Abstract
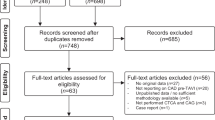
Coronary artery disease (CAD) and severe aortic valve stenosis frequently coexist. Given the progressive nature of CAD, silent or non-significant CAD may become symptomatic or functionally relevant years after TAVR. However, there is a paucity of data documenting the feasibility of either coronary angiography and/or PCI after TAVR. We systematically searched Medline, Pubmed, Embase, Cochrane database, Google Scholar, Science Direct, Web of Science, and conference abstracts from conception to March 2020 using OvidSP in TAVR patients undergoing coronary angiography with or without PCI at least 6 months after TAVR. Patients and procedural characteristics were summarized. The primary outcome of interest was successful coronary angiography for either the left main coronary artery (LMCA) or right coronary artery (RCA) with or without PCI. Pooled estimates were calculated using a random-effects meta-analysis. The study protocol was registered in PROSPERO. Eleven reports for a total of 696 coronary angiograms and 287 PCI were included in the analysis. Patients were slightly predominantly male, older and had a mean left ventricular ejection fraction of more than 50% with an intermediate STS. The summary estimate rates of successful LMCA and RCA angiography with a Medtronic self-expandable valve (SEV) were 84% (95% CI 73–90%, I2 = 79, p = 0.015) and 69% (95% CI 37–89%, I2 = 86, p = 0.23), respectively, while with the Edwards Lifesciences balloon expandable valve (BEV), the summary estimate rates for successful LMCA and RCA angiography were 94% (95% CI 72–99%, I2 = 66, p = 0.003) and 95% (95% CI 48–99%, I2 = 83, p = 0.05), respectively. The summary estimate rate of successful PCI post TAVR with either a Medtronic SEV or Edwards Lifesciences BEV was 93% (95% CI 86–96%, I2 = 33, p = 0.0001). The overall achievement of a successful coronary angiography with or without PCI in post-TAVR patients is high, with a lower success rate for RCA angiography in patients with the Medtronic SEV Mortality and bleeding did not differ in our analysis.





Similar content being viewed by others
References
Mack MJ, Leon MB, Thourani VH, et al. Transcatheter aortic-valve replacement with a balloon-expandable valve in low-risk patients. N Engl J Med. 2019;380(18):1695–705.
Popma J, Deeb M, Yakubov S, et al. Transcatheter aortic-valve replacement with a self-expanding valve in low-risk patients. N Engl J Med. 2019;380(18):1706–15.
Kvidal P, Bergström R, Hörte LG, Ståhle E. Observed and relative survival after aortic valve replacement. J Am CollCardiol. 2000;35(3):747–56.
D’Ascenzo F, Conrotto F, Giordana F, et al. Mid-term prognostic value of coronary artery disease in patients undergoing transcatheter aortic valve implantation: a meta-analysis of adjusted observational results. Int J Cardiol. 2013;168(3):2528–32.
Zivelonghi C, Pesarini G, Scarsini R, Lunardi M, Piccoli A, Ferrero V, Gottin L, Vassanelli C, Ribichini F. Coronary catheterization and percutaneous interventions after transcatheter aortic valve implantation. Am J Cardiol. 2017;120(4):625–31. https://doi.org/10.1016/j.amjcard.2016.10.046.
Neale T. CMS finalizes rule allowing reimbursement of PCI in ambulatory centers. 2019. https://oklahoman.com/article/5654349/medicare-now-covers-outpatient-coronary-procedure.
Allali A, El-Mawardy M, Schwarz B, et al. Incidence, feasibility and outcome of percutaneous coronary intervention after transcatheter aortic valve implantation with a self-expanding prosthesis. Results from a single center experience. CardiovascRevasc Med. 2016;17(6):391–8.
Boukantar M, Gallet R, Mouillet G, et al. Coronary procedures after TAVI with the self-expanding aortic bioprosthesismedtronicCoreValve TM, not an easy matter. J IntervCardiol. 2017;30(1):56–62.
Yudi MB, Sharma SK, Tang GHL, Kini A. Coronary angiography and percutaneous coronary intervention after transcatheter aortic valve replacement. J Am CollCardiol. 2018;71(12):1360–78.
Mother D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535.
van Kesteren F, Wiegerinck E, Rizzo S, et al. Autopsy after transaortic valve implantation. Virchows Arch. 2017;470:331–9.
Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed 3 Mar 2020.
Wallace B, Dahabreh I, Trikalinos T, et al. Closing the gap between methodologists and end users: R as a computational back-end. J Stat Softw. 2012;49:1–15.
Higgins J. Thompson, Simon, Deeks, Jonathan, Altman, Douglas. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–60.
DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177–88.
Blumenstein J, Kim WK, Liebetrau C, et al. Challenges of coronary angiography and intervention in patients previously treated by TAVI. Clin Res Cardiol. 2015;104(8):632–9.
