Abstract
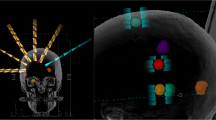
To compare the dosimetric parameters of automated noncoplanar volumetric modulated arc therapy plans using single-isocentric (SIC) and multi-isocentric (MIC) techniques for patients with two brain metastases (BMs) in stereotactic irradiation and to evaluate the robustness of rotational errors. The SIC and MIC plans were retrospectively generated (35 Gy/five fractions) for 58 patients. Subsequently, a receiver operating characteristic curve analysis between the tumor surface distance (TSD) and V25Gy was performed to determine the thresholds for the brain tissue. The SIC and MIC plans were recalculated based on the rotational images to evaluate the dosimetric impact of rotational error. The MIC plans showed better brain tissue sparing for TSD > 6.6 cm. The SIC plans provided a significantly better conformity index for TSD ≤ 6.6 cm, while significantly lower gradient index was obtained (3.22 ± 0.56vs. 3.30 ± 0.57, p < 0.05) in the MIC plans with TSD > 6.6 cm. For organs at risk (OARs) (brainstem, chiasm, lens, optic nerves, and retinas), D0.1 cc was significantly lower (p < 0.05) in the MIC plans than in the SIC plans. The prescription dose could be delivered (D99%) to the gross tumor volume (GTV) for patients with TSD ≤ 6.6 cm when the rotational error was < 1°, whereas 31% of the D99% of GTV fell below the prescription dose with TSD > 6.6 cm. MIC plans can be an optimal approach for reducing doses to OARs and providing robustness against rotational errors in BMs with TSD > 6.6 cm.





Similar content being viewed by others
References
Soffietti R, Ruda R, Mutani R. Management of brain metastases. J Neurol. 2002;249(10):1357–69.
Chang EL, Wefel JS, Hess KR, et al. Neurocognition in patients with brain metastases treated with radiosurgery or radiosurgery plus whole-brain irradiation: a randomised controlled trial. Lancet Oncol. 2009;10(11):1037–44.
Coffey RJ, Flickinger JC, Bissonette DJ, et al. Radiosurgery for solitary brain metastases using the cobalt-60 gamma unit: methods and results in 24 patients. Int J Radiat Oncol Biol Phys. 1991;20(6):1287–95.
Shiau C-Y, Sneed PK, Shu H-KG, et al. Radiosurgery for brain metastases: relationship of dose and pattern of enhancement to local control. Int J Radiat Oncol Biol Phys. 1997;37(2):375–83.
Dupic G, Brun L, Molnar I, et al. Significant correlation between gross tumor volume (GTV) D98% and local control in multifraction stereotactic radiotherapy (MF-SRT) for unresected brain metastases. Radiother Oncol. 2021;154:260–8.
Kraft J, van Timmeren JE, Mayinger M, et al. Distance to isocenter is not associated with an increased risk for local failure in LINAC-based single-isocenter SRS or SRT for multiple brain metastases. Radiother Oncol. 2021;159:168–75.
Vergalasova I, Liu H, Alonso-Basanta M, et al. Multi-institutional dosimetric evaluation of modern day stereotactic radiosurgery (SRS) treatment options for multiple brain metastases. Front Oncol. 2019;9:483.
Uematsu M, Fukui T, Shioda A, et al. A dual computed tomography linear accelerator unit for stereotactic radiation therapy: a new approach without cranially fixated stereotactic frames. Int J Radiat Oncol Biol Phys. 1996;35(3):587–92.
Milano MT, Grimm J, Niemierko A, et al. Single- and multifraction stereotactic radiosurgery dose/volume tolerances of the brain. Int J Radiat Oncol Biol Phys. 2021;110(1):68–86.
Minniti G, Scaringi C, Paolini S, et al. Single-fraction versus multifraction (3 × 9 Gy) stereotactic radiosurgery for large (> 2 cm) brain metastases: a comparative analysis of local control and risk of radiation-induced brain necrosis. Int J Radiat Oncol Biol Phys. 2016;95(4):1142–8.
