Abstract
Purpose
Total knee arthroplasty (TKA) is associated with severe postoperative pain. Continuous adductor canal blockade provides analgesia while preserving quadriceps muscle strength. Nevertheless, uncertainty still exists as to the optimal adductor canal catheter placement approach. We sought to conduct a systematic review and meta-analysis of randomized controlled trials (RCTs) comparing the analgesic effects of proximal vs distal adductor canal catheters in patients undergoing TKA.
Source
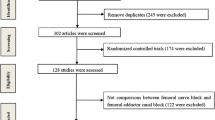
We systematically searched PubMed, EMBASE, and Cochrane for RCTs comparing distal and proximal adductor canal catheters for TKA regarding critical clinical outcomes in adult patients. Statistical analysis was performed using R version 4.1.2 (R Foundation for Statistical Computing, Vienna, Austria). Heterogeneity was assessed using the Cochran Q test and I2 statistics. Trial sequential analysis (TSA) was performed to evaluate the risk of random errors and the uncertainty of our results. The risk of bias was appraised according to the RoB-2 tool.
Principal findings
Six RCTs and 352 patients were included, of whom 151 (42.9%) were male, and 175 (49.7%) were randomized to undergo proximal adductor canal catheter placement. Due to the randomized nature of the studies, baseline characteristics were similar between groups. There were no statistical differences between proximal and distal adductor canal catheters regarding cumulative opioid consumption in the first 24 hr (mean difference [MD], −4.86; 95% confidence interval [CI], −15.19 to 5.47; P = 0.36; four RCTs; 240 patients); pain scores at rest (MD, 0.41; 95% CI, −1.23 to 0.40; P = 0.32; six RCTs; 350 patients); and pain scores with movement for the first 24 hr (MD, −0.25; 95% CI, −0.85 to 0.35; P = 0.42; four RCTs; 246 patients). In the TSA, the required information size was not reached, and the Z-curve did not cross the monitoring boundaries in any of the endpoints.
Conclusion
These findings suggest that proximal vs distal adductor canal catheter placement in patients undergoing TKA may be equally effective for the outcomes of opioid consumption in the first 24 hr, pain scores at rest, and pain scores with movement in the first 24 hr. Nevertheless, TSA findings suggest insufficient power to definitively conclude no differences between the two techniques.
Study registration
PROSPERO (CRD42022353576); registered 25 August 2022.
Résumé
Objectif
L’arthroplastie totale du genou (ATG) est associée à une douleur postopératoire majeure. Le bloc continu du canal adducteur procure une analgésie tout en préservant la force musculaire du quadriceps. Néanmoins, il existe encore des incertitudes quant à l’approche optimale de positionnement du cathéter du canal adducteur. Nous avons cherché à réaliser une revue systématique et une méta-analyse d’études randomisées contrôlées (ERC) comparant les effets analgésiques de cathéters proximaux et distaux du canal adducteur chez la patientèle bénéficiant d’une ATG.
Sources
Nous avons réalisé des recherches systématiques dans les bases de données PubMed, EMBASE et Cochrane pour en tirer les ERC comparant les cathéters distaux et proximaux du canal adducteur pour l’ATG touchant aux critères d’évaluation cliniques critiques chez les patient·es adultes. L’analyse statistique a été réalisée à l’aide de la version R 4.1.2 (R Foundation for Statistical Computing, Vienne, Autriche). L’hétérogénéité a été évaluée à l’aide du test Q de Cochran et des statistiques I2. Une analyse séquentielle des études a été réalisée pour évaluer le risque d’erreurs aléatoires et l’incertitude de nos résultats. Le risque de biais a été évalué selon l’outil RoB-2.
Constatations principales
Six ERC et 352 patient·es ont été inclus·es, dont 151 (42,9 %) hommes, et 175 (49,7 %) ont été randomisé·es pour bénéficier d’une pose proximale d’un cathéter du canal adducteur. En raison de la nature randomisée des études, les caractéristiques initiales étaient similaires entre les groupes. Il n’y avait aucune différence statistique entre les cathéters proximaux et distaux du canal adducteur en ce qui concerne la consommation cumulative d’opioïdes au cours des premières 24 heures (différence moyenne [DM], −4,86; intervalle de confiance [IC] à 95 %, −15,19 à 5,47; P = 0,36; quatre ERC; 240 patient·es); les scores de douleur au repos (DM, −0,41; IC 95 %, −1,23 à 0,40; P = 0,32; six ERC ; 350 patient·es); et les scores de douleur en mouvement pendant les premières 24 heures (DM, −0,25; IC 95 %, −0,85 à 0,35; P = 0,42; quatre ERC; 246 patient·es). Dans l’analyse séquentielle des études, la taille d’information requise n’a pas été atteinte et la courbe en Z n’a franchi les limites de surveillance dans aucun des paramètres.
