Abstract
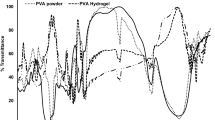
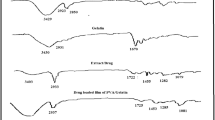
The present study aimed at developing an injectable hydrogel based on acacia gum (AG) for wound healing acceleration. The hydrogels were synthetized through metal-ligand coordination mediated by Fe3+ and characterized in terms of gelation time, gel content, initial water content, swelling capacity, water retention ratio, and porosity. Moreover, FTIR, XRD and TGA analyses were performed for the hydrogels and allantoin (Alla) loaded ones. Furthermore, bioadhessiveness, and self-healing as well as antibacterial, toxicity and wound healing potentials of the hydrogels were evaluated. The hydrogels displayed fast gelation time, high swelling, porosity, and bioadhessiveness, as well as antioxidant, self-healing, antibacterial, blood clotting, and injectability properties. FTIR, XRD and TGA analyses confirmed hydrogel synthesis and drug loading. The Alla-loaded hydrogels accelerated wound healing by decreasing the inflammation and increasing the cell proliferation as well as collagen deposition. Hemocompatibility, cell cytotoxicity, and in vivo toxicity experiments were indicative of a high biocompatibility level for the hydrogels. Given the advantages of fast gelation, injectability and beneficial biological properties, the use of Alla-loaded hydrogels could be considered a new remedy for efficient wound healing.
Graphical abstract









Similar content being viewed by others
References
Xu J, Liu Y, Hsu SH. Hydrogels based on schiff base linkages for biomedical applications. Molecules. 2019;24(16): 3005. https://doi.org/10.3390/molecules24163005.
Parwani L, Bhatnagar M, Bhatnagar A, Sharma V, Sharma V. Gum acacia-PVA hydrogel blends for wound healing. Vegetos. 2019;32(1):78–91. https://doi.org/10.1007/s42535-019-00009-4.
Ahmadian Z, Gheybi H, Adeli M. Efficient wound healing by antibacterial property: advances and trends of hydrogels, hydrogel-metal NP composites and photothermal therapy platforms. J Drug Deliv Sci Technol. 2022;103458. .https://doi.org/10.1016/j.jddst.2022.103458
Zohreband Z, Adeli M, Zebardasti A. Self-healable and flexible supramolecular gelatin/MoS2 hydrogels with molecular recognition properties. Int J Biol Macromol. 2021;182:2048–55. https://doi.org/10.1016/j.ijbiomac.2021.05.106.
Sattari S, Dadkhah Tehrani A, Adeli M. pH-responsive hybrid hydrogels as antibacterial and drug delivery systems. Polymers. 2018;10(6): 660. https://doi.org/10.3390/polym10060660.
Mescher AL. Macrophages and fibroblasts during inflammation and tissue repair in models of organ regeneration. Regeneration. 2017;4(2):39–53. https://doi.org/10.1002/reg2.77.
Atala A, Irvine DJ, Moses M, Shaunak S. Wound healing versus regeneration: role of the tissue environment in regenerative medicine. MRS Bull. 2010;35(8):597–606. https://doi.org/10.1557/mrs2010.528.
Giano MC, Ibrahim Z, Medina SH, Sarhane KA, Christensen JM, Yamada Y, Brandacher G, Schneider JP. Injectable bioadhesive hydrogels with innate antibacterial properties. Nat Commun. 2014;5(1):4095. https://doi.org/10.1038/ncomms5095.
Yan S, Wang W, Li X, Ren J, Yun W, Zhang K, Li G, Yin J. Preparation of mussel-inspired injectable hydrogels based on dual-functionalized alginate with improved adhesive, self-healing, and mechanical properties. J Mater Chem B. 2018;6(40):6377–90. https://doi.org/10.1039/C8TB01928B.
Sundaram MN, Pradeep A, Varma PK, Jayakumar R. Different forms of chitosan and its derivatives as hemostatic agent and tissue sealants. 2021. pp. 1–28; https://doi.org/10.1007/12_2021_98.
Pei X, Wang J, Cong Y, Fu J. Recent progress in polymer hydrogel bioadhesives. J Polym Sci. 2021;59(13):1312–37. https://doi.org/10.1002/pol.20210249.
