Abstract
Purpose of Review
Vestibular schwannomas are WHO grade I tumors of the eighth cranial nerve that lead to hearing loss, tinnitus, vestibular dysfunction, and facial nerve compromise. The management of vestibular schwannomas consists of observation, radiosurgery, or microsurgical resection. In this review, we discuss the various treatment modalities specifically targeting large vestibular schwannomas in addition to their treatment risk profiles.
Recent Findings
Although there has been a trend towards treatment with radiosurgery for smaller lesions, consensus reports still advocate for surgical debulking in patients with large vestibular schwannomas. There has been a shift in management philosophy towards functional preservation at the cost of more extensive resection, yet subtotal resection of vestibular schwannomas is associated with higher rates of recurrence on follow-up. Some groups have demonstrated new promise for the management of large vestibular schwannomas with stereotactic radiosurgery alone and multimodality therapy involving subtotal surgical resection with planned postoperative radiosurgery to residual tumor.
Summary
Although most groups would still advocate for microsurgical debulking of large vestibular schwannomas with evidence of brainstem compression, hybrid treatment strategies have become preferable. More work is required to determine which patients are at risk of progression after a subtotal resection to stratify those who should or should not receive postoperative stereotactic radiosurgery.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Marinelli JP, Lohse CM, Carlson ML. Incidence of vestibular schwannoma over the past half-century: a population-based study of Olmsted County, Minnesota. Otolaryngol Head Neck Surg. 2018;159:717–23.
Stangerup S-E, Tos M, Caye-Thomasen P, Tos T, Klokker M, Thomsen J. Increasing annual incidence of vestibular schwannoma and age at diagnosis. J Laryngol Otol. England. 2004;118:622–7.
Yoshimoto Y. Systematic review of the natural history of vestibular schwannoma. J Neurosurg. United States. 2005;103:59–63.
Leon J, Trifiletti DM, Waddle MR, Vallow L, Ko S, May B, et al. Trends in the initial management of vestibular schwannoma in the United States. J Clin Neurosci. Scotland. 2019;68:174–8.
Torres Maldonado S, Naples JG, Fathy R, Eliades SJ, Lee JYK, Brant JA, et al. Recent trends in vestibular schwannoma management: an 11-year analysis of the National Cancer Database. Otolaryngol Head Neck Surg. England. 2019;161:137–43.
• Goldbrunner R, Weller M, Regis J, Lund-Johansen M, Stavrinou P, Reuss D, et al. EANO guideline on the diagnosis and treatment of vestibular schwannoma. Neuro-Oncology. 2020;22:31–45 This review summarizes guidelines from the European Association for Neuro-Oncology task force for management of vestibular schwannomas.
Koos WT, Day JD, Matula C, Levy DI. Neurotopographic considerations in the microsurgical treatment of small acoustic neurinomas. J Neurosurg. 1998;88:506–12.
Samii M, Matthies C. Management of 1000 vestibular schwannomas (acoustic neuromas): surgical management and results with an emphasis on complications and how to avoid them. Neurosurgery. United States. 1997;40:11–3.
Schneider JR, Chiluwal AK, Arapi O, Kwan K, Dehdashti AR. Near total versus gross total resection of large vestibular schwannomas: facial nerve outcome. Oper Neurosurg (Hagerstown). United States. 2020;19:414–21.
Starnoni D, Daniel RT, Tuleasca C, George M, Levivier M, Messerer M. Systematic review and meta-analysis of the technique of subtotal resection and stereotactic radiosurgery for large vestibular schwannomas: a “nerve-centered” approach. Neurosurg Focus. United States. 2018;44:E4.
Huo M, Foley H, Pinkham M, Shanker M, Bernard A, Jenkins M, et al. Stereotactic radiotherapy for large vestibular schwannomas: volume change following single fraction versus hypofractionated approaches. J Radiosurg SBRT. 2020;7:11–7.
Grinblat G, Dandinarasaiah M, Braverman I, Taibah A, Lisma DG, Sanna M. Large and giant vestibular schwannomas: overall outcomes and the factors influencing facial nerve function. Neurosurg Rev. Germany. 2020.
Machinis TG, Fountas KN, Dimopoulos V, Robinson JS. History of acoustic neurinoma surgery. Neurosurg Focus. United States. 2005;18:e9.
