Abstract
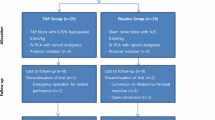
Local anesthesia in laparoscopic operations is gaining increasing consensus. To standardize analgesia, a prospective case–control study was created over a 1-year period, in collaboration with the anesthesiology service in our community hospital. Starting from February 2016, we prospectively enrolled adult patients (more than 16 years old) undergoing laparoscopic appendectomy or cholecystectomy, either in emergency or elective setting. Patients were preoperatively assigned (based on the chart-admission number) either to transversus abdominis plane (TAP) block treatment (Group 1—experimental arm) or trocar-site anesthesia (TSA) (Group 2—experimental arm), and then compared with group of patients not submitted to treatment (Group 3—control arm). Demographic and clinical characteristics of each patient were recorded. Post-operative pain level (primary outcome) was assessed with visual analog scale (VAS) score; analgesic use and length of stay in hospital were defined as secondary outcomes. Forty-two patients were assigned to TAP block treatment (Group 1), fifty-two to TSA (Group 2), and thirty-nine underwent no pre-incisional treatment (Group 3). In the comparison between patients undergoing TAP block or TSA with the control arm, a significance difference in reported pain was recorded in every scheduled time (p < 0.05 at 0, 6, 12, 18, 24, and 48 h from awakening). Both local anesthesia groups share a benefit in terms of primary outcome. The use of pre-incisional TSA for all the patients undergoing laparoscopic cholecystectomy and appendectomy could become a routine practice to reduce post-operative pain both in the elective and emergency setting.

Similar content being viewed by others
References
Loizides S, Gurusamy KS, Nagendran M, Rossi M, Guerrini GP, Davidson BR (2014) Wound infiltration with local anesthetic agents for laparoscopic cholecystectomy. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.cd007049.pub2(Review. PMID: 24619479)
Charlton S, Cyna AM, Middleton P, Griffiths JD (2010) Perioperative transversus abdominis plane (TAP) block analgesia after abdominal surgery. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.cd007705.pub2
Gurusamy KS, Vaughan J, Toon CD, Davidson BR (2014) Pharmacological interventions for prevention or treatment of postoperative pain in people undergoing laparoscopic cholecystectomy. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.cd008261.pub2
Magee C, Clarke C, Lewis A (2011) Laparoscopic TAP block for laparoscopic cholecystectomy: description of a novel technique. Surgeon 9(6):352–353. https://doi.org/10.1016/j.surge.2010.11.027
Tihan D, Totoz T, Tokocin M, Ercan G, Koc Calıkoglu T, Vartanoglu T, Celebi F, Dandin O, Kafa IM (2016) Efficacy of laparoscopic transversus abdominis plane block for elective laparoscopic cholecystectomy in elderly patients. Bosn J Basic Med Sci 16(2):139–144. https://doi.org/10.17305/bjbms.2016.841
Fields AC, Gonzalez DO, Chin EH, Nguyen SQ, Zhang LP, Divino CM (2015) Laparoscopic assisted transversus abdominis plane block for postoperative pain control in laparoscopic ventral hernia repair: a randomized-controlled trial. J Am Coll Surg 221(2):462–469. https://doi.org/10.1016/j.jamcollsurg.2015.04.007
Carney J, McDonnell JG, Ochana A, Bhinder R, Laffey JG (2008) The transversus abdominis plane block provides effective analgesia in patients undergoing total abdominal hysterectomy. Anesth Analg 107(6):2056–2060. https://doi.org/10.1213/ane.0b013e3181871313
Elkassabany N, Ahmed M, Malkowicz SB, Heitjan DF, Isserman JA, Ochroch EA (2013) Comparison between the analgesic efficacy of TAP block and placebo in open retropubic radical prostatectomy: a prospective, randomized, double blind study. J Clin Anesth 25(6):459–465. https://doi.org/10.1016/j.jclinane.2013.04.009
McDonnell JG, Curley G, Carney J, Benton A, Costello J, Maharaj CH, Laffey JG (2008) The analgesic efficacy of transversus plane block after cesarean delivery: a randomized controlled trial. Anesth Analg 106(1):186–191. https://doi.org/10.1213/01.ane.0000290294.64090.f3(table of contents)
Yu N, Long X, Lujan-Hernandez JR, Succar J, Xin X, Wang X (2014) Transversus abdominis Plane block versus local anesthetic wound infiltration in lower abdominal surgery: a systematic review and meta-analysis of randomized controlled trials. BMC Anesthesiol 15(14):121. https://doi.org/10.1186/1471-2253-14-121
El Hachem L, Small E, Chung P, Moshier EL, Friedman K, Fenske SS, Gretz HF 3rd (2015) Randomized controlled double-blind trial of transversus abdominis plane block versus trocar site infiltration in gynecologic laparoscopy. Am J Obstet Gynecol. 212(2):182.e-91. https://doi.org/10.1016/j.ajog.2014.07.049