Nam S, Mooney D. Polymeric tissue adhesives. Chem Rev. 2021;121(18):11336–84. https://doi.org/10.1021/acs.chemrev.0c00798.
Guo J, Sun W, Kim JP, Lu X, Li Q, Lin M, Mrowczynski O, Rizk EB, Cheng J, Qian G, Yang J. Development of tannin-inspired antimicrobial bioadhesives. Acta Biomater. 2018;72:35–44. https://doi.org/10.1016/j.actbio.2018.03.008.
Wu C, Shen L, Lu Y, Hu C, Liang Z, Long L, Ning N, Chen J, Guo Y, Yang Z, Hu X. Intrinsic antibacterial and conductive hydrogels based on the distinct bactericidal effect of polyaniline for infected chronic wound healing. ACS Appl Mater Interfaces. 2021;13(44):52308–20. https://doi.org/10.1021/acsami.1c14088.
Tu Y, Chen N, Li C, Liu H, Zhu R, Chen S, Xiao Q, Liu J, Ramakrishna S, He L. Advances in injectable self-healing biomedical hydrogels. Acta Biomater. 2019;90:1–20. https://doi.org/10.1016/j.actbio.2019.03.057.
Zhao X, Wu H, Guo B, Dong R, Qiu Y, Ma PX. Antibacterial anti-oxidant electroactive injectable hydrogel as self-healing wound dressing with hemostasis and adhesiveness for cutaneous wound healing. Biomaterials. 2017;122:34–47. https://doi.org/10.1016/j.biomaterials.2017.01.011.
Geng H, Dai Q, Sun H, Zhuang L, Song A, Caruso F, Hao J, Cui J. Injectable and sprayable polyphenol-based hydrogels for controlling hemostasis. ACS Appl Bio Mater. 2020;3(2):1258–66. https://doi.org/10.1021/acsabm.9b01138.
Pourshahrestani S, Zeimaran E, Kadri NA, Mutlu N, Boccaccini AR. Polymeric hydrogel systems as emerging biomaterial platforms to enable hemostasis and wound healing. Adv Healthc Mater. 2020;9(20): 2000905. https://doi.org/10.1002/adhm.202000905.
Aduba DC Jr, Yang H. Polysaccharide fabrication platforms and biocompatibility assessment as candidate wound dressing materials. Bioengineering. 2017;4(1):1. https://doi.org/10.3390/bioengineering4010001.
Patel S, Goyal A. Applications of natural polymer gum arabic: a review. Int J Food Prop. 2015;18(5):986. https://doi.org/10.1080/10942912.2013.809541.
Ibekwe CA, Oyatogun GM, Esan TA, Oluwasegun KM. Synthesis and characterization of chitosan/gum arabic nanoparticles for bone regeneration. Am J Mater Sci Eng. 2017;5(1). .https://doi.org/10.12691/ajmse-5-1-4
Sanchez C, Nigen M, Tamayo VM, Doco T, Williams P, Amine C, Renard D. Acacia gum: history of the future. Food Hydrocolloids. 2018;78:140–60. https://doi.org/10.1016/j.foodhyd.2017.04.008.
Singh B, Sharma S, Dhiman A. Acacia gum polysaccharide based hydrogel wound dressings: synthesis, characterization, drug delivery and biomedical properties. Carbohydr Polym. 2017;165:294–303. https://doi.org/10.1016/j.carbpol.2017.02.039.
Elblbesy MA, Hanafy TA, Shawki MM. Polyvinyl alcohol/gum arabic hydrogel preparation and cytotoxicity for wound healing improvement. E-Polymers. 2022;22(1):566. https://doi.org/10.1515/epoly-2022-0052.
Raguvaran R, Manuja BK, Chopra M, Thakur R, Anand T, Kalia A, Manuja A. Sodium alginate and gum acacia hydrogels of ZnO nanoparticles show wound healing effect on fibroblast cells. Int J Biol Macromol. 2017;96:185–91. https://doi.org/10.1016/j.ijbiomac.2016.12.009.
