Abstract
As alternative blood supply routes, collateral blood vessels can play a crucial role in determining patient outcomes in acute and chronic intracranial occlusive diseases. Studies have shown that increased collateral circulation can improve functional outcomes and reduce mortality, particularly in those who are not eligible for reperfusion therapy. This article aims to discuss the anatomy and physiology of collateral circulation, describe current imaging tools used to measure collateral circulation, and identify the factors that influence collateral status.




Similar content being viewed by others
Data Availability
Not applicable.
References
Liebeskind DS. Collateral Circulation. Stroke. 2003;34:2279–84. https://doi.org/10.1161/01.STR.0000086465.41263.06.
Vasquez HE, Murlimanju BV, Shrivastava A, Durango-Espinosa YA, Joaquim AF, Garcia-Ballestas E, Moscote-Salazar LR, Agrawal A. Intracranial collateral circulation and its role in neurovascular pathology. Egypt J Neurosurg. 2021;36:2. https://doi.org/10.1186/s41984-020-00095-6.
Bang OY, Goyal M, Liebeskind DS. Collateral Circulation in Ischemic Stroke. Stroke. 2015;46:3302–9. https://doi.org/10.1161/STROKEAHA.115.010508.
Gunnal SA, Farooqui MS, Wabale RN. Anatomical variations of the circulus arteriosus in cadaveric human brains. Neurol Res Int. 2014;2014:687281. https://doi.org/10.1155/2014/687281.
Faber JE, Chilian WM, Deindl E, van Royen N, Simons M. A brief etymology of the collateral circulation. Arterioscler Thromb Vasc Biol. 2014;34:1854–9. https://doi.org/10.1161/atvbaha.114.303929.
Malhotra K, Liebeskind DS. Collaterals in ischemic stroke. Brain Hemorrhages. 2020;1:6–12. https://doi.org/10.1016/j.hest.2019.12.003.
Bang OY, Saver JL, Kim SJ, Kim G-M, Chung C-S, Ovbiagele B, Lee KH, Liebeskind DS. Collateral flow averts hemorrhagic transformation after endovascular therapy for acute ischemic stroke. Stroke. 2011;42:2235–9. https://doi.org/10.1161/STROKEAHA.110.604603.
Liebeskind DS, Saber H, Xiang B, Jadhav AP, Jovin TG, Haussen DC, Budzik RF, Bonafe A, Bhuva P, Yavagal DR, Hanel RA, Ribo M, Cognard C, Sila C, Hassan AE, Smith WS, Saver JL, Nogueira RG. Collateral circulation in thrombectomy for stroke after 6 to 24 hours in the DAWN trial. Stroke. 0:STROKEAHA.121.034471. https://doi.org/10.1161/STROKEAHA.121.034471
Fiehler J, Remmele C, Kucinski T, Rosenkranz M, Thomalla G, Weiller C, Zeumer H, Röther J. Reperfusion after severe local perfusion deficit precedes hemorrhagic transformation: an MRI study in acute stroke patients. Cerebrovasc Dis (Basel Switzerland). 2005;19:117–24. https://doi.org/10.1159/000083180.
Bang OY, Saver JL, Kim SJ, Kim G-M, Chung C-S, Ovbiagele B, Lee KH, Liebeskind DS. Collateral flow predicts response to endovascular therapy for acute ischemic stroke. Stroke. 2011;42:693–9. https://doi.org/10.1161/strokeaha.110.595256.
Souza LC, Yoo AJ, Chaudhry ZA, Payabvash S, Kemmling A, Schaefer PW, Hirsch JA, Furie KL, González RG, Nogueira RG, Lev MH. Malignant CTA collateral profile is highly specific for large admission DWI infarct core and poor outcome in acute stroke. AJNR Am J Neuroradiol. 2012;33:1331–6. https://doi.org/10.3174/ajnr.A2985.
Tong E, Patrie J, Tong S, Evans A, Michel P, Eskandari A, Wintermark M. Time-resolved CT assessment of collaterals as imaging biomarkers to predict clinical outcomes in acute ischemic stroke. Neuroradiology. 2017;59:1101–9. https://doi.org/10.1007/s00234-017-1914-z.
Choi JY, Kim EJ, Hong JM, Lee SE, Lee JS, Lim YC, Kim HS. Conventional enhancement CT: a valuable tool for evaluating pial collateral flow in acute ischemic stroke. Cerebrovasc Dis. 2011;31:346–52. https://doi.org/10.1159/000322602.