Ren Y, Sethi RKV, Stankovic KM. National Trends in Surgical Resection of Vestibular Schwannomas. Otolaryngol Head Neck Surg. England. 2020;163(6):1244–1249.
Carlson ML, Tveiten OV, Driscoll CL, Goplen FK, Neff BA, Pollock BE, et al. Long-term quality of life in patients with vestibular schwannoma: an international multicenter cross-sectional study comparing microsurgery, stereotactic radiosurgery, observation, and nontumor controls. J Neurosurg. United States. 2015;122:833–42.
Stangerup SE, Caye-Thomasen P, Tos M, Thomsen J. The natural history of vestibular schwannoma. Otol Neurotol. 2006;27(4):547–52.
Marinelli JP, Lees KA, Lohse CM, Driscoll CLW, Neff BA, Link MJ, et al. Natural history of growing sporadic vestibular schwannomas: an argument for continued observation despite documented growth in select cases. Otol Neurotol. United States. 2020;41:e1149–53.
Vivas EX, Carlson ML, Neff BA, Shepard NT, McCracken DJ, Sweeney AD, et al. Congress of neurological surgeons systematic review and evidence-based guidelines on intraoperative cranial nerve monitoring in vestibular schwannoma surgery. Neurosurgery. United States. 2018;82:E44–6.
Morton RP, Ackerman PD, Pisansky MT, Krezalek M, Leonetti JP, Raffin MJM, et al. Prognostic factors for the incidence and recovery of delayed facial nerve palsy after vestibular schwannoma resection. J Neurosurg. United States. 2011;114:375–80.
Anaizi AN, Gantwerker EA, Pensak ML, Theodosopoulos P V. Facial nerve preservation surgery for Koos grade 3 and 4 vestibular schwannomas. Neurosurgery. United States; 2014;75:671–7.
Samii M, Metwali H, Gerganov V. Efficacy of microsurgical tumor removal for treatment of patients with intracanalicular vestibular schwannoma presenting with disabling vestibular symptoms. J Neurosurg. United States. 2017;126:1514–9.
Chiluwal AK, Rothman A, Svrakic M, Dehdashti AR. Surgical outcome in smaller symptomatic vestibular schwannomas. Is there a role for surgery? Acta Neurochir (Wien). Austria. 2018;160:2263–75.
Gurgel RK, Dogru S, Amdur RL, Monfared A. Facial nerve outcomes after surgery for large vestibular schwannomas: do surgical approach and extent of resection matter? Neurosurg Focus. United States. 2012;33:E16.
Seol HJ, Kim C, Park C-K, Kim CH, Kim DG, Chung Y-S, et al. Optimal extent of resection in vestibular schwannoma surgery: relationship to recurrence and facial nerve preservation. Neurol Med Chir (Tokyo). Japan. 2006;46:171–6.
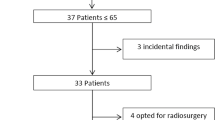
•• Monfared A, Corrales CE, Theodosopoulos P V, Blevins NH, Oghalai JS, Selesnick SH, et al. Facial nerve outcome and tumor control rate as a function of degree of resection in treatment of large acoustic neuromas: preliminary report of the acoustic neuroma subtotal resection study (ANSRS). Neurosurgery. United States; 2016;79:194–203. This prospective multicenter study of patients with vestibular schwannomas ≥ 2.5 cm in diameter demonstrated that less extensive resection was associated with a higher risk of progression on follow-up.
Breshears JD, Morshed RA, Molinaro AM, McDermott MW, Cheung SW, Theodosopoulos PV. Residual Tumor Volume and Location Predict Progression After Primary Subtotal Resection of Sporadic Vestibular Schwannomas: A Retrospective Volumetric Study. Neurosurgery. United States. 2020;86(3):410–416.
Jacob JT, Carlson ML, Driscoll CL, Link MJ. Volumetric analysis of tumor control following subtotal and near-total resection of vestibular schwannoma. Laryngoscope. United States. 2016;126:1877–82.
Schwartz MS, Kari E, Strickland BM, Berliner K, Brackmann DE, House JW, et al. Evaluation of the increased use of partial resection of large vestibular schwannomas: facial nerve outcomes and recurrence/regrowth rates. Otol Neurotol. United States. 2013;34:1456–64.
