker VE, Chivite I, et al. Somatic activating mutations in PIK3CA cause sporadic venous malformations in mice and humans. Sci Transl Med. 2016;8(332):332ra43.
Luks VL, Kamitaki N, Vivero MP, Uller W, Rab R, Bovée JV, et al. Lymphatic and other vascular malformative/overgrowth disorders are caused by somatic mutations in PIK3CA. J Pediatr. 2015;166(4):1048–54.
Cheraghlou S, Lim Y, Choate K. Genetic investigation of childhood vascular tumor biology reveals pathways for therapeutic intervention. F1000Res. 2019;8:F1000 Faculty Rev-590.
Lim YH, Bacchiocchi A, Qiu J, Straub R, Bruckner A, Bercovitch L, et al. GNA14 somatic mutation causes congenital and sporadic vascular tumors by MAPK activation. Am J Hum Genet. 2016;99(2):443–50.
Shirley MD, Tang H, Gallione CJ, Baugher JD, Frelin LP, Cohen B, et al. Sturge-Weber syndrome and port-wine stains caused by somatic mutation in GNAQ. N Engl J Med. 2013;368(21):1971–9.
Couto JA, Huang AY, Konczyk DJ, Goss JA, Fishman SJ, Mulliken JB, et al. Somatic MAP2K1 mutations are associated with extracranial arteriovenous malformation. Am J Hum Genet. 2017;100(3):546–54.
Nikolaev SI, Vetiska S, Bonilla X, Boudreau E, Jauhiainen S, Rezai Jahromi B, et al. Somatic activating KRAS mutations in arteriovenous malformations of the brain. N Engl J Med. 2018;378(3):250–61.
Lim YH, Douglas SR, Ko CJ, Antaya RJ, McNiff JM, Zhou J, et al. Somatic activating RAS mutations cause vascular tumors including pyogenic granuloma. J Invest Dermatol. 2015;135(6):1698–700.
Dekeuleneer V, Seront E, Van Damme A, Boon LM, Vikkula M. Theranostic advances in vascular malformations. J Invest Dermatol. 2020 (in press).
Nadal M, Giraudeau B, Tavernier E, Jonville-Bera AP, Lorette G, Maruani A. Efficacy and safety of mammalian target of rapamycin inhibitors in vascular anomalies: a systematic review. Acta Derm Venereol. 2016;96(4):448–52.
Boscolo E, Limaye N, Huang L, Kang KT, Soblet J, Uebelhoer M, et al. Rapamycin improves TIE2-mutated venous malformation in murine model and human subjects. J Clin Invest. 2015;125(9):3491–504.
Hammill AM, Wentzel MS, Gupta A, Nelson S, Lucky A, Elluru R, et al. Sirolimus for the treatment of complicated vascular anomalies in children. Pediatr Blood Cancer. 2011;57:1018–24.
Triana P, Dore M, Cerezo VN, Cervantes M, Sánchez AV, Ferrero MM, et al. Sirolimus in the treatment of vascular anomalies. Eur J Pediatr Surg. 2017;27(1):86–90.
Lackner H, Karastaneva A, Schwinger W, Benesch M, Sovinz P, Seidel M, et al. Sirolimus for the treatment of children with various complicated vascular anomalies. Eur J Pediatr. 2015;174(12):1579–84.
Tole S, Fantauzzi M, Cottingham D, Amaral JG, John PR, Lara-Corrales I, et al. The use of rapamycin to treat vascular tumours and malformations: a single-centre experience. Paediatr Clin Health. 2019. https://doi.org/10.1093/pch/pxz090.
Yesil S, Tanyildiz HG, Bozkurt C, Cakmakci E, Sahin G. Single-center experience with sirolimus therapy for vascular malformations. Pediatr Hematol Oncol. 2016;33(3):219–25.
Salloum R, Fox CE, Alvarez-Allende CR, Hammill AM, Dasgupta R, Dickie BH, et al. Response of blue rubber bleb nevus syndrome to sirolimus treatment. Pediatr Blood Cancer. 2016;63(11):1911–4.
