Abstract
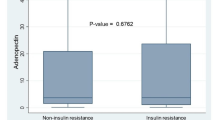
Ovarian cancer has been emerged as a most common and lethal gynecological malignancy in India. High serum insulin and low adiponectin have been associated with increased risk of ovarian cancer. But their role in development of ovarian cancer is conflicting and little evidence is available. We aimed to evaluate blood levels of insulin and adiponectin in epithelial ovarian cancer (EOC) patients and their association with the risk to develop EOC. The study included following three groups; Group 1: fifty cases of cytohistopathologically confirmed cases of EOC, Group 2: fifty age matched cases of benign ovarian conditions and Group 3: fifty ages matched healthy controls with no evidence of any benign or malignant ovarian pathology as ruled out by clinical examination and relevant investigations. Cytohistopathologically confirmed and newly diagnosed cases of EOC and benign ovarian cancer were included in this study. The median value of fasting serum insulin was significantly high (15.0 µlU/ml, P = 0.02) and adiponectin were significantly low (5.1 µg/ml, P < 0.001) in ovarian cancer patients compared to benign ovarian tumors and healthy controls group. A significant increase risk of ovarian cancer was found in high tertile (≥ 18.7 µlU/ml) of serum insulin level (OR = 2.7; 95% CI = 1.00–6.67, P = 0.04) and lower tertile (≤ 5.45 µg/ml) of adiponectin level (OR = 3.2; 95% CI = 1.10–9.71, P = 0.03). High serum insulin level and low adiponectin levels were significantly associated with increased risk for development of ovarian cancer.


Similar content being viewed by others
References
NCRP Report. Three year report of population based cancer registries 2012–14. National cancer registry program, Indian Council of Medical Research 2016
Marth C, Reimer D, Zeimet AG. Front-line therapy of advanced epithelial ovarian cancer: standard treatment. Ann Oncol. 2017;28:viii36–viii39.
Peres LC, Cushing-Haugen KL, Kobel M, Harris HR, Berchuck A, Rossing MA, et al. Invasive epithelial ovarian cancer survival by histotype and disease stage. J Natl Cancer Inst. 2019;111:60–8.
Matulonis UA, Sood AK, Fallowfield L, Howitt BE, Sehouli J, Karlan BY. Ovarian cancer. Nat Rev Dis Primers. 2016;2:16061.
Zhan Q, Wang C, Ngai S. Ovarian cancer stem cells: a new target for cancer therapy. Biomed Res Int. 2013;2013:916819.
Siegel RL, Miller KD, Jemal A. Cancer statistics. CA Cancer J Clin. 2019;69:7–34.
Momenimovahed Z, Tiznobaik A, Taheri S, Salehiniya H. Ovarian cancer in the world: epidemiology and risk factors. Int J Womens Health. 2019;11:287–99.
Booth A, Magnuson A, Fouts J, Foster M. Adipose tissue, obesity and adipokines: role in cancer promotion. Horm Mol Biol Clin Investig. 2015;21:57–74.
Tworoger SS, Huang T. Obesity and ovarian cancer. Recent Results Cancer Res. 2016;208:155–76.
Katira A, Tan PH. Evolving role of adiponectin in cancer-controversies and update. Cancer Biol Med. 2016;13:101–19.
Di Zazzo E, Polito R, Bartollino S, Nigro E, Porcile C, Bianco A, et al. Adiponectin as link factor between adipose tissue and cancer. Int J Mol Sci. 2019;20:E839.
Xu HL, Fang H, Xu WH, Qin GY, Yan YJ, Yao BD, et al. Cancer incidence in patients with type 2 diabetes mellitus: a population-based cohort study in Shanghai. BMC Cancer. 2015;15:852.
Gallagher EJ, LeRoith D. Obesity and diabetes: the increased risk of cancer and cancer-related mortality. Physiol Rev. 2015;95:727–48.
Joung KH, Jeong JW, Ku BJ. The association between type 2 diabetes mellitus and women cancer: the epidemiological evidences and putative mechanisms. Biomed Res Int. 2015;2015:920618.
Grayson K, Gregory E, Khan G, Guinn BA. Urine biomarkers for the early detection of ovarian cancer—are we there yet? Biomark Cancer. 2019;11:1179299X19830977.
