Abstract
Central nervous system (CNS) dysfunction induced by sepsis and pathogenic microbial infections is reported to be closely associated with increased permeability of the blood–brain barrier (BBB), which is mainly mediated by the stimulation of lipopolysaccharide (LPS) on inflammatory signaling. Midazolam is a novel sedative acting on the benzodiazepine receptor, which is recently reported to exert a neuroprotective effect by inhibiting inflammation. The present study will explore the potential repair capacity of Midazolam on LPS-induced damage to the BBB. The in vivo mice model was established by intraperitoneal injection of LPS, while the in vitro model was constructed by stimulating endothelial cells utilizing LPS. We found that the increased malondialdehyde (MDA) level and reduced superoxide dismutase (SOD) activity in the brain cortices, promoted serum concentration of inflammatory factors, and elevated BBB permeability were found in the LPS group, all of which were dramatically reversed by 1 mg/kg and 2 mg/kg Midazolam. Interestingly, Midazolam increased the expression of the tight junction protein zonula occludens-1 (ZO-1). In LPS-challenged in vitro human brain microvascular endothelial cells (HBMECs), the increased concentration of inflammatory factors, reduced trans-endothelial electrical resistance (TEER) level, elevated relative value of trans-endothelial permeability, and downregulated ZO-1 were observed, all of which were pronouncedly alleviated by Midazolam, accompanied by the inhibition on the Ras homolog family member A/ Rho-kinase 2 (RhoA/ROCK-2) pathway. Furthermore, the regulatory effects of Midazolam on ZO-1 expression and the endothelial monolayer permeability in LPS-challenged HBMECs were abolished by the overexpression of RhoA. Collectively, our data imply that Midazolam ameliorated the impairment of the BBB against LPS by regulating the RhoA/ROCK2 pathway.










Similar content being viewed by others
Data Availability Statement/Availability of Data Materials
Data of this study are available upon reasonable request to the corresponding authors.
References
Akira S, Uematsu S, Takeuchi O (2006) Pathogen recognition and innate immunity. Cell 124:783–801
Banks WA (2008) The blood-brain barrier as a cause of disease. Curr Pharm Des 14:1553–1554
Bednarczyk J, Lukasiuk K (2011) Tight junctions in neurological diseases. Acta Neurobiol Exp (Wars) 71:393–408
Begum AN, Jones MR, Lim GP, Morihara T, Kim P, Heath DD et al (2008) Curcumin structure-function, bioavailability, and efficacy in models of neuroinflammation and Alzheimer’s disease. J Pharmacol Exp Ther 326:196–208
Burda JE, Sofroniew MV (2014) Reactive gliosis and the multicellular response to CNS damage and disease. Neuron 81(2):229–248
Csolle C, Sperlagh B (2011) Endocannabinergic modulation of interleukin-1beta in mouse hippocampus under basal conditions and after in vivo systemic lipopolysaccharide stimulation. Neuroimmunomodulation 18:226–231
De Jong PR, González-Navajas JM, Jansen NJG (2016) The digestive tract as the origin of systemic inflammation. Crit Care 20:279
Feng S, Zou L, Wang H, He R, Liu K, Zhu H (2018) RhoA/ROCK-2 pathway inhibition and tight junction protein upregulation by catalpol suppresses lipopolysaccaride-induced disruption of blood-brain barrier permeability. Molecules 23
Haileselassie B, Joshi AU, Minhas PS, Mukherjee R, Andreasson KI, Mochly-Rosen D (2020) Mitochondrial dysfunction mediated through dynamin-related protein 1 (Drp1) propagates impairment in blood brain barrier in septic encephalopathy. J Neuroinflammation 17:36
Haruwaka K, Ikegami A, Tachibana Y, Ohno N, Konishi H, Hashimoto A et al (2019) Dual microglia effects on blood brain barrier permeability induced by systemic inflammation. Nat Commun 10:5816
He F, Yin F, Omran A, Yang LF, Xiang QL, Peng J (2012) PKC and RhoA signals cross-talk in Escherichia coli endotoxin induced alterations in brain endothelial permeability. Biochem Biophys Res Commun 425:182–188
Horiguchi Y, Ohta N, Yamamoto S, Koide M, Fujino Y (2019) Midazolam suppresses the lipopolysaccharide-stimulated immune responses of human macrophages via translocator protein signaling. Int Immunopharmacol 66:373–382
Huang Y, Chen S, Luo Y, Han Z (2020) Crosstalk between inflammation and the BBB in Stroke. Curr Neuropharmacol 18:1227–1236
Illes P (2021) P2X7 Receptors amplify CNS damage in neurodegenerative diseases. Int J Mol Sci 21(17):5996