Mack JM, Verkamp B, Richter GT, Nicholas R, Stewart K, Crary SE. Effect of sirolimus on coagulopathy of slow-flow vascular malformations. Pediatr Blood Cancer. 2019;66(10):e27896.
Isoldi S, Belsha D, Yeop I, Uc A, Zevit N, Mamula P, et al. Diagnosis and management of children with blue rubber bleb nevus syndrome: a multi-center case series. Dig Liver Dis. 2019;51(11):1537–46.
Vlahovic AM, Vlahovic NS, Haxhija EQ. Sirolimus for the treatment of a massive capillary-lymphatico-venous malformation: a case report. Pediatrics. 2015;136(2):e513–e516516.
Akyüz C, Atas E, Varan A. Treatment of a tongue lymphangioma with sirolimus after failure of surgical resection and propranolol. Pediatr Blood Cancer. 2014;61:931–2.
Iacobas I, Simon ML, Amir T, Gribbin CE, McPartland TG, Kaufman MR, et al. Decreased vascularization of retroperitoneal kaposiform hemangioendothelioma induced by treatment with sirolimus explains relief of symptoms. Clin Imaging. 2015;39(3):529–32.
Wang Z, Li K, Dong K, Xiao X, Zheng S. Successful treatment of Kasabach-Merritt phenomenon arising from kaposiform hemangioendothelioma by sirolimus. J Pediatr Hematol Oncol. 2015;37(1):72–3.
Oza VS, Mamlouk MD, Hess CP, Mathes EF, Frieden IJ. Role of sirolimus in advanced kaposiform hemangioendothelioma. Pediatr Dermatol. 2016;33(2):e88–92.
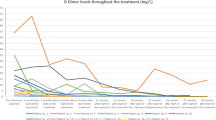
Adams DM, Trenor CC 3rd, Hammill AM, Vinks AA, Patel MN, Chaudry G, et al. Efficacy and safety of sirolimus in the treatment of complicated vascular anomalies. Pediatrics. 2016;137(2):e20153257.
Hammer J, Seront E, Duez S, Dupont S, Van Damme A, Schmitz S, et al. Sirolimus is efficacious in treatment for extensive and/or complex slow-flow vascular malformations: a monocentric prospective phase II study. Orphanet J Rare Dis. 2018;13(1):191.
Kahan BD, Napoli KL, Kelly PA, et al. Therapeutic drug monitoring of sirolimus: correlations with efficacy and toxicity. Clin Transplant. 2000;14(2):97–109.
Scott JR, Courter JD, Saldana SN, et al. Population pharmacokinetics of sirolimus in pediatric patients with neurofibromatosis type 1. Ther Drug Monit. 2013;35(3):332–7.
Emoto C, Fukuda T, Mizonu T, Schniedewind B, Christians U, Adams DM, et al. Characterizing the developmental trajectory of sirolimus clearance in neonates and infants. CPT Pharmacometr Syst Pharmacol. 2016;5(8):411–7.
Mizuno T, Fukuda T, Emoto C, Mobberley-Schuman PS, Hammill AM, Adams DM, et al. Developmental pharmacokinetics of sirolimus: implications for precision dosing in neonates and infants with complicated vascular anomalies. Pediatr Blood Cancer. 2017. https://doi.org/10.1002/pbc.26470.
Mizuno T, Emoto C, Fukuda T, Hammill AM, Adams DM, Vinks AA. Model-based precision dosing of sirolimus in pediatric patients with vascular anomalies. Eur J Pharm Sci. 2017;109S:S124–S131131.
Shimobayashi M, Hall MN. Making new contacts: the mTOR network in metabolism and signalling crosstalk. Nat Rev Mol Cell Biol. 2014;15(3):155–62.
Sharma A, Schwartz RA. Stewart-Treves syndrome: pathogenesis and management. J Am Acad Dermatol. 2012;67(6):1342–8.