Bhatia R, Bal SS, Shobha N, Menon BK, Tymchuk S, Puetz V, Dzialowski I, Coutts SB, Goyal M, Barber PA, Watson T, Smith EE, Demchuk AM. CT Angiographic source images predict outcome and final infarct volume better than noncontrast CT in proximal vascular occlusions. Stroke. 2011;42:1575–80. https://doi.org/10.1161/STROKEAHA.110.603936.
Schramm P, Schellinger PD, Klotz E, Kallenberg K, Fiebach JB, Külkens S, Heiland S, Knauth M, Sartor K. Comparison of perfusion computed tomography and computed tomography angiography source images with perfusion-weighted imaging and diffusion-weighted imaging in patients with acute stroke of less than 6 hours’ duration. Stroke. 2004;35:1652–8. https://doi.org/10.1161/01.STR.0000131271.54098.22.
Lee KH, Lee SJ, Cho SJ, Na DG, Byun HS, Kim YB, Song HJ, Jin IS, Chung CS. Usefulness of triphasic perfusion computed tomography for intravenous thrombolysis with tissue-type plasminogen activator in acute ischemic stroke. Arch Neurol. 2000;57:1000–8. https://doi.org/10.1001/archneur.57.7.1000.
Dundamadappa S, Iyer K, Agrawal A, Choi DJ. Multiphase CT Angiography: A useful technique in acute stroke imaging—collaterals and beyond. Am J Neuroradiol. 2020. https://doi.org/10.3174/ajnr.A6889.
Lee SJ, Lee KH, Na DG, Byun HS, Kim YB, Shon YM, Cho SJ, Lee J, Chung CS, Hong SC. Multiphasic helical computed tomography predicts subsequent development of severe brain edema in acute ischemic stroke. Arch Neurol. 2004;61:505–9. https://doi.org/10.1001/archneur.61.4.505.
Menon BK, d’Esterre CD, Qazi EM, Almekhlafi M, Hahn L, Demchuk AM, Goyal M. Multiphase CT Angiography: a new tool for the imaging triage of patients with acute ischemic stroke. Radiology. 2015;275:510–20. https://doi.org/10.1148/radiol.15142256.
Albers GW, Marks MP, Kemp S, Christensen S, Tsai JP, Ortega-Gutierrez S, McTaggart RA, Torbey MT, Kim-Tenser M, Leslie-Mazwi T, Sarraj A, Kasner SE, Ansari SA, Yeatts SD, Hamilton S, Mlynash M, Heit JJ, Zaharchuk G, Kim S, Carrozzella J, Palesch YY, Demchuk AM, Bammer R, Lavori PW, Broderick JP, Lansberg MG. Thrombectomy for stroke at 6 to 16 hours with selection by perfusion imaging. N Engl J Med. 2018;378:708–18. https://doi.org/10.1056/NEJMoa1713973.
Nogueira RG, Jadhav AP, Haussen DC, Bonafe A, Budzik RF, Bhuva P, Yavagal DR, Ribo M, Cognard C, Hanel RA, Sila CA, Hassan AE, Millan M, Levy EI, Mitchell P, Chen M, English JD, Shah QA, Silver FL, Pereira VM, Mehta BP, Baxter BW, Abraham MG, Cardona P, Veznedaroglu E, Hellinger FR, Feng L, Kirmani JF, Lopes DK, Jankowitz BT, Frankel MR, Costalat V, Vora NA, Yoo AJ, Malik AM, Furlan AJ, Rubiera M, Aghaebrahim A, Olivot J-M, Tekle WG, Shields R, Graves T, Lewis RJ, Smith WS, Liebeskind DS, Saver JL, Jovin TG. Thrombectomy 6 to 24 hours after stroke with a mismatch between deficit and infarct. N Engl J Med. 2017;378:11–21. https://doi.org/10.1056/NEJMoa1706442.
Ma H, Campbell BCV, Parsons MW, Churilov L, Levi CR, Hsu C, Kleinig TJ, Wijeratne T, Curtze S, Dewey HM, Miteff F, Tsai C-H, Lee J-T, Phan TG, Mahant N, Sun M-C, Krause M, Sturm J, Grimley R, Chen C-H, Hu C-J, Wong AA, Field D, Sun Y, Barber PA, Sabet A, Jannes J, Jeng J-S, Clissold B, Markus R, Lin C-H, Lien L-M, Bladin CF, Christensen S, Yassi N, Sharma G, Bivard A, Desmond PM, Yan B, Mitchell PJ, Thijs V, Carey L, Meretoja A, Davis SM, Donnan GA. Thrombolysis guided by perfusion imaging up to 9 hours after onset of stroke. N Engl J Med. 2019;380:1795–803. https://doi.org/10.1056/NEJMoa1813046.
