Abstract
Purpose
Postoperative pulmonary complications (PPCs) are a common cause of morbidity. Postoperative atelectasis is thought to be a significant risk factor in their development. Recent imaging studies suggest that patients’ extubation may result in similar postoperative atelectasis regardless of the intraoperative mechanical ventilation strategy used. In this pilot trial, we hypothesized that a study investigating the effects of an open lung extubation strategy compared with a conventional one on PPCs would be feasible.
Methods
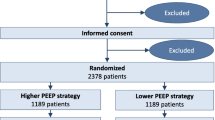
We conducted a pilot, single-centre, double-blinded randomized controlled trial. Adult patients at moderate to high risk of PPCs and scheduled for elective surgery were eligible. Patients were randomized to an open lung extubation strategy (semirecumbent position, fraction of inspired oxygen [FIO2] 50%, pressure support ventilation, unchanged positive end-expiratory pressure) or to a conventional extubation strategy (dorsal decubitus position, FIO2 100%, manual bag ventilation). The primary feasibility outcome was global protocol adherence while the primary exploratory efficacy outcome was PPCs.
Results
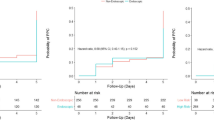
We randomized 35 patients to the conventional extubation group and 34 to the open lung extubation group. We observed a global protocol adherence of 96% (95% confidence interval, 88 to 99), which was not different between groups. Eight PPCs occurred (two in the conventional extubation group vs six in the open lung extubation group). Less postoperative supplemental oxygen and better lung aeration were observed in the open lung extubation group.
Conclusions
In this single-centre pilot trial, we observed excellent feasibility. A multicentre pilot trial comparing the effect of an open lung extubation strategy with that of a conventional extubation strategy on the occurrence of PPCs is feasible.
Study registration date
ClinicalTrials.gov (NCT04993001); registered 6 August 2021.
Résumé
Objectif
Les complications pulmonaires postopératoires (CPP) sont une cause fréquente de morbidité. L’atélectasie postopératoire est considérée comme un facteur de risque important de CPP. Des études d’imagerie récentes suggèrent que l’extubation des patient·es peut entraîner une atélectasie postopératoire semblable, quelle que soit la stratégie de ventilation mécanique peropératoire utilisée. Dans cet essai pilote, nous avons émis l’hypothèse qu’une étude examinant les effets sur les CPP d’une stratégie d’extubation à poumon ouvert par rapport à une stratégie d’extubation conventionnelle serait réalisable.
Méthode
Nous avons mené une étude randomisée contrôlée pilote, monocentrique et à double insu. Les patient·es adultes présentant un risque modéré à élevé de CPP et devant bénéficier d’une chirurgie non urgente étaient éligibles. Les patient·es ont été randomisé·es à une prise en charge par une stratégie d’extubation à poumon ouvert (position semi-couchée, fraction d’oxygène inspiré [FIO2] 50 %, ventilation par aide inspiratoire, pression positive télé-expiratoire inchangée) ou à une stratégie d’extubation conventionnelle (décubitus dorsal, FIO2 100 %, ventilation manuelle par masque). Le principal critère de faisabilité était l’adhésion au protocole global, tandis que les CPP constituaient le principal critère d’efficacité exploratoire.
Résultats
Nous avons randomisé 35 patient·es dans le groupe d’extubation conventionnelle et 34 dans le groupe d’extubation à poumon ouvert. Nous avons observé une adhésion globale au protocole de 96 % (intervalle de confiance à 95 %, 88 à 99), qui n’était pas différente entre les groupes. Huit CPP sont survenues (deux dans le groupe d’extubation conventionnelle vs six dans le groupe d’extubation à poumon ouvert). Nous avons observé des besoins moins importants en oxygène supplémentaire postopératoire et une meilleure aération pulmonaire dans le groupe extubé à poumon ouvert.