Kim HS, Kim S, Shin SJ, Park YH et al (2021) Gram-negative bacteria and their lipopolysaccharides in Alzheimer’s disease: pathologic roles and therapeutic implications. Transl Neurodegener 10(1):49
Lu YC, Yeh WC, Ohashi PS (2008) LPS/TLR4 signal transduction pathway. Cytokine 42:145–151
Mansour HM, Fawzy HM, El-Khatib AS, Khattab MM (2022) Repurposed anti-cancer epidermal growth factor receptor inhibitors: mechanisms of neuroprotective effects in Alzheimer’s disease. Neural Regen Res 17(9):1913–1918
Molnar L, Fulesdi B, Nemeth N, Molnar C (2018) Sepsis-associated encephalopathy: a review of literature. Neurol India 66:352–361
Nagyoszi P, Wilhelm I, Farkas AE, Fazakas C, Dung NT, Hasko J et al (2010) Expression and regulation of toll-like receptors in cerebral endothelial cells. Neurochem Int 57:556–564
Olkkola KT, Ahonen J (2008) Midazolam and other benzodiazepines. Handb Exp Pharmacol 335–60
O’Neill LA, Dinarello CA (2000) The IL-1 receptor/toll-like receptor superfamily: crucial receptors for inflammation and host defense. Immunol Today 21:206–209
Park SJ, Jung HJ, Son MS, Jung JM, Kim DH, Jung IH et al (2012) Neuroprotective effects of INM-176 against lipopolysaccharide-induced neuronal injury. Pharmacol Biochem Behav 101:427–433
Peng X, Luo Z, He S, Zhang L, Li Y (2021) Blood-brain barrier disruption by lipopolysaccharide and sepsis-associated encephalopathy. Front Cell Infect Microbiol 11:768108
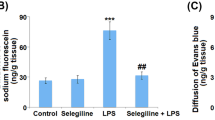
Pu Y, Qian F, Guo J, Sha Y, Qian Y (2022) Selegiline protects against lipopolysaccharide (LPS)-induced impairment of the blood-brain barrier through regulating the NF-κB/MLCK/p-MLC signaling pathway. Neurotox Res 40(1):267–275
Rom S, Dykstra H, Zuluaga-Ramirez V, Reichenbach NL, Persidsky Y (2015) miR-98 and let-7g* protect the blood-brain barrier under neuroinflammatory conditions. J Cereb Blood Flow Metab 35:1957–1965
Tucsek Z, Toth P, Sosnowska D, Gautam T, Mitschelen M, Koller A et al (2014) Obesity in aging exacerbates blood-brain barrier disruption, neuroinflammation, and oxidative stress in the mouse hippocampus: effects on expression of genes involved in beta-amyloid generation and Alzheimer’s disease. J Gerontol A Biol Sci Med Sci 69:1212–1226
Van Itallie CM, Anderson JM (2014) Architecture of tight junctions and principles of molecular composition. Semin Cell Dev Biol 36:157–165
Vutukuri R, Brunkhorst R, Kestner RI, Hansen L, Bouzas NF, Pfeilschifter J et al (2018) Alteration of sphingolipid metabolism as a putative mechanism underlying LPS-induced BBB disruption. J Neurochemistry 144:172–185
Wang YP, Wu Y, Li LY, Zheng J, Liu RG, Zhou JP et al (2011) Aspirin-triggered lipoxin A4 attenuates LPS-induced pro-inflammatory responses by inhibiting activation of NF-kappaB and MAPKs in BV-2 microglial cells. J Neuroinflammation 8:95
Xie J, Shen Z, Anraku Y, Kataoka K, Chen X (2019) Nanomaterial-based blood-brain-barrier (BBB) crossing strategies. Biomaterials 224:119491
Yang C, Hawkins KE, Dore S, Candelario-Jalil E (2019) Neuroinflammatory mechanisms of blood-brain barrier damage in ischemic stroke. Am J Physiol Cell Physiol 316:C135–C153
Yu H, Wang X, Kang F, Chen Z, Meng Y, Dai M (2019) Neuroprotective effects of midazolam on focal cerebral ischemia in rats through antiapoptotic mechanisms. Int J Mol Med 43:443–451
Zhao Z, Hu J, Gao X, Liang H, Liu Z (2014) Activation of AMPK attenuates lipopolysaccharide-impaired integrity and function of blood-brain barrier in human brain microvascular endothelial cells. Exp Mol Pathol 97:386–392
Funding
This study was supported by the “Peking Union Medical College, Chinese Academy of Medical Sciences” and "Nantong Municipal Health Committee (MB2020024)".
Author information
Authors and Affiliations
Contributions
Juyan Zheng and Xuerong Yu contributed to experimental design and data analysis; Juyan Zheng, Wei Zhang, PeiPei Kang, Xiaojiao Zheng, Kai He, and Hong Bai contributed to investigation; Xuerong Yu prepared the manuscript. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Consent to Publication
All the authors have read and approved the final submission of this study.
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zheng, J., Zhang, W., Kang, P. et al. Midazolam Ameliorates Impairment of the Blood–Brain Barrier (BBB) Against LPS. Neurotox Res 40, 751–762 (2022). https://doi.org/10.1007/s12640-022-00508-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12640-022-00508-4