Ventura-Aguiar P, Campistol JM, Diekmann F. Safety of mTOR inhibitors in adult solid organ transplantation. Expert Opin Drug Saf. 2016;15(3):303–19.
MacDonald AS, RAPAMUNE Global Study Group. A worldwide, phase III, randomized, controlled, safety and efficacy study of a sirolimus/cyclosporine regimen for prevention of acute rejection in recipients of primary mismatched renal allografts. Transplantation. 2001;71(2):271–80.
Basic-Jukic N, Kes P, Bubic-Filipi L, Vranjican Z. Rhabdomyolysis and acute kidney injury secondary to concomitant use of fluvastatin and rapamycin in a renal transplant recipient. Nephrol Dial Transplant. 2010;25(6):2036.
Stallone G, Infante B, Di Lorenzo A, Rascio F, Zaza G, Gandaliano G. mTOR inhibitors effects on regulatory T cells and on dendritic cells. J Transl Med. 2016;14(1):152.
Augustine JJ, Bodziak KA, Hricik DE. Use of sirolimus in solid organ transplantation. Drugs. 2017;67(3):369–91.
De Castro N, Xu F, Porcher R, Pavie J, Molina JM, Peraldi MN. Pneumoncystis jirovecii pneumonia in renal transplant recipients occurring after discontinuation of prophylaxis: a case-control study. Clin Microbiol Infect. 2010;16(9):1375–7.
Saito Y, Nagayama M, Miura Y, Ogushi S, Suzuki Y, Noro R, et al. A case of Pneumocystis pneumonia associated with everolimus therapy for renal cell carcinoma. Jpn J Clin Oncol. 2013;43(5):559–62.
Kuik KT, Trubiano J, Worth LJ, Harun NS, Steinfort D, Johnson D. Pneumocystic jirovecii pneumonia following everolimus treatment of metastatic breast cancer. Med Mycol Case Rep. 2014;16:34–6.
Overwater IE, Rietman AB, Bindels-de Heus K, Looman CW, Rizopoulos D, Sibindi TM, et al. Sirolimus for epilepsy in children with tuberous sclerosis complex: a randomized controlled trial. Neurology. 2016;87(10):1011–8.
Hu YN, Lee NY, Roan JN, Hsu CH, Luo CY. High-dose calcineurin inhibitor-free everolimus as a maintenance regimen for heart transplantation may be a risk factor for Pneumocystis pneumonia. Transpl Infect Dis. 2017. https://doi.org/10.1111/tid.12709.
Krueger DA, Capal JK, Curatolo P, Devinsky O, Ess K, Tzadok M, TSCure Research Group, et al. Short-term safety of mTOR inhibitors in infants and very young children with tuberous sclerosis complex (TSC): multicentre clinical experience. Eur J Paediatr Neurol. 2018;22(6):1066–73.
Russel TB, Rinker EK, Dillingham CS, Givner LB, McLean TW. Pneumocystis jirovecii pneumonia during sirolimus therapy for kaposiform hemangioendothelioma. Pediatrics. 2018;41(Suppl. 5):S421–S424424.
Ying H, Qiao C, Yang X, Lin X. A case report of 2 sirolimus-related deaths among infants with kaposiform hemangioendotheliomas. Pediatrics. 2018;141(Suppl 5):S425–S429429.
Li M, Zhou Y, Chen C, Yang T, Zhou S, Chen S, et al. Efficacy and safety of mTOR inhibitors (rapamycin and its analogues) for tuberous sclerosis complex: a meta-analysis. Orphanet J Rare Dis. 2019;14(1):39.
Ghadimi M, Mohammadpour Z, Dashti-Khavidaki S, Milajerdi A. m-TOR inhibitors and risk of Pneumocystis pneumonia after solid organ transplantation: a systematic review and meta-analysis. Eur J Clin Pharmacol. 2019;75(11):1471–80.
Goldberg H, Harari S, Cottin V, Rosas IO, Peters E, Biswal S, et al. Everolimus for the treatment of lymphangioleiomyomatosis: a phase II study. Eur Respir J. 2015;46:783–94.