Katsanos S, Debonnaire P, van der Kley F, et al. Position of Edwards SAPIEN transcatheter valve in the aortic root in relation with the coronary ostia: implications for percutaneous coronary interventions. Catheter CardiovascInterv. 2015;85(3):480–7.
Chakravarty T, Sharma R, Abramowitz Y, et al. Outcomes in patients with transcatheter aortic valve replacement and left main stenting: the TAVR-LM registry. J Am CollCardiol. 2016;67(8):951–60.
Chetcuti S, Kleiman NS, Matthews R, Popma J, Moore J. TCT-743 percutaneous coronary intervention after self-expanding transcatheter aortic valve replacement. J Am CollCardiol. 2016;68:B300–1.
Htun WW, Grines C, Schreiber T. Feasibility of coronary angiography and percutaneous coronary intervention after transcatheter aortic valve replacement using a Medtronic™ self-expandable bioprosthetic valve. Catheter Cardiovasc Interv. 2018;91(7):1339–44. https://doi.org/10.1002/ccd.27346.
Ferreira-Neto AN, Puri R, Asmarats L, et al. Clinical and technical characteristics of coronary angiography and percutaneous coronary interventions performed before and after transcatheter aortic valve replacement with a balloon-expandable valve. J IntervCardiol. 2019;2019:3579671.
Vilalta V, Asmarats L, Ferreira-Neto AN, et al. Incidence, clinical characteristics, and impact of acute coronary syndrome following transcatheter aortic valve replacement. JACC Cardiovasc Interv. 2018;11(24):2523–33.
Faroux L, Munoz-Garcia E, et al. Acute coronary syndrome following transcatheter aortic valve replacement. CircCardiovascInterv. 2020;13(2):e008620.
Couture T, Faroux L, Junquera L, et al. Interaction between self-expanding transcatheter heart valves and coronary ostia: an angiographically based analysis of the Evolut R/Pro valve system. J Invasive Cardiol. 2020. Cited in: Ovid MEDLINE(R) Epub Ahead of Print. http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=medp&NEWS=N&AN=32160151. Accessed 31 Mar 2020.
Tanaka A, Jabbour RJ, Testa L, et al. Incidence, technical safety, and feasibility of coronary angiography and intervention following self-expanding transcatheter aortic valve replacement. CardiovascRevasc Med. 2019;20(5):371–5.
Wenaweser P, Pilgrim T, Guerios E, et al. Impact of coronary artery disease and percutaneous coronary intervention on outcomes in patients with severe aortic stenosis undergoing transcatheter aortic valve implantation. EuroIntervention. 2011;7(5):541–8.
Gautier M, Pepin M, Himbert D, et al. Impact of coronary artery disease on indications for transcatheter aortic valve implantation and on procedural outcomes. EuroIntervention. 2011;7(5):549–55.
Griese DP, Reents W, Tóth A, et al. Concomitant coronary intervention is associated with poorer early and late clinical outcomes in selected elderly patients receiving transcatheter aortic valve implantation. Eur J CardiothoracSurg. 2014;46(1):e1–7.
Pasic M, Dreysse S, Unbehaun A, et al. Combined elective percutaneous coronary intervention and transapicaltranscatheter aortic valve implantation. Interact CardiovascThoracSurg. 2012;14(4):463–8.
Kotronias RA, Kwok CS, George S, et al. Transcatheter aortic valve implantation with or without percutaneous coronary artery revascularization strategy: a systematic review and meta-analysis. J Am Heart Assoc. 2017;6(6):1–27.
Harhash A, Ansari J, Mandel L, Kipperman R. STEMI after TAVR: procedural challenge and catastrophic outcome. JACC CardiovascInterv. 2016;9(13):1412–3.
Chodor P, Wilczek K, Przybylski R, Nozynski J, Wloch L, Kalarus Z. Percutaneous access to coronary arteries in patients after transcatheter aortic valve implantation procedures - is it a real problem? PostepyKardiolInterwencyjnej. 2019;15(3):274–82.
Barbanti M, Costa G, Picci A, et al. Coronary cannulation after transcatheter aortic valve replacement: the RE-ACCESS study. JACC CardiovascInterv. 2020;13(21):2542–55.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
There are no financial conflicts to disclose. All authors contributed equally to this manuscript. This study used only aggregate de-identified data and was therefore exempt from additional review board review and previous informed consent, strictly following the Declaration of Helsinki and the NIH guidelines involving human subjects.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Diaz, M.A., Patton, M., Valdes, P. et al. A systematic review and meta-analysis of delayed coronary artery access for coronary angiography with or without percutaneous coronary intervention (PCI) in patients who underwent transcatheter aortic valve replacement (TAVR). Cardiovasc Interv and Ther 37, 167–181 (2022). https://doi.org/10.1007/s12928-020-00753-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12928-020-00753-4