Komiyama R, Ohira S, Ueda H, et al. Intra-fractional patient motion when using the Qfix Encompass immobilization system during HyperArc treatment of patients with brain metastases. J Appl Clin Med Phys. 2021;22(3):254–60.
Parikh NR, Kundu P, Levin-Epstein R, et al. Time-driven activity-based costing comparison of stereotactic radiosurgery to multiple brain lesions using single-isocenter versus multiple-isocenter technique. Int J Radiat Oncol Biol Phys. 2020;108(4):999–1007.
Andruska N, Kennedy WR, Bonestroo L, et al. Dosimetric predictors of symptomatic radiation necrosis after five-fraction radiosurgery for brain metastases. Radiother Oncol. 2021;156:181–7.
Xu Y, Ma P, Xu Y, et al. Selection of prescription isodose line for brain metastases treated with volumetric modulated arc radiotherapy. J Appl Clin Med Phys. 2019;20(12):63–9.
Sagawa T, Ohira S, Ueda Y, et al. Dosimetric effect of rotational setup errors in stereotactic radiosurgery with HyperArc for single and multiple brain metastases. J Appl Clin Med Phys. 2019;20(10):84–91.
Nakano H, Tanabe S, Yamada T, et al. Maximum distance in single-isocenter technique of stereotactic radiosurgery with rotational error using margin-based analysis. Radiol Phys Technol. 2021;14(1):57–63.
Borges C, Zarza-Moreno M, Heath E, et al. Monte Carlo modeling and simulations of the High Definition (HD120) micro MLC and validation against measurements for a 6 MV beam. Med Phys. 2012;39(1):415–23.
Shaw E, Kline R, Gillin M, et al. Radiation therapy oncology group: Radiosurgery quality assurance guidelines. Int J Radiat Oncol Biol Phys. 1993;27(5):1231–9.
Paddick I. A simple scoring ratio to index the conformity of radiosurgical treatment plans. Technical note. J Neurosurg. 2000;93(Suppl 3):219–22.
Kubo K, Kenjo M, Doi Y, et al. MRI appearance change during stereotactic radiotherapy for large brain metastases and importance of treatment plan modification during treatment period. Jpn J Radiol. 2019;37(12):850–9.
Inoue HK, Seto K, Nozaki A, et al. Three-fraction CyberKnife radiotherapy for brain metastases in critical areas: referring to the risk evaluating radiation necrosis and the surrounding brain volumes circumscribed with a single dose equivalence of 14 Gy (V14). J Radiat Res. 2013;54(4):727–35.
Park HS, Wang EH, Rutter CE, et al. Changing practice patterns of Gamma Knife versus linear accelerator-based stereotactic radiosurgery for brain metastases in the US. J Neurosurg. 2016;124(4):1018–24.
Gevaert T, Steenbeke F, Pellegri L, et al. Evaluation of a dedicated brain metastases treatment planning optimization for radiosurgery: a new treatment paradigm? Radiat Oncol. 2016;11:13.
Amaya D, Shinde A, Wohlers C, et al. Dosimetric comparison of multiple vs single isocenter technique for linear accelerator-based stereotactic radiosurgery: the importance of the six degree couch. J Appl Clin Med Phys. 2021;22(6):45–9.
Ohira S, Ueda Y, Kanayama N, et al. Impact of multileaf collimator width on dose distribution in HyperArc fractionated stereotactic irradiation for multiple (5–10) brain metastases. Anticancer Res. 2021;41(6):3153–9.
Kielar KN, Mok E, Hsu A, et al. Verification of dosimetric accuracy on the TrueBeam STx: rounded leaf effect of the high definition MLC. Med Phys. 2012;39(10):6360–71.
Jang SY, Vassiliev ON, Liu HH, et al. Development and commissioning of a multileaf collimator model in Monte Carlo dose calculations for intensity-modulated radiation therapy. Med Phys. 2006;33(3):770–81.
Roper J, Chanyavanich V, Betzel G, et al. Single-isocenter multiple-target stereotactic radiosurgery: risk of compromised coverage. Int J Radiat Oncol Biol Phys. 2015;93(3):540–6.