Demeestere J, Wouters A, Christensen S, Lemmens R, Lansberg MG. Review of perfusion imaging in acute ischemic stroke. Stroke. 2020;51:1017–24. https://doi.org/10.1161/STROKEAHA.119.028337.
Tan JC, Dillon WP, Liu S, Adler F, Smith WS, Wintermark M. Systematic comparison of perfusion-CT and CT-angiography in acute stroke patients. Ann Neurol. 2007;61:533–43. https://doi.org/10.1002/ana.21130.
Lin L, Chen C, Tian H, Bivard A, Spratt N, Levi CR, Parsons MW. Perfusion computed tomography accurately quantifies collateral flow after acute ischemic stroke. Stroke. 2020;51:1006–9. https://doi.org/10.1161/STROKEAHA.119.028284.
Nael K, Sakai Y, Larson J, Goldstein J, Deutsch J, Awad AJ, Pawha P, Aggarwal A, Fifi J, Deleacy R, Yaniv G, Wintermark M, Liebeskind DS, Shoirah H, Mocco J. CT perfusion collateral index in assessment of collaterals in acute ischemic stroke with delayed presentation: comparison to single phase CTA. J Neuroradiol = J Neuroradiol. 2021; https://doi.org/10.1016/j.neurad.2021.11.002.
Olivot JM, Mlynash M, Inoue M, Marks MP, Wheeler HM, Kemp S, Straka M, Zaharchuk G, Bammer R, Lansberg MG, Albers GW. Hypoperfusion intensity ratio predicts infarct progression and functional outcome in the DEFUSE 2 cohort. Stroke. 2014;45:1018–23. https://doi.org/10.1161/STROKEAHA.113.003857.
Nomani AZ, KamtchumTatuene J, Rempel JL, Jeerakathil T, Winship IR, Khan KA, Buck BH, Shuaib A, Jickling GC. Association of CT-based hypoperfusion index with ischemic core enlargement in patients with medium and large vessel stroke. Neurology. 2021;97:e2079–87. https://doi.org/10.1212/wnl.0000000000012855.
Tsui B, Chen I, Qiao J, Khatibi K, Mejia LP, Liebeskind DS, Sharma LK, Tateshima S, Hosseini MB, Colby G, Nour M, Salamon N, Saver J, Jahan R, Duckwiler G, Nael K. Abstract P348: Perfusion collateral index vs. hypoperfusion intensity ratio in assessment of angiographic collateral scores in patients with acute ischemic stroke. Stroke. 2021;52:AP348–AP348. https://doi.org/10.1161/str.52.suppl_1.P348.
Kim SJ, Ha YS, Ryoo S, Noh HJ, Ha S-Y, Bang OY, Kim G-M, Chung C-S, Lee KH. Sulcal effacement on fluid attenuation inversion recovery magnetic resonance imaging in hyperacute stroke. Stroke. 2012;43:386–92. https://doi.org/10.1161/STROKEAHA.111.638106.
Lee KY, Latour LL, Luby M, Hsia AW, Merino JG, Warach S. Distal hyperintense vessels on FLAIR: an MRI marker for collateral circulation in acute stroke? Neurology. 2009;72:1134–9. https://doi.org/10.1212/01.wnl.0000345360.80382.69.
Nael K, Khan R, Choudhary G, Meshksar A, Villablanca P, Tay J, Drake K, Coull BM, Kidwell CS. Six-minute magnetic resonance imaging protocol for evaluation of acute ischemic stroke: pushing the boundaries. Stroke. 2014;45:1985–91. https://doi.org/10.1161/strokeaha.114.005305.
Bang OY, Chung J-W, Son JP, Ryu W-S, Kim D-E, Seo W-K, Kim G-M, Kim Y-C. Multimodal MRI-based triage for acute stroke therapy: challenges and progress. Front Neurol. 2018, 9. https://doi.org/10.3389/fneur.2018.00586.
Lee MJ, Son JP, Kim SJ, Ryoo S, Woo S-Y, Cha J, Kim G-M, Chung C-S, Lee KH, Bang OY. Predicting collateral status with magnetic resonance perfusion parameters. Stroke. 2015;46:2800–7. https://doi.org/10.1161/STROKEAHA.115.009828.
Nael K, Doshi A, De Leacy R, Puig J, Castellanos M, Bederson J, Naidich TP, Mocco J, Wintermark M. MR perfusion to determine the status of collaterals in patients with acute ischemic stroke: a look beyond time maps. Am J Neuroradiol. 2018;39:219–25. https://doi.org/10.3174/ajnr.A5454.