Conclusion
Ces résultats suggèrent que le positionnement proximal ou distal d’un cathéter du canal adducteur chez les personnes subissant une ATG peut être tout aussi efficace en ce qui touche aux critères de consommation d’opioïdes au cours des premières 24 heures, de scores de douleur au repos et de scores de douleur en mouvement au cours des premières 24 heures. Néanmoins, les résultats de l’analyse séquentielle suggèrent une puissance insuffisante pour conclure de manière définitive à l’absence de différences entre les deux techniques.
Enregistrement de l’étude
PROSPERO (CRD42022353576); enregistrée le 25 août 2022.





Similar content being viewed by others
References
Terkawi AS, Mavridis D, Sessler DI, et al. Pain management modalities after total knee arthroplasty: a network meta-analysis of 170 randomized controlled trials. Anesthesiology 2017; 126: 923–37. https://doi.org/10.1097/aln.0000000000001607
Jenstrup MT, Jæger P, Lund J, et al. Effects of adductor-canal-blockade on pain and ambulation after total knee arthroplasty: a randomized study. Acta Anaesthesiol Scand 2012; 56: 357–64. https://doi.org/10.1111/j.1399-6576.2011.02621.x
Macrinici GI, Murphy C, Christman L, et al. Prospective, double-blind, randomized study to evaluate single-injection adductor canal nerve block versus femoral nerve block: postoperative functional outcomes after total knee arthroplasty. Reg Anesth Pain Med 2017; 42: 10–6. https://doi.org/10.1097/aap.0000000000000507
Wang D, Yang Y, Li Q, et al. Adductor canal block versus femoral nerve block for total knee arthroplasty: a meta-analysis of randomized controlled trials. Sci Rep 2017; 7: 40721. https://doi.org/10.1038/srep40721
Mariano ER, Kim TE, Wagner MJ, et al. A randomized comparison of proximal and distal ultrasound-guided adductor canal catheter insertion sites for knee arthroplasty. J Ultrasound Med 2014; 33: 1653–62. https://doi.org/10.7863/ultra.33.9.1653
Yu R, Wang H, Zhuo Y, Liu D, Wu C, Zhang Y. Continuous adductor canal block provides better performance after total knee arthroplasty compared with the single-shot adductor canal block?: an updated meta-analysis of randomized controlled trials. Medicine (Baltimore) 2020; 99: e22762. https://doi.org/10.1097/md.0000000000022762
Tran J, Chan VW, Peng PW, Agur AM. Evaluation of the proximal adductor canal block injectate spread: a cadaveric study. Reg Anesth Pain Med 2019; 45: 124–30. https://doi.org/10.1136/rapm-2019-101091
Abdallah FW, Mejia J, Prasad GA, et al. Opioid- and motor-sparing with proximal, mid-, and distal locations for adductor canal block in anterior cruciate ligament reconstruction: a randomized clinical trial. Anesthesiology 2019; 131: 619–29. https://doi.org/10.1097/aln.0000000000002817
Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021; 372: n71. https://doi.org/10.1136/bmj.n71
Sterne JA, Savović J, Page MJ, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 2019; 366: I4898. https://doi.org/10.1136/bmj.l4898
Schünemann H, Brożek J, Guyatt G, Oxman A. GRADE handbook: handbook for grading the quality of evidence and strength of recommendations using the GRADE approach, 2013. Available from URL: https://gdt.gradepro.org/app/handbook/handbook.html (accessed March 2023).
GRADEpro. Homepage. Available from URL: https://www.gradepro.org/ (accessed March 2023).