Tam T, Harkins G, Wegrzyniak L, Ehrgood S, Kunselman A, Davies M (2014) Infiltration of bupivacaine local anesthetic to trocar insertion sites after laparoscopy: a randomized, double-blind, stratified, and controlled trial. J Minim Invasive Gynecol 21(6):1015–1021. https://doi.org/10.1016/j.jmig.2014.04.013
Saxena R, Joshi S, Srivastava K, Tiwari S, Sharma N, Valecha UK (2016) Comparative study of ultrasound-guided abdominal field blocks versus port infiltration in laparoscopic cholecystectomies for post-operative pain relief. Indian J Anaesth 60(8):578–583. https://doi.org/10.4103/0019-5049.187790
Bava EP, Ramachandran R, Rewari V, Chandralekha Bansal VK, Trikha A (2016) Analgesic efficacy of ultrasound guided transversus abdominis plane block versus local anesthetic infiltration in adult patients undergoing single incision laparoscopic cholecystectomy: a randomized controlled trial. Anesth Essays Res 10(3):561–567
Savoia G, Alampi D, Amantea B, Ambrosio F, Arcioni R, Berti M, Bettelli G, Bertini L, Bosco M, Casati A, Castelletti I, Carassiti M, Coluzzi F, Costantini A, Danelli G, Evangelista M, Finco G, Gatti A, Gravino E, Launo C, Loreto M, Mediati R, Mokini Z, Mondello E, Palermo S, Paoletti F, Paolicchi A, Petrini F, Piacevoli Q, Rizza A, Sabato AF, Santangelo E, Troglio E, Mattia C, SIAARTI Study Group (2010) Postoperative pain treatment SIAARTI Recommendations 2010 Short version. Minerva Anestesiol 76(8):657–667
Oksar M, Koyuncu O, Turhanoglu S, Temiz M, Oran MC (2016) Transversus abdominis plane block as a component of multimodal analgesia for laparoscopic cholecystectomy. J Clin Anesth 34:72–78. https://doi.org/10.1016/j.jclinane.2016.03.033
Coughlin SM, Karanicolas PJ, Emmerton-Coughlin HM, Kanbur B, Kanbur S, Colquhoun PH (2010) Better late than never? Impact of local analgesia timing on postoperative pain in laparoscopic surgery: a systematic review and metaanalysis. Surg Endosc 24(12):3167–3176. https://doi.org/10.1007/s00464-010-1111-1
Abdallah FW, Chan VW, Brull R (2012) Transversus abdominis plane block: a systematic review. Reg Anesth Pain Med 37(2):193–209. https://doi.org/10.1097/AAP.0b013e3182429531(Review. PubMed PMID: 22286518)
Hasaniya NW, Zayed FF, Faiz H, Severino R (2001) Preinsertion local anesthesia at the trocar site improves perioperative pain and decreases costs of laparoscopic cholecystectomy. Surg Endosc 15(9):962–964
Souto MM, Radaelli E, Giordani AE, Savaris A, Bassols GF (2015) Effectiveness of local anesthetics in laparoscopic cholecystectomy: a randomized clinical trial. Surg Laparosc Endosc Percutan Tech 25(4):317–320. https://doi.org/10.1097/sle.0000000000000166
Altuntas G, Akkaya ÖT, Özkan D, Sayin MM, Balas S, Özlü E (2016) Comparison of intraabdominal and trocar site local anaesthetic infiltration on postoperative analgesia after laparoscopic cholecystectomy. Turk J Anaesthesiol Reanim 44(6):306–311. https://doi.org/10.5152/tjar.2016.75983
Leone S, Di Cianni S, Casati A, Fanelli G (2008) Pharmacology, toxicology, and clinical use of new long acting local anesthetics, ropivacaine and levobupivacaine. Acta Biomed 79(2):92–105 (Review. PMID: 18788503)
Vitale SG, Gasbarro N, Lagana AS, Sapia F, Rapisarda AMC, Valenti G, Trovato MA, Rossetti D, Chiofalo B, Barrasso G, Tinelli A, Corrado F (2016) Safe introduction of ancillary trocars in gynecological surgery: the “yellow island” anatomical landmark. Ann Ital Chir 87:608–611 (PMID: 27909270)
Rondelli F, Manina G, Agnelli G, Becattini C (2013) Venous thromboembolism after laparoscopic cholecystectomy: clinical burden and prevention. Surg Endosc 27(6):1860–1864. https://doi.org/10.1007/s00464-012-2717-2
Sturlese E, Triolo O, Grasso R, Laganà AS, Retto A, Rossetti D, Vitale SG, Sarpietro G, De Dominici R (2017) Thromboembolism prophylaxis in laparoscopic surgery for gynecologic benign diseases. Results of a single center experience in 922 procedures. Ann Ital Chir 88:342–347 (PMID: 28590256)
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This research involving human participants was in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Research involving human participants and/or animals
This research involved human participants who supplied their own consent. This study was performed in accordance with the ethical standards of the Declaration of Helsinki. All authors disclose any financial and personal relationships with other people or organizations that could inappropriately influence this study.
Informed consent
For this type of study, formal consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Molfino, S., Botteri, E., Baggi, P. et al. Pain control in laparoscopic surgery: a case–control study between transversus abdominis plane-block and trocar-site anesthesia. Updates Surg 71, 717–722 (2019). https://doi.org/10.1007/s13304-018-00615-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13304-018-00615-y