Li M, Li H, Li X, Zhu H, Xu Z, Liu L, Ma J, Zhang M. A bioinspired alginate-gum arabic hydrogel with micro-/nanoscale structures for controlled drug release in chronic wound healing. ACS Appl Mater Interfaces. 2017;9(27):22160–75. https://doi.org/10.1021/acsami.7b04428.
Ye J, Yang G, Zhang J, Xiao Z, He L, Zhang H, Liu Q. Preparation and characterization of gelatin-polysaccharide composite hydrogels for tissue engineering. PeerJ. 2021;9: e11022. https://doi.org/10.7717/peerj.11022.
Bealer EJ, Onissema-Karimu S, Rivera-Galletti A, Francis M, Wilkowski J, Salas-de la Cruz D, Hu X. Protein–polysaccharide composite materials: fabrication and applications. Polymers. 2020;12(2): 464. https://doi.org/10.3390/polym12020464.
Amaya-Chantaca NJ, Caldera-Villalobos M, Claudio-Rizo JA, Flores-Guía TE, Becerra-Rodríguez JJ, Soriano-Corral F, Herrera-Guerrero A. Semi-IPN hydrogels of collagen and gum arabic with antibacterial capacity and controlled release of drugs for potential application in wound healing. Prog Biomater. 2023;12(1):25–40. https://doi.org/10.1007/s40204-022-00210-w.
Ahmadian Z, Correia A, Hasany M, Figueiredo P, Dobakhti F, Eskandari MR, Hosseini SH, Abiri R, Khorshid S, Hirvonen J, Santos HA. A hydrogen-bonded extracellular matrix‐mimicking bactericidal hydrogel with radical scavenging and hemostatic function for pH‐responsive wound healing acceleration. Adv Health Mater. 2021;10(3):2001122. https://doi.org/10.1002/adhm.202001122.
Becker LC, Bergfeld WF, Belsito DV, Klaassen CD, Marks JG, Shank RC, Slaga TJ, Snyder PW, Andersen FA. Final report of the safety assessment of allantoin and its related complexes. Int J Toxicol. 2010;29(3suppl):84S – 97. https://doi.org/10.1177/1091581810362805.
Li QX, Song BZ, Yang ZQ, Fan HL. Electrolytic conductivity behaviors and solution conformations of chitosan in different acid solutions. Carbohydr Polym. 2006;63(2):272. https://doi.org/10.1016/j.carbpol.2005.09.024.
Gupta KC, Jabrail FH. Glutaraldehyde and glyoxal cross-linked chitosan microspheres for controlled delivery of centchroman. Carbohydr Res. 2006;341(6):744. https://doi.org/10.1016/j.carres.2006.02.003.
Gupta KC, Jabrail FH. Glutaraldehyde cross-linked chitosan microspheres for controlled release of centchroman. Carbohydr Res. 2007;342(15):2244–52. https://doi.org/10.1016/j.carres.2007.06.009.
Dherange DD, Pangavane MR. Review on: excipients used in herbal drug technology. Int J Res Publ Rev. 2022;3(2):465–475.
Musa HH, Ahmed AA, Musa TH. Chemistry, biological, and pharmacological properties of gum Arabic. Bioactive Molecules in Food; Springer International Publishing AG: Cham, Switzerland. 2018:1–8; https://doi.org/10.1007/978-3-319-54528-8_11-1.
Qu J, Zhao X, Liang Y, Zhang T, Ma PX, Guo B. Antibacterial adhesive injectable hydrogels with rapid self-healing, extensibility and compressibility as wound dressing for joints skin wound healing. Biomaterials. 2018;183:185–99. https://doi.org/10.1016/j.biomaterials.2018.08.044.
Zhu J, Han H, Li F, Wang X, Yu J, Qin X, Wu D. Peptide-functionalized amino acid-derived pseudoprotein-based hydrogel with hemorrhage control and antibacterial activity for wound healing. Chem Mater. 2019;31(12):4436–50. https://doi.org/10.1021/acs.chemmater.9b00850.
Murphy CM, O’Brien FJ, Little DG, Schindeler A. Cell-scaffold interactions in the bone tissue engineering triad. Eur Cell Mater. 2013;26(4):120. https://doi.org/10.22203/eCM.v026a09.