Matsumoto H, Ozeki M, Hori T, Kanda K, Kawamoto N, Nagano A, et al. Successful everolimus treatment of kaposiform hemangioendothelioma with Kasabach-Merritt phenomenon: clinical efficacy and adverse effects of mTOR inhibitor therapy. J Pediatr Hematol Oncol. 2016;38(8):e322–e325.
Jenkins D, McCuaig C, Drolet BA, Siegel D, Adams S, Lawson JA, et al. Tuberous sclerosis complex associated with vascular anomalies or overgrowth. Pediatr Dermatol. 2016;33(5):536–42.
Wiemer-Kruel A, Mayer H, Ewert P, Martinoff S, Eckstein H, Kriebel T, et al. Congenital lymphatic malformation and aortic aneurysm in a patient with TSC2 mutation. Neuropediatrics. 2020;51(1):57–61.
Parker VER, Keppler-Noreuil KM, Faivre L, Luu M, Oden NL, De Silva L, et al. Safety and efficacy of low-dose sirolimus in the PIK3CA-related overgrowth spectrum. Genet Med. 2019;21(5):1189–98.
López Gutiérrez JC, Lizarraga R, Delgado C, Martínez Urrutia MJ, Díaz M, Miguel M, et al. Alpelisib treatment for genital vascular malformation in a patient with congenital lipomatous overgrowth, vascular malformations, epidermal nevi, and spinal/skeletal anomalies and/or scoliosis (CLOVES) syndrome. J Pediatr Adolesc Gynecol. 2019;32(6):648–50.
Parker VER, Keppler-Noreuil KM, Faivre L, Luu M, Oden NL, De Silva L, PROMISE Working Group, et al. Safety and efficacy of low-dose sirolimus in the PIK3CA-related overgrowth spectrum. Genet Med. 2019;21(5):1189–98.
Mayer IA, Abramson VG, Formisano L, Balko JM, Estrada MV, Sanders ME, et al. A phase Ib study of alpelisib (BYL719), a PI3Kα inhibitor, with letrozole in ER+/HER2-negative metastatic breast cancer. Clin Cancer Res. 2017;23(1):26–34.
Ando Y, Iwasa S, Takahashi S, Saka H, Kakizume T, Natsume K, et al. Phase I study of alpelisib (BYL719), an α-specific PI3K inhibitor, in Japanese patients with advanced solid tumors. Cancer Sci. 2019;110(3):1021–31.
Markham A. Alpelisib: first global approval. Drugs. 2019;79(11):1249–53.
Venot Q, Blanc T, Rabia SH, Berteloot L, Ladraa S, Duong JP, et al. Targeted therapy in patients with PIK3CA-related overgrowth syndrome. Nature. 2018;558(7711):540–6.
Lindhurst MJ, Yourick MR, Yu Y, Savage RE, Ferrari D, Biesecker LG. Repression of AKT signaling by ARQ 092 in cells and tissues from patients with Proteus syndrome. Sci Rep. 2015;5:17162.
Ranieri C, Di Tommaso S, Loconte DC, Grossi V, Sanese P, Bagnulo R, et al. In vitro efficacy of ARQ 092, an allosteric AKT inhibitor, on primary fibroblast cells derived from patients with PIK3CA-related overgrowth spectrum (PROS). Neurogenetics. 2018;19(2):77–91.
Biesecker LG, Edwards M, O’Donnell S, Doherty P, MacDougall T, Tith K, et al. Clinical report: one year of treatment of Proteus syndrome with miransertib (ARQ 092). Cold Spring Harb Mol Case Stud. 2020;6(1) (pii: a004549).
Adams DM, Ricci KW. Vascular anomalies: diagnosis of complicated anomalies and new medical treatment options. Hematol Oncol Clin N Am. 2019;33(3):455–70.
Ozeki M, Fukao T. Generalized lymphatic anomaly and Gorham-Stout disease: overview and recent insights. Adv Wound Care (New Rochelle). 2019;8(6):230–45.