Conclusion
Dans cet essai pilote monocentrique, nous avons observé une excellente faisabilité. Une étude pilote multicentrique comparant l’effet d’une stratégie d’extubation à poumon ouvert à celui d’une stratégie d’extubation conventionnelle sur la survenue de CPP est réalisable.
Date d’enregistrement de l’étude
ClinicalTrials.gov (NCT04993001); enregistrée le 6 août 2021.


Similar content being viewed by others
References
Holmer H, Bekele A, Hagander L, et al. Evaluating the collection, comparability and findings of six global surgery indicators. Br J Surg 2019; 106: e138–50. https://doi.org/10.1002/bjs.11061
PROVE Network Investigators for the Clinical Trial Network of the European Society of Anaesthesiology, Hemmes SN, de Abreu MG, Pelosi P, Schultz MJ. High versus low positive end-expiratory pressure during general anaesthesia for open abdominal surgery (PROVHILO trial): a multicentre randomised controlled trial. Lancet 2014; 384: 495–503. https://doi.org/10.1016/s0140-6736(14)60416-5
LAS VEGAS Investigators. Epidemiology, practice of ventilation and outcome for patients at increased risk of postoperative pulmonary complications: LAS VEGAS – an observational study in 29 countries. Eur J Anaesthesiol 2017; 34: 492–507. https://doi.org/10.1097/eja.0000000000000646
Fernandez-Bustamante A, Frendl G, Sprung J, et al. Postoperative pulmonary complications, early mortality, and hospital stay following noncardiothoracic surgery. JAMA Surg 2017; 152: 157–10. https://doi.org/10.1001/jamasurg.2016.4065
Young CC, Harris EM, Vacchiano C, et al. Lung-protective ventilation for the surgical patient: international expert panel-based consensus recommendations. Br J Anaesth 2019; 123: 898–913. https://doi.org/10.1016/j.bja.2019.08.017
Lagier D, Zeng C, Fernandez-Bustamante A, Melo MF. Perioperative pulmonary atelectasis: part II. Clinical implications. Anesthesiology 2022; 136: 206–36. https://doi.org/10.1097/aln.0000000000004009
Futier E, Constantin JM, Paugam-Burtz C, et al. A trial of intraoperative low-tidal-volume ventilation in abdominal surgery. N Engl J Med 2013; 369: 428–37. https://doi.org/10.1056/nejmoa1301082
Ferrando C, Soro M, Unzueta C, et al. Individualised perioperative open-lung approach versus standard protective ventilation in abdominal surgery (iPROVE): a randomised controlled trial. Lancet Respir Med 2018; 6: 193–203. https://doi.org/10.1016/s2213-2600(18)30024-9
Writing Committee for the PROBESE Collaborative Group of the PROtective Ventilation Network (PROVEnet) for the Clinical Trial Network of the European Society of Anaesthesiology, Bluth T, Neto AS, et al. Effect of intraoperative high positive end-expiratory pressure (PEEP) with recruitment maneuvers vs low PEEP on postoperative pulmonary complications in obese patients: a randomized clinical trial. JAMA 2019; 321: 2292–305. https://doi.org/10.1001/jama.2019.7505
Güldner A, Kiss T, Neto AS, et al. Intraoperative protective mechanical ventilation for prevention of postoperative pulmonary complications: a comprehensive review of the role of tidal volume, positive end-expiratory pressure, and lung recruitment maneuvers. Anesthesiology 2015; 123: 692–713. https://doi.org/10.1097/aln.0000000000000754
Kostic P, LoMauro A, Larsson A, Hedenstierna G, Frykholm P, Aliverti A. Specific anesthesia-induced lung volume changes from induction to emergence: a pilot study. Acta Anaesthesiol Scand 2018; 62: 282–92. https://doi.org/10.1111/aas.13026