Haller S, Zaharchuk G, Thomas DL, Lovblad KO, Barkhof F, Golay X. Arterial spin labeling perfusion of the brain: emerging clinical applications. Radiology. 2016;281:337–56. https://doi.org/10.1148/radiol.2016150789.
Zaharchuk G, Do HM, Marks MP, Rosenberg J, Moseley ME, Steinberg GK. Arterial spin-labeling MRI can identify the presence and intensity of collateral perfusion in patients with moyamoya disease. Stroke. 2011;42:2485–91. https://doi.org/10.1161/STROKEAHA.111.616466.
Guan J, Zhang S, Zhou Q, Li C, Lu Z. Usefulness of transcranial doppler ultrasound in evaluating cervical-cranial collateral circulations. Interv Neurol. 2013;2:8–18. https://doi.org/10.1159/000354732.
Wiegers EJA, Mulder MJHL, Jansen IGH, Venema E, Compagne KCJ, Berkhemer OA, Emmer BJ, Marquering HA, Es ACGMv, Sprengers ME, Zwam WHv, Oostenbrugge RJv, Roos YBWEM, Majoie CBLM, Roozenbeek B, Lingsma HF, Dippel DWJ, Lugt Avd, Boiten J, Vos JA, Brouwer J, Hartog SJd, Hinsenveld WH, Kappelhof M, Goldhoorn R-JB, Coutinho JM, Schonewille WJ, Vos JA, Wermer MJH, Walderveen MAAv, Staals J, Hofmeijer J, Martens JM, Nijeholt GJLà, Bruijn SFd, Dijk LCv, Worp HBvd, Lo RH, Dijk EJv, Boogaarts HD, Vries Jd, Kort PLMd, Tuijl Jv, Peluso JJP, Fransen P, Berg JSPvd, Hasselt BAAMv, Aerden LAM, Dallinga RJ, Uyttenboogaart M, Eschgi O, Bokkers RPH, Schreuder THCML, Heijboer RJJ, Keizer K, Yo LSF, Hertog HMd, Sturm EJC, Brouwers P, Nijeholt GJLà, Walderveen MAAv, Jenniskens SFM, Berg Rvd, Yoo AJ, Beenen LFM, Postma AA, Roosendaal SD, Kallen BFWvd, Wijngaard IRvd, Martens JM, Yo LSF, Vos JA, Bot J, Doormaal P-Jv, Meijer A, Ghariq E, Bokkers RPH, Proosdij MPv, Krietemeijer GM, Peluso JP, Boogaarts HD, Lo R, Gerrits D, Dinkelaar W, Appelman APA, Hammer B, Pegge S, Hoorn Avd, Vinke S, Nijeholt GJLà, Boiten J, Vos JA, Schonewille WJ, Hofmeijer J, Martens JM, Worp HBvd, Lo RH, Hofmeijer J, Flach HZ, Ghannouti Ne, Sterrenberg M, Puppels C, Pellikaan W, Sprengers R, Elfrink M, Simons M, Vossers M, Meris Jd, Vermeulen T, Geerlings A, Vemde Gv, Simons T, Rijswijk Cv, Messchendorp G, Nicolaij N, Bongenaar H, Bodde K, Kleijn S, Lodico J, Droste H, Wollaert M, Verheesen S, Jeurrissen D, Bos E, Drabbe Y, Sandiman M, Elfrink M, Aaldering N, Zweedijk B, Khalilzada M, Vervoort J, Droste H, Nicolaij N, Simons M, Ponjee E, Romviel S, Kanselaar K, Bos E, Barning D, Chalos V, Geuskens RR, Straaten Tv, Ergezen S, Harmsma RRM, Muijres D, Jong Ad, Boers AMM, Huguet J, Groot PFC, Mens MA, Kranendonk KRv, Treurniet KM, Tolhuisen ML, Alves H, Weterings AJ, Kirkels ELF, Voogd EJHF, Schupp LM, Collette S, Groot AED, LeCouffe NE, Konduri PR, Prasetya H, Arrarte-Terreros N, Ramos LA. Clinical and imaging determinants of collateral status in patients with acute ischemic stroke in MR CLEAN trial and registry. Stroke. 2020, 51:1493-1502. https://doi.org/10.1161/STROKEAHA.119.027483.