Danoff JR, Goel R, Sutton R, Maltenfort MG, Austin MS. How much pain is significant? Defining the minimal clinically important difference for the visual analog scale for pain after total joint arthroplasty. J Arthroplasty 2018; 33: S71–5. https://doi.org/10.1016/j.arth.2018.02.029
ClinCalc LLC. Equivalent opioid calculator. Available from URL: https://clincalc.com/Opioids/ (accessed March 2023).
Laigaard J, Pedersen C, Rønsbo TN, Mathiesen O, Karlsen AP. Minimal clinically important differences in randomised clinical trials on pain management after total hip and knee arthroplasty: a systematic review. Br J Anaesth 2021; 126: 1029–37. https://doi.org/10.1016/j.bja.2021.01.021
Shah A, Smith AF. Trial sequential analysis: adding a new dimension to meta-analysis. Anaesthesia 2020; 75: 15–20. https://doi.org/10.1111/anae.14705
Sztain JF, Khatibi B, Monahan AM, et al. Proximal versus distal continuous adductor canal blocks: does varying perineural catheter location influence analgesia? A randomized, subject-masked, controlled clinical trial. Anesth Analg 2018; 127: 240–6. https://doi.org/10.1213/ane.0000000000003422
Lee B, Park SJ, Park KK, Kim HJ, Lee YS, Choi YS. Optimal location for continuous catheter analgesia among the femoral triangle, proximal, or distal adductor canal after total knee arthroplasty: a randomized double-blind controlled trial. Reg Anesth Pain Med 2022; 47: 353–8. https://doi.org/10.1136/rapm-2021-103284
Zhang LK, Chen C, Du WB, Zhou HT, Quan RF, Liu JS. Is the proximal adductor canal block a better choice than the distal adductor canal block for primary total knee arthroplasty?: a meta-analysis of randomized controlled trials. Medicine (Baltimore) 2020; 99: e22667. https://doi.org/10.1097/md.0000000000022667
Shoja MM. Chapter 80: Pelvic girdle, gluteal region and thigh. In: Standring S. (Ed.). Gray’s Anatomy: The Anatomical Basis of Clinical Practice, 41st ed. London: Elsevier; 2016: 1337–75.
Meier AW, Auyong DB, Yuan SC, Lin SE, Flaherty JM, Hanson NA. Comparison of continuous proximal versus distal adductor canal blocks for total knee arthroplasty: a randomized, double-blind, noninferiority trial. Reg Anesth Pain Med 2018; 43: 36–42. https://doi.org/10.1097/aap.0000000000000692
Romano C, Lloyd A, Nair S, et al. A randomized comparison of pain control and functional mobility between proximal and distal adductor canal blocks for total knee replacement. Anesth Essays Res 2018; 12: 452–8. https://doi.org/10.4103/aer.aer_17_18
Fei Y, Cui X, Chen S, et al. Continuous block at the proximal end of the adductor canal provides better analgesia compared to that at the middle of the canal after total knee arthroplasty: a randomized, double-blind, controlled trial. BMC Anesthesiol 2020; 20: 260. https://doi.org/10.1186/s12871-020-01165-w
Muñoz-Leyva F, El-Boghdadly K, Chan V. Is the minimal clinically important difference (MCID) in acute pain a good measure of analgesic efficacy in regional anesthesia? Reg Anesth Pain Med 2020; 45: 1000–5. https://doi.org/10.1136/rapm-2020-101670
Gasbjerg KS, Hägi-Pedersen D, Lunn TH, et al. DEX-2-TKA-DEXamethasone twice for pain treatment after total knee arthroplasty: a protocol for a randomized, blinded, three-group multicentre clinical trial. Acta Anaesthesiol Scand 2020; 64: 267–75. https://doi.org/10.1111/aas.13481
Thybo KH, Hägi-Pedersen D, Dahl JB, et al. Effect of combination of paracetamol (acetaminophen) and ibuprofen vs either alone on patient-controlled morphine consumption in the first 24 hours after total hip arthroplasty: the PANSAID randomized clinical trial. JAMA 2019; 321: 562–71. https://doi.org/10.1001/jama.2018.22039
Hickman SR, Mathieson KM, Bradford LM, Garman CD, Gregg RW, Lukens DW. Randomized trial of oral versus intravenous acetaminophen for postoperative pain control. Am J Health Syst Pharm 2018; 75: 367–75. https://doi.org/10.2146/ajhp170064
Bakshi SG, Rathod A, Salunkhe S. Influence of interpretation of pain scores on patients’ perception of pain: a prospective study. Indian J Anaesth 2021; 65: 216–20. https://doi.org/10.4103/ija.ija_130_21