Li D, March M, Gutierrez-Uzquiza A, Kao C, Seiler C, Pinto E, et al. ARAF recurrent mutation causes central conducting lymphatic anomaly treatable with a MEK inhibitor. Nat Med. 2019;25(7):1116–22.
Lekwuttikarn R, Lim YH, Admani S, Choate KA, Teng JMC. Genotype-guided medical treatment of an arteriovenous malformation in a child. JAMA Dermatol. 2019;155(2):256–7.
Dupuis-Girod S, Ginon I, Saurin JC, Marion D, Guillot E, Decullier E, et al. Bevacizumab in patients with hereditary hemorrhagic telangiectasia and severe hepatic vascular malformations and high cardiac output. JAMA. 2012;307(9):948–55.
Halderman AA, Ryan MW, Marple BF, Sindwani R, Reh DD, Poetker DM. Bevacizumab for epistaxis in hereditary hemorrhgaic telangiectasia: an evidence-based review. Am J Rhinol Allergy. 2018;32(4):258–68.
Kini SD, Yiu DW, Weisberg RA, Davila JF, Chelius DC. Bevacizumab as treatment for epistaxis in hereditary hemorrhagic telangiectasia: a literature review. Ann Otol Rhinol Laryngol. 2019;128(5):467–71.
Stokes P, Rimmer J. Intranasal bevacizumab in the treatment of HHT-related epistaxis: a systematic review. Rhinology. 2018;56(1):3–10.
Parambil JG, Woodard TD, Koc ON. Pazopanib effective for bevacizumab-unresponsive epistaxis in hereditary hemorrhagic teleangiectasia. Laryngoscope. 2018;128(10):2234–6.
Robert F, Desroches-Castan A, Bailly S, Dupuis-Girod S, Feige JJ. Future treatments for hereditary hemorrhagic telangiectasia. Orphanet J Rare Dis. 2020;15(1):4.
Uno T, Ito S, Nakazawa A, Miyazaki O, Mori T, Terashima K. Successful treatment of kaposiform hemangioendothelioma with everolimus. Pediatr Blood Cancer. 2015;62:536–8.
Author information
Authors and Affiliations
Contributions
AVD performed the literature search and data analysis, and drafted the manuscript. ES, VD, LMB, and MV critically revised the work. The authors of this publication are members of the Vascular Anomalies Working Group (VASCA WG) of the European Reference Network for Rare Multisystemic Vascular Diseases (VASCERN), Project ID: 769036.
Corresponding author
Ethics declarations
Funding
No sources of funding were used to assist in the preparation of this review.
Conflict of interest
An Van Damme and Valérie Dekeuleneer have no conflicts of interest that are directly relevant to the content of this article. Emmanuel Seront discloses the following interactions with the medical industry: (1) clinical trial support for VASE: Pfizer [slow-flow vascular anomalies (rapamycin)] and (2) clinical trial support for TRAMAV: Novartis [fast-flow vascular anomalies (trametinib)]. Laurence M. Boon discloses the following interactions with the medical industry: (1) clinical trial support for VASE: Pfizer [slow-flow vascular anomalies (rapamycin)]; (2) clinical trial support for TRAMAV: Novartis [fast-flow vascular anomalies (trametinib)]; (3) clinical advisory board: Venthera [slow-flow malformations (transdermal PI3K inhibitor)]; and (4) clinical advisory board: Pierre Fabre [infantile hemangiomas (beta-blockers)]. Miikka Vikkula discloses the following interactions with the medical industry: (1) research grant from Deciphera Pharmaceuticals [venous malformations (rebastinib)] and (2) scientific and clinical advisory boards: Venthera [slow-flow malformations (transdermal PI3K inhibitor)].
Rights and permissions
About this article
Cite this article
Van Damme, A., Seront, E., Dekeuleneer, V. et al. New and Emerging Targeted Therapies for Vascular Malformations. Am J Clin Dermatol 21, 657–668 (2020). https://doi.org/10.1007/s40257-020-00528-w
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40257-020-00528-w