Broderick JP, Palesch YY, Demchuk AM, Yeatts SD, Khatri P, Hill MD, Jauch EC, Jovin TG, Yan B, Silver FL, von Kummer R, Molina CA, Demaerschalk BM, Budzik R, Clark WM, Zaidat OO, Malisch TW, Goyal M, Schonewille WJ, Mazighi M, Engelter ST, Anderson C, Spilker J, Carrozzella J, Ryckborst KJ, Janis LS, Martin RH, Foster LD, Tomsick TA. Endovascular therapy after intravenous t-PA versus t-PA alone for stroke. N Engl J Med. 2013;368:893–903. https://doi.org/10.1056/NEJMoa1214300.
Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, Biller J, Brown M, Demaerschalk BM, Hoh B, Jauch EC, Kidwell CS, Leslie-Mazwi TM, Ovbiagele B, Scott PA, Sheth KN, Southerland AM, Summers DV, Tirschwell DL. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2019;50:e344–418. https://doi.org/10.1161/STR.0000000000000211.
Casaubon LK, Boulanger JM, Blacquiere D, Boucher S, Brown K, Goddard T, Gordon J, Horton M, Lalonde J, LaRivière C, Lavoie P, Leslie P, McNeill J, Menon BK, Moses B, Penn M, Perry J, Snieder E, Tymianski D, Foley N, Smith EE, Gubitz G, Hill MD, Glasser E, Lindsay P. Canadian stroke best practice recommendations: hyperacute stroke care guidelines, update 2015. Int J Stroke Off J Int Stroke Soc. 2015;10:924–40. https://doi.org/10.1111/ijs.12551.
Liu L, Ding J, Leng X, Pu Y, Huang L-A, Xu A, Wong KSL, Wang X, Wang Y. Guidelines for evaluation and management of cerebral collateral circulation in ischaemic stroke 2017. Stroke Vasc Neurol. 2018;3:117–30. https://doi.org/10.1136/svn-2017-000135.
Parthasarathy R, Kate M, Rempel JL, Liebeskind DS, Jeerakathil T, Butcher KS, Shuaib A. Prognostic evaluation based on cortical vein score difference in stroke. Stroke. 2013;44:2748–54. https://doi.org/10.1161/strokeaha.113.001231.
Parthasarathy R, Sohn S-I, Jeerakathil T, Kate MP, Mishra SM, Nambiar VK, Ahmad A, Menon BK, Shuaib A. A combined arterial and venous grading scale to predict outcome in anterior circulation ischemic stroke. J Neuroimaging. 2015;25:969–77. https://doi.org/10.1111/jon.12260.
Markus HS. Cerebral perfusion and stroke. J Neurol Neurosurg Psychiatry. 2004;75:353–61. https://doi.org/10.1136/jnnp.2003.025825.
Vagal A, Aviv R, Sucharew H, Reddy M, Hou Q, Michel P, Jovin T, Tomsick T, Wintermark M, Khatri P. Collateral clock is more important than time clock for tissue fate. Stroke. 2018;49:2102–7. https://doi.org/10.1161/STROKEAHA.118.021484.
Schirmer SH, van Nooijen FC, Piek JJ, van Royen N. Stimulation of collateral artery growth: travelling further down the road to clinical application. Heart (British Cardiac Soc). 2009;95:191–7. https://doi.org/10.1136/hrt.2007.136119.
Fujita K, Tanaka K, Yamagami H, Ide T, Ishiyama H, Sonoda K, Satow T, Takahashi JC, Ihara M, Koga M, Yokota T, Toyoda K. Detrimental effect of chronic hypertension on leptomeningeal collateral flow in acute ischemic stroke. Stroke. 2019;50:1751–7. https://doi.org/10.1161/STROKEAHA.119.025142.
Cipolla MJ, Chan S-L. Impact of acute and chronic hypertension on changes in pial collateral tone in vivo during transient ischemia. Hypertension. 2020;76:1019–26. https://doi.org/10.1161/HYPERTENSIONAHA.120.15356.
Author information
Authors and Affiliations
Contributions
Equal contribution from Patel and Liebeskind.
Corresponding author
Ethics declarations
Ethical Approval and Consent to Participate
Not applicable.
Human and Animal Ethics
Not applicable.
Consent for Publication
Not applicable.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Highlights
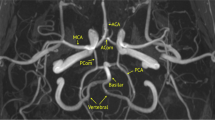
• Anatomy of the brain’s collateral circulation.
• Vascular biology of the brain’s collateral circulation.
• Measurement of collateral flow and the ischemic penumbra.
• Clinical and imaging definitions of collateral status.
• Impact of collateral flow on evolution of the penumbra and penumbral salvage after stroke.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Patel, S.D., Liebeskind, D. Collaterals and Elusive Ischemic Penumbra. Transl. Stroke Res. 14, 3–12 (2023). https://doi.org/10.1007/s12975-022-01116-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12975-022-01116-2