Abstract
Background
Homocysteine (Hcy) is an endogenous nonprotein sulfur-containing amino acid biosynthesized from methionine by the removal of its terminal methyl group. Hyperhomocysteinemia (HHcy) has been linked to many systemic disorders, including stroke, proteinuria, epilepsy, psychosis, diabetes, lung disease, and liver disease. The clinical effects of high serum Hcy level, also known as hyperhomocysteinemia, have been explained by different mechanisms. However, little has been reported on the clinical and laboratory findings and etiologies of genetic HHcy in children. This study aimed to examine the relationships between clinical features, laboratory findings, and genetic defects of HHcy.
Methods
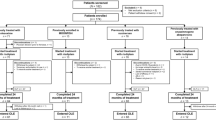
We retrospectively evaluated 20 consecutive children and adolescents with inherited HHcy at the pediatric neurology division of Baskent University, Adana Hospital (Adana, Turkey) between December 2011 and December 2022.
Results
Our main finding is that the most common cause of genetic HHcy is MTHFR mutation. The other main finding is that the Hcy level was higher in patients with CBS deficiency and intracellular cbl defects than in MTHFR mutations. We also found that clinical presentations of genetic HHcy vary widely, and the most common clinical finding is seizures. Here, we report the first and only case of a cbl defect with nonepileptic myoclonus. We also observed that mild and intermediate HHcy associated with the MTHFR mutation may be related to migraine, vertigo, tension-type headache, and idiopathic intracranial hypertension. Although some of the patients were followed up in tertiary care centers for a long time, they were not diagnosed with HHcy. Therefore, we suggest evaluating Hcy levels in children with unexplained neurological symptoms.
Conclusions
Our findings suggest that genetic HHcy might be associated with different clinical manifestations and etiologies. Therefore, we suggest evaluating Hcy levels in children with unexplained neurologic symptoms.


Similar content being viewed by others
Data availability
The data that support the findings of this study are available on request from the corresponding author.
Abbreviations
- Hcy:
-
Homocysteine
- HHcy:
-
Hyperhomocysteinemia
- EEG:
-
Electroencephalographic
- MRI:
-
Magnetic resonance imaging
- PPH:
-
Primary pulmonary hypertension
- FSGS:
-
Focal glomerular sclerosis
- CBS:
-
Cystathionine b-synthase
- CSF:
-
Cerebrospinal fluid pressure
- IIH:
-
İDiopathic cranial hypertension
- RAO:
-
Retinal artery occlusion
- MR:
-
Mental retardation
References
Zaric BL, Obradovic M, Bajic V, Haidara MA, Jovanovic M, Isenovic ER (2019) Homocysteine and hyperhomocysteinaemia. Curr Med Chem 26(16):2948–2961. https://doi.org/10.2174/0929867325666180313105949
Graham IM, Daly LE, Refsum HM et al (1997) Plasma homocysteine as a risk factor for vascular disease. Eur Concerted Action Project JAMA 277(22):1775–1781. https://doi.org/10.1001/jama.1997.03540460039030
Coban-Karatas M, Erol I, Ozkale Y, Yazıcı N (2013) Central retinal artery occlusion in a 13-year-old child as a presenting sign of hyperhomocysteinemia together with high lipoprotein(a) level. Pediatr Neurol 49(2):138–140. https://doi.org/10.1016/j.pediatrneurol.2013.04.002
Thurtell MJ, Bruce BB, Newman NJ, Biousse V (2010). An update on idiopathic intracranial hypertension. Rev Neurol Dis; 7(2–3):e56–68. PMID: 20944524; PMCID: PMC3674489
Muttamthottil Varghese Francis. Brief migraine episodes in children and adolescents-a modification to International Headache Society pediatric migraine (without aura) diagnostic criteria. Springerplus. 2(1):77. https://doi.org/10.1186/2193-1801-2-77
Stern LL, Bagley PJ, Rosenberg IH (2000) Conversion of 5-formyltetrahydrofolic acid is unimpaired in folate-adequate persons homozygous for the C677T mutation in the methylenetetrahydrofolate reductase gene. J Nutr 130(9):2238–2242. https://doi.org/10.1093/jn/130.9.2238
Lopaciuk S, Bykowska K, Kwiecinski H et al (2001) Factor V Leiden, prothrombin gene G20210A variant, and methylenetetrahydrofolat reductase C677T genotype in young adults with ischemic stroke. Clin Appl Thromb Hemost 7(4):346–350. https://doi.org/10.1177/107602960100700418
Markus HS, Ali N, Swaminathan R, Sankaralingam A, Molloy J, Powell J (1997) A common polymorphism in the methylenetetrahydrofolat reductase gene, homocysteine, and ischemic cerebrovascular disease. Stroke 28(9):1739–1743. https://doi.org/10.1161/01.str.28.9.1739
Ho PI, Collins SC, Dhitavat S et al (2001) Homocysteine potentiatesbeta-amyloid neurotoxicity: role of oxidative stres. J Neurochem 78(2):249–253. https://doi.org/10.1046/j.1471-4159.2001.00384.x
Homberger G, Linnebank M, Winter C (2000) Genomic structure and transcript variants of the human methylenetetrahydrofolate reductase gene. Eur J Hum Genet 8(9):725–729. https://doi.org/10.1038/sj.ejhg.5200522
Ono H, Sakamoto A, Mizoguchi N, Sakura N (2002) The C677Tmutation in the methylenetetrahydrofolate reductase gene contributesto hyperhomocysteinemia in patients taking anticonvulsants. Brain Dev 24(4):223–226. https://doi.org/10.1016/s0387-7604(02)00004-9
Prasad AN, Rupar CA, Prasad C (2011) Methylenetetrahydrofolate reductase (MTHFR) deficiency and infantile epilepsy. Brain Dev 33(9):758–769. https://doi.org/10.1016/j.braindev.2011.05.014
Van der Put NM, Gabreels F, Stevens EM et al (1998). A second common mutation in the methylenetetrahydrofolate reductase gene: an additional risk factor for neural-tube defects? Am J Hum Genet 62(5):1044–1O51 https://doi.org/10.1086/301825.