Kumar P, Tripathi L. Challenges in pain assessment: pain intensity scales. Indian J Pain 2014; 28: 61–70. https://doi.org/10.4103/0970-5333.132841
Todd KH. Pain assessment and ethnicity. Ann Emerg Med 1996; 27: 421–3. https://doi.org/10.1016/s0196-0644(96)70221-4
Luo D, Wan X, Liu J, Tong T. Optimally estimating the sample mean from the sample size, median, mid-range, and/or mid-quartile range. Stat Methods Med Res 2018; 27: 1785–805. https://doi.org/10.1177/0962280216669183
Wan X, Wang W, Liu J, Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol 2014; 14: 135. https://doi.org/10.1186/1471-2288-14-135
Marian AA, Ranganath Y, Bayman EO, Senasu J, Brennan TJ. A comparison of 2 ultrasound-guided approaches to the saphenous nerve block: adductor canal versus distal transsartorial: a prospective, randomized, blinded, noninferiority trial. Reg Anesth Pain Med 2015; 40: 623–30. https://doi.org/10.1097/aap.0000000000000277
McGrath S, Zhao X, Steele R, Thombs BD, Benedetti A, DEPRESsion Screening Data (DEPRESSD) Collaboration. Estimating the sample mean and standard deviation from commonly reported quantiles in meta-analysis. Stat Methods Med Res 2020; 29: 2520–37. https://doi.org/10.1177/0962280219889080
Thiayagarajan MK, Kumar SV, Venkatesh S. An exact localization of adductor canal and its clinical significance: a cadaveric study. Anesth Essays Res 2019; 13: 284–6. https://doi.org/10.4103/aer.aer_35_19
Wong WY, Bjørn S, Strid JM, Børglum J, Bendtsen TF. Defining the location of the adductor canal using ultrasound. Reg Anesth Pain Med 2017; 42: 241–5. https://doi.org/10.1097/aap.0000000000000539
Breen TW, Shapiro T, Glass B, Foster-Payne D, Oriol NE. Epidural anesthesia for labor in an ambulatory patient. Anesth Analg 1993; 77: 919–24. https://doi.org/10.1213/00000539-199311000-00008
Craig D, Carli F. Bromage motor blockade score - a score that has lasted more than a lifetime. Can J Anesth 2018; 65: 837–8. https://doi.org/10.1007/s12630-018-1101-7
Author contributions
All authors contributed to the study conception and design. Rafael Lombardi, Isabela Marques, Pedro E. P. Carvalho, Gabriela R. Brandão, Jasmeen Kaur, and Ashish Sakharpe performed material preparation, data collection, and analysis. Rafael Lombardi, Isabela Marques, Pedro E. P. Carvalho, Gabriela R. Brandão, Jasmeen Kaur, and Ashish Sakharpe wrote the first draft of the manuscript. All authors critically reviewed previous versions of the manuscript. All authors agree to be accountable for all aspects of the work.
Acknowledgements
The authors would like to thank Dr. Rhanderson Cardoso, MD, for his review of the manuscript.
Disclosures
The authors have no relevant financial or nonfinancial interests to disclose.
Funding statement
The authors did not receive support from any organization for the submitted work.
Prior conference presentations
Presented at the American Academy of Pain Medicine 2023 meeting (23–26 March 2023, Fort Lauderdale, FL, USA).
Data availability
Because this meta-analysis was based on data extracted from previously published research, all the data and study materials are available in the public domain. The authors of this meta-analysis do not have access to patient-level data of the individual studies. Researchers interested in individual-level data from the studies included in this meta-analysis are encouraged to contact the corresponding author from each study for such requests.
Editorial responsibility
This submission was handled by Dr. Vishal Uppal, Associate Editor, Canadian Journal of Anesthesia/Journal canadien d’anesthésie.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lombardi, R.A., Marques, I.R., Carvalho, P.E.P. et al. Proximal versus distal adductor canal catheters for total knee arthroplasty: a systematic review and meta-analysis of randomized controlled trials. Can J Anesth/J Can Anesth (2023). https://doi.org/10.1007/s12630-023-02552-w
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12630-023-02552-w