Généreux V, Chassé M, Girard F, Girard F, Massicotte N, Chartrand-Lefebvre C, Girard M. Effects of positive end-expiratory pressure/recruitment manoeuvres compared with zero end-expiratory pressure on atelectasis during open gynaecological surgery as assessed by ultrasonography: a randomised controlled trial. Br J Anaesth 2020; 124: 101–9. https://doi.org/10.1016/j.bja.2019.09.040
Nestler C, Simon P, Petroff D, et al. Individualized positive end-expiratory pressure in obese patients during general anaesthesia: a randomized controlled clinical trial using electrical impedance tomography. Br J Anaesth 2017; 119: 1194–205. https://doi.org/10.1093/bja/aex192
Bolther M, Henriksen J, Holmberg MJ, et al. ventilation strategies during general anesthesia for noncardiac surgery: a systematic review and meta-analysis. Anesth Analg 2022; 135: 971–85. https://doi.org/10.1213/ane.0000000000006106
Pereira SM, Tucci MR, Morais CC, et al. Individual positive end-expiratory pressure settings optimize intraoperative mechanical ventilation and reduce postoperative atelectasis. Anesthesiology 2018; 129: 1070–81. https://doi.org/10.1097/aln.0000000000002435
Musch G, Melo MF. Intraoperative protective mechanical ventilation: fact or fiction? Anesthesiology 2022; 137: 381–3. https://doi.org/10.1097/aln.0000000000004366
Jeong H, Tanatporn P, Ahn HJ, et al. Pressure support versus spontaneous ventilation during anesthetic emergence—effect on postoperative atelectasis: a randomized controlled trial. Anesthesiology 2021; 135: 1004–14. https://doi.org/10.1097/aln.0000000000003997
Benoît Z, Wicky S, Fischer JF, et al. The effect of increased FiO2 before tracheal extubation on postoperative atelectasis. Anesth Analg 2002; 95: 1777–81. https://doi.org/10.1097/00000539-200212000-00058
Boyce JR, Ness T, Castroman P, Gleysteen JJ. A preliminary study of the optimal anesthesia positioning for the morbidly obese patient. Obes Surg 2003; 13: 4–9. https://doi.org/10.1381/096089203321136511
Östberg E, Thorisson A, Enlund M, Zetterström H, Hedenstierna G, Edmark L. Positive end-expiratory pressure and postoperative atelectasis: a randomized controlled trial. Anesthesiology 2019; 131: 809–17. https://doi.org/10.1097/aln.0000000000002764
Kleinsasser AT, Pircher I, Truebsbach S, Knotzer H, Loeckinger A, Treml B. Pulmonary function after emergence on 100%; oxygen in patients with chronic obstructive pulmonary disease. Anesthesiology 2014; 120: 1146–51. https://doi.org/10.1097/aln.0000000000000161
Lumb AB, Greenhill SJ, Simpson MP, Stewart J. Lung recruitment and positive airway pressure before extubation does not improve oxygenation in the post-anaesthesia care unit: a randomized clinical trial. Br J Anaesth 2010; 104: 643–7. https://doi.org/10.1093/bja/aeq080
Rostin P, Teja BJ, Friedrich S, et al. The association of early postoperative desaturation in the operating theatre with hospital discharge to a skilled nursing or long‐term care facility. Anaesthesia 2019; 74: 457–67. https://doi.org/10.1111/anae.14517
Eldridge SM, Chan CL, Campbell MJ, et al. CONSORT 2010 statement: extension to randomised pilot and feasibility trials. BMJ 2016; 355: i5239. https://doi.org/10.1136/bmj.i5239
Canet J, Gallart L, Gomar C, et al. Prediction of postoperative pulmonary complications in a population-based surgical cohort. Anesthesiology 2010; 113: 1338–50. https://doi.org/10.1097/aln.0b013e3181fc6e0a
Harris PA, Taylor R, Minor BL, et al. The REDCap consortium: building an international community of software platform partners. J Biomed Inform 2019; 95: 103208. https://doi.org/10.1016/j.jbi.2019.103208
Abbott TE, Fowler AJ, Pelosi P, et al. A systematic review and consensus definitions for standardised end-points in perioperative medicine: pulmonary complications. Br J Anaesth 2018; 120: 1066–79. https://doi.org/10.1016/j.bja.2018.02.007