Strickland BA, Ravina K, Rennert RC, Jackanich A, Aaron K, Bakhsheshian J, et al. Intentional subtotal resection of vestibular schwannoma: a reexamination. J Neurol Surg B Skull Base. 2020;81:136–41.
Jeltema HR, Bakker NA, Bijl HP, Wagemakers M, Metzemaekers JDM, van Dijk JMC. Near total extirpation of vestibular schwannoma with salvage radiosurgery. Laryngoscope. United States. 2015;125:1703–7.
Myrseth E, Møller P, Pedersen P-H, Lund-Johansen M. Vestibular schwannoma: surgery or gamma knife radiosurgery? A prospective, nonrandomized study. Neurosurgery. United States. 2009;64:653–4.
Régis J, Pellet W, Delsanti C, Dufour H, Roche PH, Thomassin JM, et al. Functional outcome after gamma knife surgery or microsurgery for vestibular schwannomas. J Neurosurg. Journal of Neurosurgery Publishing Group; 2002;97:1091–100.
Karpinos M, Teh BS, Zeck O, Carpenter LS, Phan C, Mai W-Y, et al. Treatment of acoustic neuroma: stereotactic radiosurgery vs. microsurgery. Int J Radiat Oncol Biol Phys. United States. 2002;54:1410–21.
Pollock BE, Lunsford LD, Kondziolka D, Flickinger JC, Bissonette DJ, Kelsey SF, et al. Outcome analysis of acoustic neuroma management: a comparison of microsurgery and stereotactic radiosurgery. Neurosurgery. United States. 1995;36:215–9.
Pollock BE, Driscoll CLW, Foote RL, Link MJ, Gorman DA, Bauch CD, et al. Patient outcomes after vestibular schwannoma management: a prospective comparison of microsurgical resection and stereotactic radiosurgery. Neurosurgery. United States. 2006;59:77–85.
Carlson ML, Vivas EX, McCracken DJ, Sweeney AD, Neff BA, Shepard NT, et al. Congress of neurological surgeons systematic review and evidence-based guidelines on hearing preservation outcomes in patients with sporadic vestibular schwannomas. Neurosurgery. United States. 2018;82:E35–9.
Lefranc M, Da Roz LM, Balossier A, Thomassin JM, Roche PH, Regis J. Place of Gamma Knife stereotactic radiosurgery in grade 4 vestibular schwannoma based on case series of 86 patients with long-term follow-up. World Neurosurg. United States. 2018;114:e1192–8.
Huang C-W, Tu H-T, Chuang C-Y, Chang C-S, Chou H-H, Lee M-T, et al. Gamma Knife radiosurgery for large vestibular schwannomas greater than 3 cm in diameter. J Neurosurg. United States. 2018;128:1380–7.
Teo M, Zhang M, Li A, Thompson PA, Tayag AT, Wallach J, et al. The outcome of hypofractionated stereotactic radiosurgery for large vestibular schwannomas. World Neurosurg. United States. 2016;93:398–409.
•• Mezey G, Cahill J, Rowe JG, Yianni J, Bhattacharyya D, Walton L, et al. A retrospective analysis of the role of single-session Gamma Knife stereotactic radiosurgery in sporadic vestibular schwannomas with tumor volumes greater than 10 cm3: is it worth stretching the boundaries? Stereotact Funct Neurosurg. Switzerland; 2020;98:85–94. This is the largest study of large vestibular schwannomas treated with single session SRS. The group observed an overall control rate of 78.6% with 6.2 years of follow-up.
Radwan H, Eisenberg MB, Sandberg Knisely JP, Ghaly MM, Schulder M. Outcomes in patients with vestibular schwannoma after subtotal resection and adjuvant radiosurgery. Stereotact Funct Neurosurg. Switzerland. 2016;94:216–24.
Funding
This study was funded by the National Center for Advancing Translational Sciences of the NIH (RAM) and the Neurosurgery Research and Education Foundation (RAM).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical collection on OTOLOGY: Vestibular Schwannomas
Rights and permissions
About this article
Cite this article
Morshed, R.A., Arora, T. & Theodosopoulos, P.V. Multimodality Treatment of Large Vestibular Schwannomas. Curr Otorhinolaryngol Rep 9, 155–161 (2021). https://doi.org/10.1007/s40136-021-00336-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40136-021-00336-8