Abstract
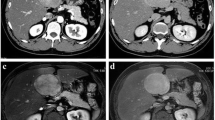
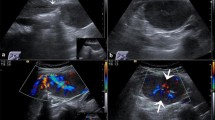
Focal nodular hyperplasia (FNH) is a benign nodular lesion, but because of its feature of portal tract vessel abnormality, it may induce portal hypertension. A 27-year-old woman was admitted with a fever. A large nodule with satellite lesions was found in the liver and cotton wool-like feature of arteries were detected on angiography. Technetium galactosyl serum albumin scintigraphy and diagnostic laparoscopy showed that the tumor site was functional, while the surrounding area was a non-functional fibrotic area. A biopsy specimen indicated that the nodular lesion was an FNH-like lesion. She experienced several instances of variceal rupture and suffered liver failure, receiving liver transplantation. The excised liver showed a centrally scarred area in the nodule, indicating that the diagnosis was FNH. We herein report this case as a rare case of FNH that progressed to liver failure.



Similar content being viewed by others
References
Libbrecht L, Cassiman D, Verslype C, et al. Clinicopathological features of focal nodular hyperplasia-like nodules in 130 cirrhotic explant livers. Am J Gastroenterol. 2006;101:2341–6.
Bioulac-Sage P, Rebouissou S, Thomas C, et al. Hepatocellular adenoma subtype classification using molecular markers and immunohistochemistry. Hepatology. 2007;46:740–8.
Margolskee E, Bao F, de Gonzalez AK, et al. Hepatocellular adenoma classification: a comparative evaluation of immunohistochemistry and targeted mutational analysis. Diagn Pathol. 2016;11:016–0475.
Chuma M, Sakamoto M, Yamazaki K, et al. Expression profiling in multistage hepatocarcinogenesis: identification of HSP70 as a molecular marker of early hepatocellular carcinoma. Hepatology. 2003;37:198–207.
Libbrecht L, Severi T, Cassiman D, et al. Glypican-3 expression distinguishes small hepatocellular carcinomas from cirrhosis, dysplastic nodules, and focal nodular hyperplasia-like nodules. Am J Surg Pathol. 2006;30:1405–11.
Nguyen TB, Roncalli M, Di Tommaso L, et al. Combined use of heat-shock protein 70 and glutamine synthetase is useful in the distinction of typical hepatocellular adenoma from atypical hepatocellular neoplasms and well-differentiated hepatocellular carcinoma. Mod Pathol. 2016;29:283–92.
Narita M, Hatano E, Arizono S, et al. Expression of OATP1B3 determines uptake of Gd-EOB-DTPA in hepatocellular carcinoma. J Gastroenterol. 2009;44:793–8.
Scheuer PJ. Classification of chronic viral hepatitis: a need for reassessment. J Hepatol. 1991;13:372–4.
Sherlock S, Feldman CA, Moran B, et al. Partial nodular transformation of the liver with portal hypertension. Am J Med. 1966;40:195–203.
Guido M, Alves VAF, Balabaud C, et al. Histology of portal vascular changes associated with idiopathic non-cirrhotic portal hypertension: nomenclature and definition. Histopathology. 2019;74:219–26.
Giannitrapani L, Soresi M, La Spada E, et al. Sex hormones and risk of liver tumor. Ann N Y Acad Sci. 2006;1089:228–36.
Maillette de Buy Wenniger L, Terpstra V, Beuers U. Focal nodular hyperplasia and hepatic adenoma: epidemiology and pathology. Dig Surg. 2010;27:24–31.
Nault JC, Paradis V, Cherqui D, et al. Molecular classification of hepatocellular adenoma in clinical practice. J Hepatol. 2017;67:1074–83.
Takahashi S, Miyanishi K, Takada K, et al. Case report of a focal nodular hyperplasia-like nodule present in cirrhotic liver. Hepatol Res. 2008;38:521–8.
Kondo F. Focal nodular hyperplasia-like lesions in heavy drinkers. Intern Med. 2009;48(13):1117–23 (Epub 2009 Jul 1.; 2009).
Kondo F. Benign nodular hepatocellular lesions caused by abnormal hepatic circulation: etiological analysis and introduction of a new concept. J Gastroenterol Hepatol. 2001;16:1319–28.
Okudaira S. Clinicopathologic study on 23 resected cases of focal nodular hyperplasia. Kanzo. 1993;34:621–9.
Wanless IR, Albrecht S, Bilbao J, et al. Multiple focal nodular hyperplasia of the liver associated with vascular malformations of various organs and neoplasia of the brain: a new syndrome. Mod Pathol. 1989;2:456–62.
Rebouissou S, Bioulac-Sage P, Zucman-Rossi J. Molecular pathogenesis of focal nodular hyperplasia and hepatocellular adenoma. J Hepatol. 2008;48:163–70.
Kondo F, Koshima Y, Ebara M. Nodular lesions associated with abnormal liver circulation. Intervirology. 2004;47:277–87.
Nakanuma Y, Hoso M, Sasaki M, et al. Histopathology of the liver in non-cirrhotic portal hypertension of unknown aetiology. Histopathology. 1996;28:195–204.
De Gottardi A, Rautou PE, Schouten J, et al. Porto-sinusoidal vascular disease: proposal and description of a novel entity. Lancet Gastroenterol Hepatol. 2019;4:399–411.
Kang JH, Kim DH, Kim SY, et al. Porto-sinusoidal vascular disease with portal hypertension versus liver cirrhosis: differences in imaging features on CT and hepatobiliary contrast-enhanced MRI. Abdom Radiol (NY). 2020. https://doi.org/10.1007/s00261-020-02831-w.
Glatard AS, Hillaire S, d’Assignies G, et al. Obliterative portal venopathy: findings at CT imaging. Radiology. 2012;263:741–50.
Merli L, Grimaldi C, Monti L, et al. Liver transplantation for refractory severe pruritus related to widespread multifocal hepatic focal nodular hyperplasia (FNH) in a child: case report and review of literature. Pediatr Transplant. 2012;16:E265–8.
Author information
Authors and Affiliations
Contributions
TY participated in the actual diagnosis and treatment of the case, data analysis, and writing of the paper; YT participated in the writing of the paper; AT participated in the actual diagnosis and treatment of the case, data analysis, and writing of the paper; FK and KK participated in the pathological diagnosis; TY participated in the liver transplantation and post-transplantation care for the case; AO, TA, NW, HO, and HS participated in the actual diagnosis and treatment of the case; HO participated in the actual writing of the paper
Corresponding author
Ethics declarations
Conflict of interest
Tetsuya Yasunaka, Yasuto Takeuchi, Akinobu Takaki, Fukuo Kondo, Tomoharu Yoshizumi, Kenichi Kohashi, Atsushi Oyama, Takuya Adachi, Nozomu Wada, Hideki Onishi, Hidenori Shiraha and Hiroyuki Okada declare that they have no conflict of interest.
Human/animal rights
All procedures followed have been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Informed consent
We could not earn informed consent from the patient because she cannot be traced now. This case report does not contain identifying information of the patient.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yasunaka, T., Takeuchi, Y., Takaki, A. et al. A case of focal nodular hyperplasia with hepatic failure treated with liver transplantation. Clin J Gastroenterol 15, 171–176 (2022). https://doi.org/10.1007/s12328-021-01529-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12328-021-01529-w