Balaji A, Jaganathan SK, Ismail AF, Rajasekar R. Fabrication and hemocompatibility assessment of novel polyurethane-based bio-nanofibrous dressing loaded with honey and Carica papaya extract for the management of burn injuries. Int J Nanomed. 2016;11:4339. https://doi.org/10.2147/IJN.S112265.
Wang Y, Tong L, Zheng Y, Pang S, Sha J, Li L, Zhao G. Hydrogels with self-healing ability, excellent mechanical properties and biocompatibility prepared from oxidized gum arabic. Eur Polymer J. 2019;117:363–71. https://doi.org/10.1016/j.eurpolymj.2019.05.033.
Duan W, Bian X, Bu Y. Applications of bioadhesives: a mini review. Front Bioeng Biotechnol. 2021;9:716035. https://doi.org/10.3389/fbioe.2021.716035.
Rad ZP, Mokhtari J, Abbasi M. Fabrication and characterization of PCL/zein/gum arabic electrospun nanocomposite scaffold for skin tissue engineering. Mater Sci Eng: C. 2018;93:356–66. https://doi.org/10.1016/j.msec.2018.08.010.
Ates B, Koytepe S, Balcioglu S, Karaaslan MG, Kelestemur U, Gulgen S, Ozhan O. Biomimetic approach to tunable adhesion of polyurethane adhesives through Fe3 + crosslinking and hydrophobic tween units with balance of adhesion/cohesion forces. Int J Adhes Adhes. 2019;95: 102396. https://doi.org/10.1016/j.ijadhadh.2019.102396.
Ali S, Khatri Z, Oh KW, Kim IS, Kim SH. Zein/cellulose acetate hybrid nanofibers: electrospinning and characterization. Macromol Res. 2014;22:971–7. https://doi.org/10.1007/s13233-014-2136-4.
Cai Y, Wang Q, Wei Q, You Q, Huang F, Song L, Hu Y, Gao W. Structure, thermal, and antibacterial properties of polyacrylonitrile/ferric chloride nanocomposite fibers by electrospinning. Int J Polym Anal Charact. 2010;15(2):110–8. https://doi.org/10.1080/10236660903525083.
Baien SH, Seele J, Henneck T, Freibrodt C, Szura G, Moubasher H, Nau R, Brogden G, Mörgelin M, Singh M, Kietzmann M. Antimicrobial and immunomodulatory effect of gum arabic on human and bovine granulocytes against Staphylococcus aureus and Escherichia coli. Front Immunol. 2020;10: 3119. https://doi.org/10.3389/fimmu.2019.03119.
Tian R, Qiu X, Yuan P, Lei K, Wang L, Bai Y, Liu S, Chen X. Fabrication of self-healing hydrogels with on-demand antimicrobial activity and sustained biomolecule release for infected skin regeneration. ACS Appl Mater Interfaces. 2018;10(20):17018–27. https://doi.org/10.1021/acsami.8b01740.
Lv C, Li L, Jiao Z, Yan H, Wang Z, Wu Z, Guo M, Wang Y, Zhang P. Improved hemostatic effects by Fe3 + modified biomimetic PLLA cotton-like mat via sodium alginate grafted with dopamine. Bioactive Mater. 2021;6(8):2346–59. https://doi.org/10.1016/j.bioactmat.2021.01.002.
Sakthiguru N, Sithique MA. Fabrication of bioinspired chitosan/gelatin/allantoin biocomposite film for wound dressing application. Int J Biol Macromol. 2020;152:873–83. https://doi.org/10.1016/j.ijbiomac.2020.02.289.
O’Connor NA, Syed A, Wong M, Hicks J, Nunez G, Jitianu A, Siler Z, Peterson M. Polydopamine antioxidant hydrogels for wound healing applications. Gels. 2020;6(4): 39. https://doi.org/10.3390/gels6040039.
Standard AS. F756-00: Standard standard practice for assessment of hemolytic properties of materials. USA: Annual Book of ASTM Standards; 2000.
Ugartondo V, Mitjans M, Vinardell MP. Comparative antioxidant and cytotoxic effects of lignins from different sources. Bioresour Technol. 2008;99(14):6683–7. https://doi.org/10.1016/j.biortech.2007.11.038.