Prentou G, Pappas EP, Logothetis A, et al. Dosimetric impact of rotational errors on the quality of VMAT-SRS for multiple brain metastases: comparison between single- and two-isocenter treatment planning techniques. J Appl Clin Med Phys. 2020;21(3):32–44.
Ohira S, Ueda Y, Akino Y, et al. HyperArc VMAT planning for single and multiple brain metastases stereotactic radiosurgery: a new treatment planning approach. Radiat Oncol. 2018;13(1):13.
Ruggieri R, Naccarato S, Mazzola R, et al. Linac-based VMAT radiosurgery for multiple brain lesions: comparison between a conventional multi-isocenter approach and a new dedicated mono-isocenter technique. Radiat Oncol. 2018;13(1):38.
Hartgerink D, Swinnen A, Roberge D, et al. LINAC based stereotactic radiosurgery for multiple brain metastases: guidance for clinical implementation. Acta Oncol. 2019;58(9):1275–82.
Garsa AA, Badiyan SN, DeWees T, et al. Predictors of individual tumor local control after stereotactic radiosurgery for non-small cell lung cancer brain metastases. Int J Radiat Oncol Biol Phys. 2014;90(2):407–13.
Ohira S, Kanayama N, Komiyama R, et al. Intra-fractional patient setup error during fractionated intracranial stereotactic irradiation treatment of patients wearing medical masks: comparison with and without bite block during COVID-19 pandemic. J Radiat Res. 2021;62(1):163–71.
Tryggestad E, Christian M, Ford E, et al. Inter- and intrafraction patient positioning uncertainties for intracranial radiotherapy: a study of four frameless, thermoplastic mask-based immobilization strategies using daily cone-beam CT. Int J Radiat Oncol Biol Phys. 2011;80(1):281–90.
Tsui SSW, Wu VWC, Cheung JSC. Comparison of dosimetric impact of intra-fractional setup discrepancy between multiple- and single-isocenter approaches in LINAC-based stereotactic radiotherapy of multiple brain metastases. J Appl Clin Med Phys. 2022;23(2): e13484.
Cui T, Zhou Y, Yue NJ, et al. Optimization of treatment isocenter location in single-isocenter LINAC-based stereotactic radiosurgery for management of multiple brain metastases. Med Phys. 2021;48(12):7632–40.
Kirkpatrick JP, Wang Z, Sampson JH, et al. Defining the optimal planning target volume in image-guided stereotactic radiosurgery of brain metastases: results of a randomized trial. Int J Radiat Oncol Biol Phys. 2015;91(1):100–8.
Tanaka Y, Oita M, Inomata S, et al. Impact of patient positioning uncertainty in noncoplanar intracranial stereotactic radiotherapy. J Appl Clin Med Phys. 2020;21(2):89–97.
Covington EL, Fiveash JB, Wu X, et al. Optical surface guidance for submillimeter monitoring of patient position during frameless stereotactic radiotherapy. J Appl Clin Med Phys. 2019;20(6):91–8.
Tomihara J, Takatsu J, Sugimoto S, et al. Intrafraction stability using full head mask for brain stereotactic radiotherapy. J Appl Clin Med Phys. 2021;22(9):360–70.
Funding
This study was supported by JSPS KAKENHI Grant (Grant-in-Aid for Scientific Research (C) 21K07742).
Author information
Authors and Affiliations
Contributions
All the authors participated in the writing this article and take responsibility for its content. The authors confirm that the content of the manuscript has not been published, or submitted for publication elsewhere.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare in relation to this study.
Ethics approval
This study was approved by the ethics committee of our institution.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Yamamoto, Y., Ohira, S., Kanayama, N. et al. Comparison of dosimetric parameters and robustness for rotational errors in fractionated stereotactic irradiation using automated noncoplanar volumetric modulated arc therapy for patients with brain metastases: single- versus multi-isocentric technique. Radiol Phys Technol 16, 310–318 (2023). https://doi.org/10.1007/s12194-023-00720-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12194-023-00720-7