Molloy AM, Daly S, Mills JL et al (1997) Thermolabile variant of 5,10-methylenetetrahydrofolate reductase associated with low red-cell folates: implications for folate intake recommendations. Lancet 349(9065):1591–1593. https://doi.org/10.1016/S0140-6736(96)12049-3
Van der Put NM, Steegers-Theunissen RP, Frosst P et al (1995) Mutated methylenetetrahydro folate reductase as a risk factor for spina bifida. Lancet 346(8982):1070–10711. https://doi.org/10.1016/s0140-6736(95)91743-8
Vurucu S, Demirkaya E, Kul M et al (2008) Evaluation of the relationship between C677T variants of methylenetetrahydro folate reductase gene and hyperhomocysteinemiain children receiving antiepileptic drug therapy. Prog Neuro- Psychopharmacol Biol Psychiatry 32(3):844–848. https://doi.org/10.1016/j.pnpbp.2007.12.018
Wu YL, Yang HY, Ding XX et al (2014) Association between methylene tetrahydrofolate reductase C677T polymorphism and epilepsy susceptibility: a meta-analysis. Seizure 23(6):411–416. https://doi.org/10.1016/j.seizure.2014.01.018
Lipton SA, Kim WK, Choi YB et al (1997) Neurotoxicity associated with dual actions of homocysteine at the N-methyl-D-aspartate receptor. Proc Natl Acad Sci U S A 94(11):5923–5928. https://doi.org/10.1073/pnas.94.11.5923
Rai V, Kumar P (2018) Methylenetetrahydrofolate reductase C677T polymorphism and susceptibility to epilepsy. Neurol Sci 39(12):2033–2041. https://doi.org/10.1007/s10072-018-3583-z
Liew SC, Gupta ED (2015) Methylenetetrahydrofolate reductase (MTHFR) C677T polymorphism: epidemiology, metabolism and the associated diseases. Eur J Med Genet 58(1):1–10. https://doi.org/10.1016/j.ejmg.2014.10.004
Karabiber H, Sonmezgoz E, Ozerol E, Yakinci C, Otlu B, Yologlu S (2003) Effects of valproate and carbamazepine on serum levels of homocysteine, vitamin B12, and folic acid. Brain Dev 25(2):113–115. https://doi.org/10.1016/s0387-7604(02)00163-8
Fu Y, Wang X, Kong W (2018) Hyperhomocysteinaemia and vascular injury: advances in mechanisms and drug targets. Br J Pharmacol 58(1):1–10. https://doi.org/10.1016/j.ejmg.2014.10.004
Lee EJ, Cho YJ, Yoon YJ (2010) Methylenetetrahydrofolate reductase C677T gene mutation as risk factor for sudden sensorineural hearing loss: association with plasma homocysteine, folate and cholesterol concentrations. J Laryngol Otol 124(12):1268–1273. https://doi.org/10.1017/S002221511000099X
Scaramella JG (2003) Hyperhomocysteinemia and left internal jugular vein thrombosis with Ménière’s symptom complex. Ear Nose Throat J 82(11):856
Weiss N (2005) Mechanisms of increased vascular oxidant stress in hyperhomocys-teinemia and its impact on endothelial function. Curr Drug Metab 6(1):27–36. https://doi.org/10.2174/1389200052997357
De Bruijn SF, de Haan RJ, Stam J (2001) Clinical features and prognostic factors of cerebral venous sinus thrombosis in a prospective series of 59 patients for the cerebral venous sinus thrombosis study group. J Neurol Neurosurg Psychiatry 70(1):105–108. https://doi.org/10.1136/jnnp.70.1.105
Yetgin S, Derman O, Dogan M (2006) A pediatric patient with recurrent pseudotumor cerebri and vitamin b12 deficiency. Pediatr Hematol Oncol 23(1):39–43. https://doi.org/10.1080/08880010500313322
Kara I, Sazci A, Ergul E, Kaya G, Kilic G (2003) Association of the C677T and A1298C polymorphisms in the 5,10 methylenetetrahydrofolate reductase gene in patients with migraine risk. Brain Res Mol Brain Res 111(1–2):84–90. https://doi.org/10.1016/s0169-328x(02)00672-1
Rainero I, Vacca A, Roveta F, Govone F, Gai A, Rubino E (2019) Targeting MTHFR for the treatment of migraines. Expert Opin Ther Targets 23(1):29–37. https://doi.org/10.1080/14728222.2019.1549544
