Abstract
Purpose
Diabetic foot infection (DFI) is one of the most feared complications of diabetes. In Sudan, the number of cases and the problems associated with diabetic foot infections increased in recent years. This study aimed to assess the bacteriological profile of patients with DFIs and their antibiotic susceptibility pattern.
Methods
A descriptive retrospective cross-sectional study was carried out at Surgery Department of Ribat University Hospital. All medical records of patients with DFIs during the period from September 2017 to February 2019 were reviewed using data collection sheet. The collected data were analyzed using Statistical Package for Social Sciences.
Results
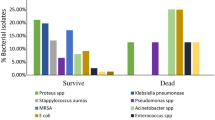
Out of 250 DFI patients, 73.2% of them were males, and 86.4% of them had type 2 diabetes mellitus, and most of them suffered from diabetes for more than 10 years. Regarding culture results, 64.7% and 35.3% of the samples revealed presence of single microorganism and mixed infections, respectively. A total of 335 bacterial isolates were identified, gram-negative were more prevalent than gram-positive organisms. The most frequently isolated organisms were Proteus spp. Staphylococcus aureus, and Escherichia coli. Furthermore, antibiotic susceptibility pattern showed that imipenem, amikacin and vancomycin have the highest activity against isolated bacteria, and all isolates were found to be completely resistant to different cephalosporin drugs.
Conclusion
Among the studied samples, gram-negative bacteria were found to be more common in DFI patients, Proteus spp. and S. aureus were the most common microorganisms. Moreover, different isolated microorganisms showed to have different degrees of resistance and sensitivity to various antibacterial drugs.
Similar content being viewed by others
Availability of data
available.
References
Khanolkar MP, Bain SC, Stephens JW. The diabetic foot. QJM. 2008;101:685–95.
Diabetic Foot. In: Liapis CD, Balzer K, Benedetti-Valentini F, Fernandes E, Fernandes J, editors. Vascular Surgery. Berlin, Heidelberg: Springer Berlin Heidelberg; 2007. p. 501–21.
Alavi SM, Khosravi A, Sarami A, Dashtebozorg A, Montazeri EA. Bacteriologic study of diabetic foot ulcer. Int. J. Infect. Dis. 2008;12:e209.
Sharma VK, Khadka PB, Joshi A, Sharma R. Common pathogens isolated in diabetic foot infection in Bir hospital. Kathmandu Univ. Med. J. 2006;4:295–301.
Oyibo SO, Jude EB, Tarawneh I, Nguyen HC, Harkless LB, Boulton AJ. A comparison of two diabetic foot ulcer classification systems: the Wagner and the University of Texas wound classification systems. Diabetes Care. 2001;24:84–8.
Pickwell K, Siersma V, Kars M, Apelqvist J, Bakker K, Edmonds M, et al. Predictors of lower-extremity amputation in patients with an infected diabetic foot ulcer. Diabetes Care. 2015;38:852–7.
Hobizal KB, Wukich DK. Diabetic foot infections: current concept review. Diabet. Foot. Ankle. 2012;3:184–9.
Shankar EM, Mohan V, Premalatha G, Srinivasan RS, Usha AR. Bacterial etiology of diabetic foot infections in South India. Eur. J. Intern. Med. 2005;16:567–70.
Akhi MT, Ghotaslou R, Asgharzadeh M, Varshochi M, Pirzadeh T, Memar MY, et al. Bacterial etiology and antibiotic susceptibility pattern of diabetic foot infections in Tabriz. Iran. GMS Hyg. Infect. Control. 2015;10:1–6.
Citron DM, Goldstein EJC, Merriam CV, Lipsky BA, Abramson MA. Bacteriology of moderate-to-severe diabetic foot infections and in vitro activity of antimicrobial agents. J. Clin. Microbiol. 2007;45:2819–28.
Jain SK, Barman R. Bacteriological profile of diabetic Foot ulcer with special reference to drug-resistant strains in a tertiary Care Center in North-East India. Indian. J. Endocrinol. Metab. 2017;21:688–94.
Lipsky BA. Medical treatment of diabetic foot infections. Clin. Infect. Dis. 2004;39:S104–14.
Blanes JI. Consensus document on treatment of infections in diabetic foot. Rev. Esp. Quimioter. 2011;24:233–62.
Boulton AJM, Armstrong DG, Hardman MJ, Malone M, Embil JM, Attinger CE, et al. Diagnosis and Management of Diabetic Foot Infections. Arlington (VA): Am. Diabetes Assoc.2020.
Lipsky BA, Berendt AR, Embil J, De Lalla F. Diagnosing and treating diabetic foot infections. Diabetes Metab. Res. Rev. 2004;20:S56–64.