Mongodi S, Bouhemad B, Orlando A, et al. modified lung ultrasound score for assessing and monitoring pulmonary aeration. Ultraschall Med 2017; 38: 530–7. https://doi.org/10.1055/s-0042-120260
Andrea C, Irene S, Emanuele P, et al. Clinical performance of lung ultrasound in predicting time-dependent changes in lung aeration in ARDS patients. J Clin Monitor Comp 2022; https://doi.org/10.1007/s10877-022-00902-5
Zaouter C, Moore A, Carrier FM, Girard J, Girard M. Pressure support ventilation and atelectasis: comment. Anesthesiology 2022; 136: 1043–4. https://doi.org/10.1097/aln.0000000000004193
Zoremba M, Kalmus G, Dette F,Kuhn C, Wulf H. Effect of intra‐operative pressure support vs pressure controlled ventilation on oxygenation and lung function in moderately obese adults. Anaesthesia 2010; 65: 124–9. https://doi.org/10.1111/j.1365-2044.2009.06187.x
Zaouter C, Damphousse R, Moore A, Stevens LM, Gauthier A, Carrier FM. Elements not graded in the Cardiac Enhanced Recovery After Surgery guidelines might improve postoperative outcome: a comprehensive narrative review. J Cardiothorac Vasc Anesth 2022; 36: 746–65. https://doi.org/10.1053/j.jvca.2021.01.035
Pang QY, Mo J, An R, Liu HL. Meta-analysis of the optimal ventilation strategies to improve perioperative oxygenation in obese patients. Int J Clin Exp Med 2017; 10: 5883–91
Ioannidis JP. Why most discovered true associations are inflated. Epidemiology 2008; 19: 640–8. https://doi.org/10.1097/ede.0b013e31818131e7
Bouhemad B, Liu ZH, Arbelot C, et al. Ultrasound assessment of antibiotic-induced pulmonary reaeration in ventilator-associated pneumonia. Crit Care Med 2010; 38: 84–92. https://doi.org/10.1097/ccm.0b013e3181b08cdb
Author contributions
Julie Girard contributed to data collection and revising the final draft of the paper. Cédrick Zaouter and Alex Moore contributed to study design, data collection, and revising the final draft of the paper. François M. Carrier contributed to study design, data analysis, and revising the final draft of the paper. Martin Girard contributed to study design, data collection, data analysis, writing the first draft of the paper, and revising the final draft of the paper.
Acknowledgements
The authors thank Monique Ruel, RN, Julie Desroches, PhD, and Vicky Thiffault, RN, for their valuable assistance and dedication.
Disclosures
Martin Girard is a paid consultant for the point-of-care ultrasonography group of GE Healthcare. The other authors declare no competing interests.
Funding statement
This study was supported by a 2021 research operating grant from the Fonds de développement du Département d’anesthésiologie et de médecine de la douleur de l’Université de Montréal. Dr. Carrier is a recipient of a Career Award from the Fonds de la Recherche du Québec – Santé.
Prior conference presentations
Preliminary results of this study were presented at the Société Française d’Anesthésie et de Réanimation’s annual congress in September 2022 (Paris, France).
Editorial responsibility
This submission was handled by Dr. Philip M. Jones, Deputy Editor-in-Chief, Canadian Journal of Anesthesia/Journal canadien d’anesthésie.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Girard, J., Zaouter, C., Moore, A. et al. Effects of an open lung extubation strategy compared with a conventional extubation strategy on postoperative pulmonary complications after general anesthesia: a single-centre pilot randomized controlled trial. Can J Anesth/J Can Anesth 70, 1648–1659 (2023). https://doi.org/10.1007/s12630-023-02533-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-023-02533-z