Yeganeh F, Nikbakht F, Bahmanpour S, Rastegar K, Namavar RJ (2013) Neuroprotective effects of NMDA and group I metabotropic glutamate receptor antagonists against neurodegeneration induced by homocysteine in rat hippocampus: in vivo study. Mol Neurosci 50(3):551–557. https://doi.org/10.1007/s12031-013-9996-5
Lossos A, Teltsh O, Milman T et al (2014) Severe methylenetetrahydrofolate reductase deficiency: clinical clues to a potentially treatable cause of adult-onset hereditary spastic paraplegia. JAMA Neurol 71(7):901–4. https://doi.org/10.1001/jamaneurol.2014
Marelli C, Lavigne C, Stepien KM et al (2021) Clinical and molecular characterization of adult patients with late-onset MTHFR deficiency. J Inherit Metab Dis 44(3):777–786. https://doi.org/10.1002/jimd.12323
Bottiglieri T, Parnetti L, Arning E et al (2001) Plasma total homocysteine levels and the C677T mutation in the methylenetetrahydrofolate reductase (MTHFR) gene: a study in an Italian population with dementia. Mech Ageing Dev 122(16):2013–2023. https://doi.org/10.1016/s0047-6374(01)00307-4
Altun H, Şahin N, Belge Kurutaş E, Güngör O (2018) Homocysteine, pyridoxine, folate and vitamin B12 levels in children with attention deficit hyperactivity disorder. Psychiatr Danub 30(3):310–316. https://doi.org/10.24869/psyd.2018.310
Pavone V, Praticò AD, Parano E, Pavone P, Verrotti A, Falsaperla R (2012) Spine and brain malformations in a patient obligate carrier of MTHFR with autism and mental retardation. Clin Neurol Neurosurg 114(9):1280–1282. https://doi.org/10.1016/j.clineuro.2012.03.008
Huemer M, Diodato D, Martinelli D et al (2019) Phenotype, treatment practice and outcome in the cobalamin-dependent remethylation disorders and MTHFR deficiency: data from the E-HOD registry. J Inherit Metab Dis 42(2):333–352. https://doi.org/10.1002/jimd.12041
Huemer M, Diodato D, Schwahn B et al (2017) Guidelines for diagnosis and management of the cobalamin-related remethylation disorders cblC, cblD, cblE, cblF, cblG, cblJ and MTHFR deficiency. J Inherit Metab Dis 40(1):21–48. https://doi.org/10.1007/s10545-016-9991-4
Li DX, Li XY, Dong H et al (2018) Eight novel mutations of CBS gene in nine Chinese patients with classical homocystinuria. World J Pediatr 14(2):197–203. https://doi.org/10.1007/s12519-018-0135-9
Huemer M, Kožich V, Rinaldo P et al (2015) Newborn screening for homocystinurias and methylation disorders: systematic review and proposed guidelines. J Inherit Metab Dis 38(6):1007–1019. https://doi.org/10.1007/s10545-015-9830-z
Funding
The authors declare that this study did not receive any financial support.
Author information
Authors and Affiliations
Contributions
ŞB wrote the manuscript. ŞB, YÖ, İE, SC, and AN were involved in patient care, including administration of medication and routine clinical follow-up. İE, YÖ, ŞB reviewed the results and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare there are no conflicts of interest financial or otherwise related to the material presented herein.
Ethical approval
Our study was approved by the Baskent University Institutional Review Board and Ethics Committee. The approvement number is KA20/120. Written informed consent was obtained from the parents of all participants.
Copyright form disclosure
The authors disclosed government work.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Besen, S., Ozkale, Y., Ceylaner, S. et al. Clinical and laboratory findings and etiologies of genetic homocystinemia: a single-center experience. Acta Neurol Belg 124, 213–222 (2024). https://doi.org/10.1007/s13760-023-02356-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13760-023-02356-1