Chandra A, Pius C, Nabeel M, Nair M, Vishwanatha JK, Ahmad S, et al. Ovarian cancer: current status and strategies for improving therapeutic outcomes. Cancer Med. 2019;8:7018–31.
Dupont J, Scaramuzzi RJ. Insulin signalling and glucose transport in the ovary and ovarian function during the ovarian cycle. Biochem J. 2016;473:1483–501.
Kong L, Wang Q, Jin J, Xiang Z, Chen T, Shen S, et al. Insulin resistance enhances the mitogen-activated protein kinase signaling pathway in ovarian granulosa cells. PLoS ONE. 2017;12:e0188029.
Das D, Arur S. Conserved insulin signaling in the regulation of oocyte growth, development, and maturation. Mol Reprod Dev. 2017;84:444–59.
Stocco C, Baumgarten SC, Armouti M, Fierro MA, Winston NJ, Scoccia B, et al. Genome-wide interactions between FSH and insulin-like growth factors in the regulation of human granulosa cell differentiation. Hum Reprod. 2017;32:905–14.
Giovannucci E, Harlan DM, Archer MC, Bergenstal RM, Gapstur SM, Habel LA, et al. Diabetes and cancer: a consensus report. Diabetes Care. 2010;33:1674–85.
Orgel E, Mittelman SD. The links between insulin resistance, diabetes, and cancer. Curr Diabetes Rep. 2013;13:213–22.
Otokozawa S, Tanaka R, Akasaka H, Ito E, Asakura S, Ohnishi H, Saito S, et al. Associations of serum isoflavone, adiponectin and insulin levels with risk for epithelial ovarian cancer: results of a case-control study. Asian Pac J Cancer Prev. 2015;16:4987–91.
Serin IS, Tanriverdi F, Yilmaz MO, Ozcelik B, Unluhizarci K. Serum insulin-like growth factor (IGF)-I, IGF binding protein (IGFBP)-3, leptin concentrations and insulin resistance in benign and malignant epithelial ovarian tumors in postmenopausal women. Gynecol Endocrinol. 2008;24:117–21.
Gelsomino L, Naimo GD, Catalano S, Mauro L, Ando S. The emerging role of adiponectin in female malignancies. Int J Mol Sci. 2019;20:E2127.
Cheaib B, Auguste A, Leary A. The PI3K/Akt/mTOR pathway in ovarian cancer: therapeutic opportunities and challenges. Chin J Cancer. 2015;34:4–16.
Savant SS, Sriramkumar S, O'Hagan HM. The role of inflammation and inflammatory mediators in the development, progression, metastasis, and chemoresistance of epithelial ovarian cancer. Cancers (Basel). 2018;10:E251.
Grossmann ME, Cleary MP. The balance between leptin and adiponectin in the control of carcinogenesis-focus on mammary tumorigenesis. Biochimie. 2012;94:2164–71.
Ruan H, Dong LQ. Adiponectin signaling and function in insulin target tissues. J Mol Cell Biol. 2016;8:101–9.
Jin JH, Kim HJ, Kim CY, Kim YH, Ju W, Kim SC. Association of plasma adiponectin and leptin levels with the development and progression of ovarian cancer. Obstet Gynecol Sci. 2016;59:279–85.
Acknowledgements
We are thankful to members of ethical committee, Maulana Azad Medical College, New Delhi for giving opportunity to conduct study.
Funding
The authors received no financial support for the research and/or publication of this article.
Author information
Authors and Affiliations
Contributions
RKG designed research, collection and analysis of data, clinical monitoring and laboratory detection and reviewed the manuscript; SJD performed collection and analysis of data and helped in manuscript preparation. SK, SKG, RT and SLJ helped in discussion, designing research strategies and crafting the manuscript. All authors reviewed and edited the manuscript and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Authors declare that there is no conflict of interest.
Ethics Approval
Study has been approved by ethical committee of Maulana Azad Medical College, New Delhi and hospital based case–control study has been performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments.
Informed Consent
Informed consent was taken from all participants.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gupta, R.K., Dholariya, S.J., Kaushik, S. et al. Hyperinsulinemia and Hypoadiponectinemia are Associated with Increased Risk for Occurrence of Ovarian Cancer in Non-diabetic Women of North Indian Population. Ind J Clin Biochem 36, 221–227 (2021). https://doi.org/10.1007/s12291-020-00891-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12291-020-00891-9