Lipsky BA. New developments in diagnosing and treating diabetic foot infections. Diabetes Metab. Res. Rev. 2008;24:828.
Lipsky BA, Berendt AR, Cornia PB, Pile JC, Peters EJ, Armstrong DG, et al. 2012 Infectious Diseases Society of America clinical practice guideline for the diagnosis and treatment of diabetic foot infections. Clin. Infect. Dis. 2012;54:e132–73.
Joseph WS, Lipsky BA. Medical therapy of diabetic foot infections. J. Vasc. Surg. 2010;52:S67–71.
Lipsky BA, Holroyd KJ, Zasloff M. Topical versus systemic antimicrobial therapy for treating mildly infected diabetic foot ulcers: a randomized, controlled, double-blinded, multicenter trial of pexiganan cream. Clin. Infect. Dis. 2008;47:1537–45.
Almobarak AO, Awadalla H, Osman M, Ahmed MH. Prevalence of diabetic foot ulceration and associated risk factors: an old and still major public health problem in Khartoum, Sudan? Ann. Transl. Med. 2017;5:340.
Bakheit HE, Mohamed MF, Mahadi SEI, Widatalla ABH, Shawer MA, Khamis AH, et al. Diabetic heel ulcer in the Sudan: determinants of outcome. J. Foot Ankle Surg. 2012;51:152–5.
Richard JL, Sotto A, Jourdan N, Combescure C, Vannereau D, Rodier M, et al. Risk factors and healing impact of multidrug-resistant bacteria in diabetic foot ulcers. Diabetes Metab. 2008;34:363–9.
Hartemann-Heurtier A, Robert J, Jacqueminet S, Ha Van G, Golmard J, Jarlier V, et al. Diabetic foot ulcer and multidrug-resistant organisms: risk factors and impact. Diabet. Med. 2004;21:710–5.
Ganguly NK, Arora NK, Chandy SJ, Fairoze MN, Gill JP, Gupta U, et al. Rationalizing antibiotic use to limit antibiotic resistance in India. Indian J. Med. Res. 2011;134:281–94.
Umasankari J, Jeya M, Sekar C. Microbiological study of diabetic foot ulcers and analysis of ESBL activity of the bacterial isolates. J. Pharm. Res. 2012;5:2329–32.
Bentkover J. Economic evaluation of alternative methods of treatment for diabetic foot ulcer patients: cost-effectiveness of platelet releasate and wound care clinics. Wounds. 1993;5:207–15.
Jouhar L, Minhem M, Akl E, Rizk N, Hoballah J. Microbiological profile of diabetic foot infection in the Middle East and North Africa: a systematic review. Wounds. 2019;6:43–50.
Casqueiro J, Casqueiro J, Alves C. Infections in patients with diabetes mellitus: a review of pathogenesis. Indian. J. Endocrinol. Metab. 2012;16:S27–36.
Badawi MM, Adam AA, Sidig ES, SalahEldin MA, Abdalla SA, Yousof YS, et al. Genotypic and phenotypic drug resistance of Bacteria associated with diabetic septic Foot infections among Sudanese. Saudi. J. Pathol. Microbiol. 2017;2:228–36.
Abdulrazak A, Bitar ZI, Al-Shamali AA, Mobasher LA. Bacteriological study of diabetic foot infections. J. Diabetes Complicat. 2005;19:138–41.
Hefni AA, Ibrahim AM, Attia KM, Moawad MM, El-ramah AF, Shahin MM, et al. Bacteriological study of diabetic foot infection in Egypt. J. Arab. Society Med. Res. 2013;8:26–32.
Ben MM, Khalfallah M, Boutiba IBB, Nouira R, Slim A, Jerraya H, et al. Bacteriological and therapeutic profile of diabetic foot infection: a prospective study of 100 patients. La Tunisie medicale. 2016;94:95–101.
Al Ayed MY, Ababneh M, Alwin Robert A, Alzaid A, Ahmed RA, Salman A, et al. Common pathogens and antibiotic sensitivity profiles of infected diabetic foot ulcers in Saudi Arabia. Int J Low Extrem Wounds. 2018;17:161–8.
Kamel NA, Abouelwafa MM, El-tayeb WN, Aboshanab KM. Antibacterial resistance pattern of aerobic bacteria isolated from patients with diabetic foot ulcers in Egypt. Afr. J. Microbiol. Res. 2014;8:2947–54.