Picone P, Sabatino MA, Ajovalasit A, Giacomazza D, Dispenza C, Di Carlo M. Biocompatibility, hemocompatibility and antimicrobial properties of xyloglucan-based hydrogel film for wound healing application. Int J Biol Macromol. 2019;121:784–95. https://doi.org/10.1016/j.ijbiomac.2018.10.078.
Tsou YH, Khoneisser J, Huang PC, Xu X. Hydrogel as a bioactive material to regulate stem cell fate. Bioactive Mater. 2016;1(1):39–55. https://doi.org/10.1016/j.bioactmat.2016.05.001.
Tibbitt MW, Anseth KS. Hydrogels as extracellular matrix mimics for 3D cell culture. Biotechnol Bioeng. 2009;103(4):655. https://doi.org/10.1002/bit.22361.
Ahmadian Z, Dargahi AR, Musaie K, Eskandari MR. Preparation and in vivo toxicity study of allantoin incorporated hyaluronic acid-L-cysteine oral solution: a future treatment for mucositis. Pharm Sci. 2021;28(3):414–23. https://doi.org/10.34172/PS.2021.65.
Florentino IF, Silva DP, Galdino PM, Lino RC, Martins JL, Silva DM, de Paula JR, Tresvenzol LM, Costa EA. Antinociceptive and anti-inflammatory effects of Memora nodosa and allantoin in mice. J Ethnopharmacol. 2016;186:298–304. https://doi.org/10.1016/j.jep.2016.04.010.
Ali BH, Al-Husseni I, Beegam S, Al-Shukaili A, Nemmar A, Schierling S, Queisser N, Schupp N. Effect of gum arabic on oxidative stress and inflammation in adenine–induced chronic renal failure in rats. PLoS ONE. 2013;8(2): e55242. https://doi.org/10.1371/journal.pone.0055242.
Sowa I, Paduch R, Strzemski M, Zielińska S, Rydzik-Strzemska E, Sawicki J, Kocjan R, Polkowski J, Matkowski A, Latalski M, Wójciak-Kosior M. Proliferative and antioxidant activity of Symphytum officinale root extract. Nat Prod Res. 2018;32(5):605–9. https://doi.org/10.1080/14786419.2017.1326492.
Araújo LU, Grabe-Guimarães A, Mosqueira VC, Carneiro CM, Silva-Barcellos NM. Profile of wound healing process induced by allantoin. Acta Cirurgica Brasileira. 2010;25:460–1. https://doi.org/10.1590/S0102-86502010000500014.
Nokoorani YD, Shamloo A, Bahadoran M, Moravvej H. Fabrication and characterization of scaffolds containing different amounts of allantoin for skin tissue engineering. Sci Rep. 2021;11(1):16164. https://doi.org/10.1038/s41598-021-95763-4.
Valle KZ, Saucedo Acuña RA, Ríos Arana JV, Lobo N, Rodriguez C, Cuevas-Gonzalez JC, Tovar-Carrillo KL. Natural film based on pectin and allantoin for wound healing: obtaining, characterization, and rat model. BioMed Res Int. 2020;2020. https://doi.org/10.1155/2020/6897497
Acknowledgements
The authors would like to thank Dr. Ahmad Salimi, Ardabil University of Medical Sciences, for helpful suggestions with regard to the technical issues examined in the present study. The authors also would like to thank Ardabil University of Medical Sciences for its financial support (ethical code: IR.ARUM.REC.1400.016). The authors are also grateful to the staff of Iran Science Elites Federation.
Funding
The financial resources of this work were provided by Ardabil University of Medical Sciences, Ardabil, Iran.
Author information
Authors and Affiliations
Contributions
Conceptualization: Zainab Ahmadian, Mohsen Adeli; Methodology: Zainab Ahmadian, Mahsa Zibanejad Jelodar, Sajjad Sefareshi, Vahed Adhami; Formal analysis and investigation: Zainab Ahmadian, Hossein Ali Ebrahimi, Motaleb Ghasemian; Writing-original and editing: Zainab Ahmadian, Marzieh Rashidipour.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ahmadian, Z., Jelodar, M.Z., Rashidipour, M. et al. A self-healable and bioadhesive acacia gum polysaccharide-based injectable hydrogel for wound healing acceleration. DARU J Pharm Sci 31, 205–219 (2023). https://doi.org/10.1007/s40199-023-00475-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40199-023-00475-x