Al-Joufi FA, Aljarallah KM, Hagras SA, Al Hosiny IM, Salem-Bekhit MM, Youssof AM, et al. Microbial spectrum, antibiotic susceptibility profile, and biofilm formation of diabetic foot infections (2014–18): a retrospective multicenter analysis. 3. Biotech. 2020;10:1–12.
Anvarinejad M, Pouladfar G, Japoni A, Bolandparvaz S, Satiary Z, Abbasi P, et al. Isolation and antibiotic susceptibility of the microorganisms isolated from diabetic foot infections in Nemazee hospital. Southern Iran J. Pathog. 2015;2015:328796.
Dhanasekaran G, Sastry G, Viswanathan M. Microbial pattern of soft tissue infections in diabetic patients in South India. Asian. J. Diabet. 2003;5:8–10.
Tiwari S, Pratyush DD, Dwivedi A, Gupta SK, Rai M, Singh SK. Microbiological and clinical characteristics of diabetic foot infections in northern India. J. Infect. Dev. Ctries. 2012;6:329–32.
Gadepalli R, Dhawan B, Sreenivas V, Kapil A, Ammini AC, Chaudhry R. A clinico-microbiological study of diabetic foot ulcers in an Indian tertiary care hospital. Diabetes Care. 2006;29:1727–32.
Sotto A, Richard JL, Combescure C, Jourdan N, Schuldiner S, Bouziges N, et al. Beneficial effects of implementing guidelines on microbiology and costs of infected diabetic foot ulcers. Diabetologia. 2010;53:2249–55.
Bansal E, Garg A, Bhatia S, Attri AK, Chander J. Spectrum of microbial flora in diabetic foot ulcers. Indian J. Pathol. Microbiol. 2008;51:204–8.
Sivanmaliappan TS, Sevanan M. Antimicrobial susceptibility patterns of Pseudomonas aeruginosa from diabetes patients with Foot ulcers. Int. J. Microbiol. 2011;2011:605195.
Gu J, Li H, Li M, Vuong C, Otto M, Wen Y, et al. Bacterial insertion sequence IS256 as a potential molecular marker to discriminate invasive strains from commensal strains of Staphylococcus epidermidis. J. Hosp. Infect. 2005;61:342–8.
Dumville JC, O'Meara S, Deshpande S, Speak K. Alginate dressings for healing diabetic foot ulcers. Cochrane Database Syst. Rev. 2012;15:CD009110.
Rawat V, Singhai M, Kumar A, Jha PK, Goyal R. Bacteriological and resistance profile in isolates from diabetic patients. N. Am. J. Med. Sci. 2012;4:563–8.
Bengalorkar GM, Kumar T. Culture and sensitivity pattern of micro-organism isolated from diabetic foot infections in a tertiary care hospital. Int. J. Cur. Biomed. Phar. Res. 2011;1:34–40.
Lee JH, Bae IK, Lee SH. New definitions of extended-spectrum β-lactamase conferring worldwide emerging antibiotic resistance. Med. Res. Rev. 2012;32:216–32.
Shahid M, Singhai M, Malik A, Shukla I, Khan H, Shujatullah F, et al. In vitro efficacy of ceftriaxone/sulbactam against Escherichia coli isolates producing CTX-M-15 extended-spectrum β-lactamase. J. Antimicrob. Chemother. 2007;60:187–8.
Byarugaba D. Antimicrobial resistance in developing countries and responsible risk factors. Int. J. Antimicrob. Agents. 2004;24:105–10.
Barbosa TM, Levy SB. The impact of antibiotic use on resistance development and persistence. Drug Resist. Updat. 2000;3:303–11.
Abdalla SN, Yousef BA. Prescribing patterns of antimicrobials in the internal medicine Department of Ibrahim Malik Teaching Hospital in Khartoum, 2016. Pan Afr. Med. J. 2019;34:89.
Salim AMA, Elgizoli B. Exploring the reasons why pharmacists dispense antibiotics without prescriptions in Khartoum state. Sudan Int. J. Pharm. Pract. 2017;25:59–65.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Code availability
available.
Consent to participate
Not applicable.
Consent to publish
The Author transfers to Springer/ Journal of Diabetes & Metabolic Disorders the non-exclusive publication rights. This transfer of publication rights covers the non-exclusive right to reproduce and distribute the article, including reprints, translations, photographic reproductions, microform, electronic form or any other reproductions of similar nature.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hamid, M.H., Arbab, A.H. & Yousef, B.A. Bacteriological profile and antibiotic susceptibility of diabetic Foot infections at Ribat University hospital; a retrospective study from Sudan. J Diabetes Metab Disord 19, 1397–1406 (2020). https://doi.org/10.1007/s40200-020-00660-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40200-020-00660-8